Use of the O-Z flap as an alternative to free tissue transfer for reconstruction of large scalp defects
Abstract
Objective
The reconstruction of large scalp defects poses both functional and cosmetic challenges. While free tissue transfer remains the standard for defects larger than 30 cm2, prolonged anesthesia and postoperative complications remain significant limitations. The purpose of this study is to evaluate the use of O-Z flaps for the reconstruction of large scalp defects and to describe the techniques employed.
Methods
This is a retrospective analysis of ten patients who underwent reconstructive surgery using an O-Z flap approach for large scalp defects between July 2017 and June 2019. The parameters included in this study were patient demographics, tumor characteristics, and postoperative management, collected for at least a year after surgery.
Results
In this cohort, the mean age was 76.1 years and 90% were male. All patients were treated for neoplastic skin lesions, with 70% located on the vertex and 30% located on the temporoparietal region. The mean size of defect was 52.0 cm2 (range: 38.6 to 63.8 cm2). The maximum hospital stay was two days, and no patients were readmitted within 30 days of surgery. There were no cases of wound infection or flap necrosis. All patients reported pain control with acetaminophen and ibuprofen. Four patients received adjuvant radiation, and there was no delay to receiving treatment following surgery.
Conclusions
The O-Z flap is a reliable alternative for the reconstruction of non-irradiated scalp defects in the vertex and temporoparietal regions up to 63 cm2. This technique provides advantages for patients, including hairline preservation, shorter hospital stays, and decreased postoperative complications.
INTRODUCTION
Reconstruction of scalp defects requires consideration of functional goals like vascularization and protection of the calvarium, and aesthetic goals related to the location of incisions and reduction of hairline distortion.1, 2 The limited laxity and unique cosmetic demands of the scalp pose many challenges for the reconstructive surgeon, and the proximity of defects to facial features and hair bearing areas can invariably change the approach to the surgery.3 The reconstructive ladder describes the increasing complexity of techniques that a surgeon may consider when repairing a defect, mostly dependent on the size and location of the defect and the patient's comorbidities. The primary tenet of the reconstructive ladder is to use the least complex technique to meet the functional and aesthetic goals of the procedure. These surgical approaches include direct primary closure, skin grafts and dermal regeneration templates, local advancement and rotation flaps, and free flaps.
The size and location of lesions are usually the first considerations for determining the necessity of more complex approaches to scalp repair. For small defects less than 3 cm in diameter and without hairline involvement, direct primary closure is the preferred approach due to its simplicity and minimal rate of complications.4 To ensure a tension-free closure, galeal-releasing incisions placed parallel to the incision may be considered. Split-thickness and full-thickness skin grafts are uncommonly utilized and limited to non-hair-bearing areas or large defects that cannot be entirely covered with direct primary closure or a flap. The use of skin substrates like dermal regeneration templates (Integra) or acellular human dermis (AlloDerm) show promising results and may be utilized in bone-exposed areas; however, they often require coverage with a skin graft and have relatively high cost compared to autografts.5, 6
Local flaps are the gold standard for small and medium-sized defects in non-irradiated patients, including rotation, advancement, and transposition flaps. The most common techniques are the pinwheel flap, the O-Z flap, and the Orticochea flap.7, 8 Tissue expansion may be considered to increase skin coverage, epidermal thickness, and blood flow to the flap.1 Generally, local flap procedures have complication rates as low as 3.4% for small and medium-sized defects.9
The reconstruction of large-sized defects, often following tumor resection, remains a technical challenge. One algorithm outlines that local flaps should be considered for defects with a diameter less than 6-8 cm or at the hairline with a diameter less than 4-5 cm, with free tissue transfer or skin grafts necessary for any larger, full-depth defects.10 Due to limited laxity of the scalp, which can be worsened by prior radiation and infection, free flaps are the current recommendation for reconstruction of scalp defects larger than 25-50 cm2, as they bring reliable vascularized tissue with bulk.1, 9, 11 However, the downsides of free flap reconstruction are non-hair-bearing skin, graft site morbidity, increased complexity of surgery, and increased length of surgery equating to increased risk from anesthesia. Free flap procedures also typically require a minimum of 3 days of postoperative admission and have higher complication rates requiring revision surgery.3 For patients with health comorbidities or inability to tolerate prolonged general anesthesia, these factors play a significant role in the decision-making for performing a free flap.12
In the current study, we present a case series of patients who had undergone the use of a 2-flap rotation flap (O-Z flap) without tissue expansion or skin grafting for the reconstruction of large scalp defects, for which free flap reconstruction is often considered. We evaluate patient outcomes and describe techniques employed to achieve an optimal outcome following tumor resection.
METHODS
This was a retrospective case series approved by the institutional review board at the University of Pennsylvania. We performed a chart review of patients with large-sized scalp defects who underwent reconstructive surgery by the senior author between July 2017 and June 2019. Patients were included if they had scalp defects larger than 6 cm in diameter (approximately 30 cm2) for which an O-Z flap reconstruction was performed. Patients were excluded if they had a history of scalp radiation treatment or prior scalp surgery with nonhealing wounds, or if minimal skin laxity was noted on physical exam.
We begin our O-Z flap design by drawing an outer border defining the proposed bases for the flaps. This border is typically 3-4 times the radius of the defect and should have adequate margins to expand the incisions if needed (Figure 1). When possible, the incisions are designed parallel to the lines of minimum tension. Incisions should also parallel the directional orientation of hair in order to avoid hair follicle transection. These tend to be oriented longitudinally on the top of the scalp and horizontally in the lower part of the occiput. The scalp has a rich vascular supply due to contribution from five arteries, including the superficial temporal, posterior auricular, occipital, supraorbital, and supratrochlear arteries.13 The incisions are designed such that at least one major branch is present in each flap, with preference for the superficial temporal and occipital arteries.
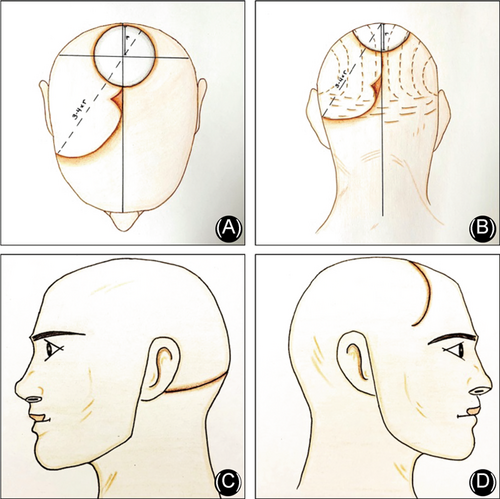
The flaps are widely undermined in a subgaleal plane, which is usually performed from root of one ear to root of the contralateral ear in the horizontal direction, and from brow to nuchal ridge in the anterior-posterior direction. The large flap design, coupled with wide undermining dramatically improves the laxity and mobility of the flaps, which is necessary for a minimal-tension closure (Figure 2). Scoring of the galeal layer perpendicular to the direction of flap advancement can also be performed to relieve tension and enhance advancement. The blood supply to the scalp is cutaneous, meaning that the vessels enter from the periphery and run medially in the subcutaneous tissues. Therefore, as long as the dissection is confined to the subgaleal plane, the blood supply to the tissues should not be compromised.14 Once the flaps are rotated to cover the resected area with minimal tension, the wounds edges are approximated and closed. A subgaleal 10 flat Jackson Pratt drain was routinely placed prior to closure.
The parameters evaluated in this study included patient age, gender, pathologic diagnosis, prior scalp surgery, smoking status, diabetes, depth, size, and location of defect, length of hospitalization, postoperative complications, and need for adjuvant radiation. Follow up data were collected for a minimum of 1 year after surgery. Demographic and follow-up data was summarized using descriptive statistics.
RESULTS
A total of 10 patients met inclusion criteria for the study. The mean age was 76.1 years (range: 65 to 88 years), including nine males and one female (Table 1). All patients were being treated for neoplastic skin lesions, including squamous cell carcinoma, melanoma, angiosarcoma, and dermatofibrosarcoma protuberans (Table 2). The mean surface area of the defects was 52.0 cm2 (range: 38.6 to 63.8 cm2). Nine patients had defects that extended down to the calvarium. One patient required preoperative imaging due to concern for dural involvement on physical exam, which was confirmed with computed tomography (CT) of the head. All patients had defects located on the vertex or temporoparietal regions of the scalp. The mean number of prior scalp surgeries was 1.9 (range: 0-4), and four patients also received adjuvant radiation (Table 1) due to high-risk pathology.
| Characteristic | Number | Percentage |
|---|---|---|
| Total | 10 | 100% |
| Gender | ||
| Male | 9 | 90% |
| Female | 1 | 10% |
| Mean age (Year) | 76.1 (SD = 7.3) | |
| Mean prior scalp surgeries | 1.9 (SD = 1.2) | |
| Associated factors | ||
| Prior scalp surgery | 9 | 90% |
| Current smoker | 0 | 0 |
| Diabetes | 3 | 30% |
| Adjuvant radiation | 4 | 40% |
| Characteristic | Number | Percentage |
|---|---|---|
| Tumor pathology | ||
| Squamous cell carcinoma | 4 | 40% |
| Melanoma | 4 | 40% |
| Angiosarcoma | 1 | 10% |
| Dermatofibrosarcoma protuberans | 1 | 10% |
| Mean size of defect (cm2) | 52.0 (SD = 9.0) | |
| Location of defect | ||
| Vertex | 7 | 70% |
| Temporoparietal | 3 | 30% |
| Depth of defect | ||
| Down to calvarium | 9 | 90% |
| Down to dura | 1 | 10% |
All patients underwent a single stage resection and O-Z flap reconstruction with two rotational flaps without tissue expansion (Figure 1). Neck dissection was not indicated for any of the patients. The maximum length of hospital stay was two days, with 80% of patients being discharged on the day of surgery. Patients were seen on a biweekly schedule for the first eight weeks and then every three months as part of standard oncologic surveillance. All patients had mean total follow up duration of 501 days (range: 370-821 days). All patients were managed in the outpatient setting with local wound care, consisting of the application of over-the-counter petroleum-based ointment such as Aquaphor or Vaseline and serial wound debridement in the office. All patients reported adequate pain control with acetaminophen and ibuprofen, and none of the patients required opioid pain medications. There were no cases of wound infection, flap necrosis, or positive margins, and no patients required revision surgery. None of the patients were readmitted within 30 days of the operation for related or unrelated conditions. Four patients receiving adjuvant radiation and there were no delays to receiving treatment. Additionally, none of these patients had any wound complications or signs of osteoradionecrosis of the scalp following radiation treatment.
DISCUSSION
Due to an increasing prevalence of cutaneous neoplasms in the United States, there is an increased focus on reconstructive techniques for skin defects, particularly in cosmetically-sensitive areas like the head and neck.15 Current reconstructive algorithms recommend that defects larger than 30 cm2 be repaired with free tissue transfer alone or the addition of skin grafts to a local flap.1, 3, 10, 12, 16, 17 To our knowledge, this is the largest case series that demonstrates the use of O-Z flaps for the reconstruction of scalp defects as large as 63 cm2 following tumor resection.
The basic goals of designing local flaps include reducing the number of flaps used, using wide bases to distribute wound closure tension over a larger area, and placing incisions that can be hidden in hair-bearing areas.18 Of the different patterns available for local flap construction, rotational flaps are the most practical and effective for operating in the spherical confines of the scalp and achieving the above-mentioned goals.19 Large defects in the vertex and temporoparietal regions are best suited for O-Z flaps since a large area is available for flap design. Patients with a history of preoperative scalp radiation or chemotherapy are not good candidates for local reconstruction due to the presence of significant skin fibrosis, which limits the ability to mobilize tissue for coverage of a defect.9
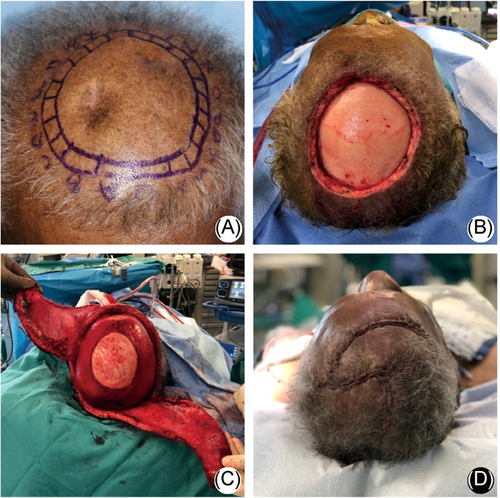
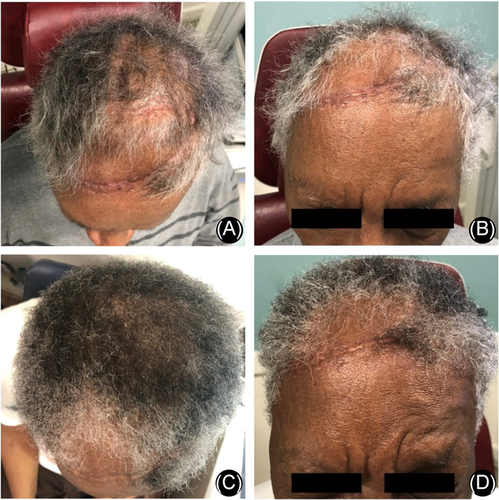
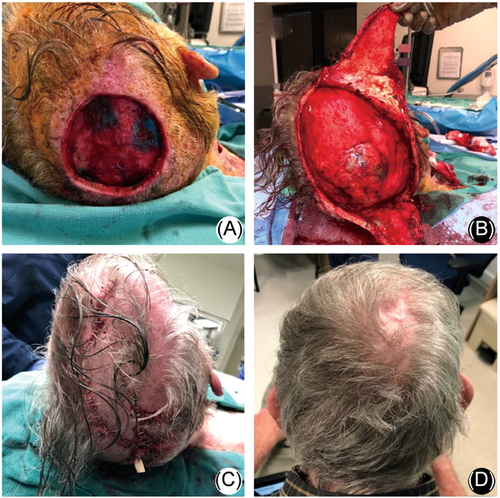
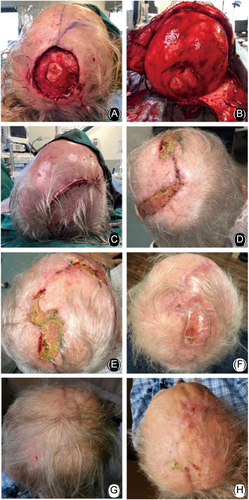
Postoperatively, patients can be sent home with a drain if they are able to provide proper care. In our series, two patients felt more comfortable staying in the hospital for two days until drain removal, while the remaining eight patients were discharged home on the same day. All patients were advised to take acetaminophen and ibuprofen for pain. No patients required narcotic pain medication. Patients were typically seen every two weeks after surgery, but this time frame can be extended for patients who are able to care for the wound themselves. The wounds were evaluated in the office and areas with significant crusting were debrided. All incisions were completely healed by 6-8 weeks, and postoperative images for one patient are shown in Figure 3. Images for the reconstruction and wound healing of a different large scalp defect are shown in Figure 4. In our series, four patients required adjuvant radiation therapy due to tumor characteristics (three had defects to the depth of the calvarium, and one requiring a craniectomy with exposure of the dura). Microvascular reconstruction can result in a delay to radiation treatment if there is flap failure or partial necrosis, and delays longer than 6 weeks are associated with decreased overall survival.20 Our reconstructive surgery did not delay the start of radiation therapy for these patients, and none had wound complications following completion of radiation treatment. The progression of wound healing for one of the patients that received adjuvant chemoradiation is shown in Figure 5.
The benefits of the O-Z flap are due to use of tissue identical to the defect in terms of thickness, texture, and hair-bearing status, resulting in preferable cosmetic results. Compared to free tissue transfer options, we found this technique offers the advantages of reduced postoperative hospitalization, minimal postoperative pain controlled with over-the-counter pain medications alone, ease of wound care in the outpatient setting, and reduced risk of 30-day readmission or revision surgery. In particular, for large defects in high-risk patients with comorbid conditions or unable to tolerate a long period of general anesthesia, the O-Z flap reconstruction may be considered over free tissue transfer.
Another surgical option seeing increased popularity is the dermal regeneration template (Integra) for repair of large, full-thickness defects.21 A cost analysis for reconstuction of scalp defects with bone exposure determined that the median total cost per patient was approximately $12,000 for Integra compared to $8,000 for flap reconstruction (including 14 pedicled flaps and 3 free flaps).5 However, the use of dermal regeneration templates in defects larger than 100 cm2 showed a significantly decreased length of hospital stay and overall cost to patients when compared to free flaps.5, 6 One series reported that post-operative radiation to the Integra site led to partial breakdown of the reconstruction after 2 years in one patient, and the authors concluded that they would not advocate routine radiation therapy to the skin grafted Integra site.22 Alternatively, a separate study reported the theoretical benefit of Integra reconstruction allowing for immediate radiotherapy.23 Limitations for Integra include susceptibility to infection, availability, and requirement for a second procedure for coverage of the matrix with a split-thickness skin graft 4-6 weeks later. For reconstruction of small and medium-sized defects smaller than 63 cm2, we would currently prefer a local flap approach to optimize cosmetic results, reduce donor site morbidity, and reduce the number of procedures. Further work on single-stage Integra reconstruction with skin grafting during the same procedure may further augment the usefulness of dermal regeneration templates in the future.24
Skin quality is the primary consideration for determining whether a patient can undergo a local scalp reconstruction since flaps must have a significant degree of mobility to fill a large defect. In general, we prefer not to use pre-operative tissue expansion due to its risk for complications including infection, extrusion, dermal thinning, pre-operative deformity, need for serial expansion, potential delay in management of neoplastic processes, and need for multiple operations. The most common causes of reduced skin laxity in our patients are prior scalp surgery and scalp irradiation. Prior scalp surgeries are not a definitive contraindication unless significant wound contracture or nonhealing wounds are present in the flap area. In our case series, a majority of patients had undergone multiple prior scalp surgeries which did not present as an impediment to surgery. However, prior radiation treatments remains a significant barrier to the local flap approach, as radiation-induced fibrosis reduces flap mobility and makes covering larger scalp defects more difficult. Due to the limited scalp area that can be used for flap design, free tissue transfer is the gold-standard for patients with minimal skin laxity or skin defects larger than 63 cm2.
No randomized trials exist in the literature for comparing the effectiveness of local flap and free flap approaches for large scalp defects. Some recent case reports have demonstrated the use of the Orticochea flap for large frontal or vertex scalp defects.16, 17 Given the various factors that contribute to outcomes with different reconstructive techniques, further studies are required to understand the independent risks and optimize the selection criteria for these approaches.
CONCLUSIONS
Large-sized scalp defects continue to present a reconstructive challenge for surgeons following tumor resection. While microvascular free tissue transfer remains the standard for many of these defects, increased morbidity due to donor-site complications and prolonged anesthesia is a barrier for many patients. In this case series, we argue that the O-Z flap is a reliable alternative approach for the reconstruction of large scalp defects up to 63 cm2 in the vertex and temporoparietal regions of patients without a history of scalp radiation. This technique provides significant advantages for patients, including improved hairline preservation, reduced need for pain medications, and shorter hospital stays.
-
Edited by Qiong Wu
CONFLICTS OF INTEREST
Informed consent was obtained for publication of photographs.
CONSENT TO PARTICIPATE
The authors declare no conflicts of interest.