A case of cutaneous malignant fibrous histiocytoma with multiple organ metastases
Abstract
Malignant fibrous histiocytoma is a soft tissue sarcoma that most commonly occurs in the extremities and rarely metastasizes cutaneously. A 79-year-old male patient consulted a dermatologist 11 months after recognizing an intractable ulcer on the right mandible. Punch biopsy revealed eosinophilic tumor cells in the dermal area and proliferation of rich spindle cells. Malignant fibrous histiocytoma or atypical fibroxanthoma was suspected and he was referred to our hospital. Red plaque tumors on the right mandible and right temple were 30 mm and 15 mm in size, respectively. The right mandible lesion was ulcerated. Immunohistochemically, the lesions were positive for CD10, CD74 and alpha-smooth muscle actin. Radiological analysis revealed multiple organ metastases, including bone, liver, lung and skin on the right temple. The patient was diagnosed with malignant fibrous histiocytoma, stage IV and died 8 weeks after the first visit due to respiratory failure. Cutaneous malignant fibrous histiocytoma has a poor prognosis resulting in death.
Introduction
We report a case of cutaneous MFH on the right mandible with multiple metastases to the skin on the right temple and other organs.
Case report
A 79-year-old male patient with a history of schizophrenia and Parkinson's disease presenting with tumors on his right mandible and right temple was referred to our hospital (Fig. 1A). The patient had recognized an intractable ulcer on the right mandible 12 months before consulting us. He consulted an orthopedic surgeon for his lumbago 5 months prior to consulting us. Magnetic resonance and bone scintigraphy showed space-occupying lesions on the third and fourth vertebrae and on the left humerus (Fig. 2A and B). Computed tomography-guided aspiration cytodiagnosis was conducted, but the specimen comprised a hematoma and no atypical cells were found. The patient refused another cytodiagnosis. He had noticed a tumor on the right temple 3 months before consulting us and had visited a local dermatologist. A skin biopsy of the intractable ulcer on the right mandible was performed and histology revealed that the tumor was either an MFH or an atypical fibroxanthoma (AFX). The patient was then referred to us.

The tumors on the right mandible and right temple on the first day of consultation. (A) The largest diameter of the tumors was 30 mm on the right mandible and 15 mm on the right temple. (B) The tumor on the right temple was a red nodule. (C) The tumor on the right mandible consisted of a nodule on the outer edge and an ulcer in the middle. (D) The dermoscopy of the right temple showed no specific feature other than a brown pigmentation. (E) The dermoscopy of the right mandible showed telangiectasia.
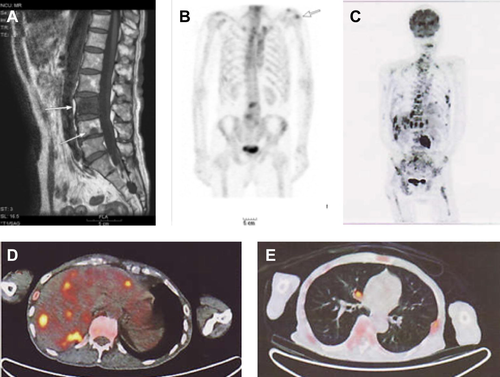
Magnetic resonance imaging (MRI) and bone scintigraphy conducted by the orthopedist 5 months prior to consulting us (A, B) and fluorodeoxyglucose-positron emission tomography images after consulting us (C–E). (A) T1-weighted MRI revealed low signal areas indicating space-occupying lesions on the third and fourth vertebrae (arrows). (B) Bone scintigraphy showed focal accumulation on the left humerus (arrow) as well as the third and fourth vertebrae. (C) Abnormal accumulations were seen in the vertebrae, costae, and other bones of the extremities. (D) Multiple accumulations were observed in the liver. (E) There were abnormal accumulations in both lungs.
At the first visit, the tumor on the right temple appeared as red nodule that was 15 mm at its largest diameter (Fig. 1B). The tumor on the right mandible was 30 mm across at its largest point, and comprised a nodule on the outer edge and an ulcer in the middle (Fig. 1C). Dermoscopy showed no specific features (Fig. 1D–E).
Laboratory testing showed normocytic anemia with a hemoglobin level of 8.4 g/dl and hematocrit of 26.7%. Blood chemistry revealed hypoproteinemia (5.9 g/dl), hypoalbuminemia (2.6 g/dl), high blood urea nitrogen (23.0 mg/dl), elevated lactate dehydrogenase level (459 U/l), and elevated alkaline phosphatase level (801 U/l). The computed tomography image of the head showed that the tumor on the right mandible was 27 × 26 × 25 mm3 in size and the boundary against the right geniohyoid muscle was partially irregular. In the fluorodeoxyglucose positron emission tomography images, abnormal accumulations were seen in the right mandible, the vertebrae, costae, and other bones of the extremities. Multiple accumulations in the liver and both sides of the lungs were also observed (Fig. 2C–E).
Histopathological examination showed ill-defined cellular proliferation of spindle cells with enlarged, pleomorphic nuclei, showing a storiform pattern (Fig. 3A). The mitotic count was high, with each high-power field containing 1–4 mitotic cells and bizarre cells (Fig. 3B). The material was taken as a trephine biopsy specimen and the tumor had invaded the subcutaneous fat (Fig. 3C). Immunohistochemically, tumor cells were positive with CD10, alpha-smooth muscle actin, and CD74 (Fig. 3D–F); it was negative with CD34, CD68, S100, cytokeratins (AE1/AE3), leukocyte common antigen, desmin, caldesmon, and calponin.
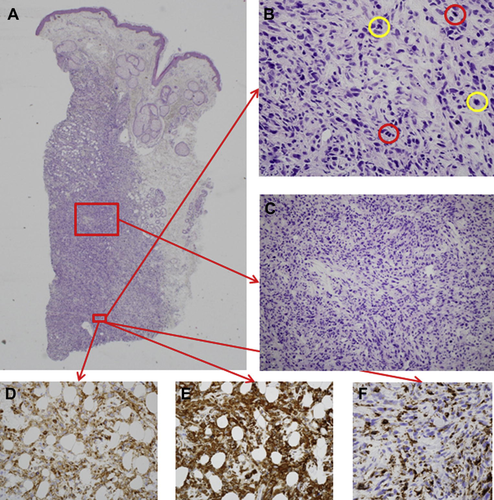
Histopathological examination of the tumor of the right mandible. (A) Proliferation of atypical tumor cells in the dermis. (B) Mitotic count (in the red circle) is high, each high-power filed containing 1–4 mitotic cells and bizarre cells (in the yellow circle). (C) The tumor cells were pleomorphic spindle cells partially arranged in a storiform pattern. (D–F) The tumor cells were positively stained with CD10 (D), alpha-smooth muscle actin (E), and CD74 (F). Hematoxylin and eosin staining; original magnifications ×20 (A), ×400 (B) and ×200 (C); CD10, alpha-SMA, and CD74 immunocytochemistry, original magnification ×400 (D–F)].
We diagnosed the tumor as MFH of the right mandible with multiple organ metastases to lung, liver, bone, and the skin on the right temple. Among the histological subtypes of MFH, the present case was subclassifed as pleomorphic type because the tumor contained no conspicuous giant cells, no myxoid stroma, and no significant inflammatory infiltrate. We explained to the patient that his illness was serious and there was no treatment to improve the prognosis and the patient stated that he did not desire further treatment. He died 8 weeks after the first visit due to respiratory failure while in a nursing home.
Discussion
- • Since all these facts occurred within 1 year, it is more natural to consider that all the lesions originated from the same tumor, rather than that more than two different tumors appeared at the same time.
- • Multiple lesions detected by an orthopedic surgeon 5 months earlier with magnetic resonance imaging had increased by the time the patient came to us. We believe that the metastases from the same origin would have spread.
These clinical findings strongly supported the diagnosis of MFH over AFX.
Immunohistochemistry showed that the present case was positive for CD74. Lazova et al. [5] retrospectively examined 20 MFH cases and 20 AFX cases and reported that 90% of the MFH cases were positive for CD74, whereas 90% of the AFX cases were negative for CD74. It is noteworthy that CD74-positive AFX tends to have a more aggressive behavior [6]. Positivity of CD74 in our case supports the diagnosis of MFH.
Among other differential diagnoses of spindle cell sarcomas, dermatofibrosarcoma protuberans is characteristically CD34 positive, but our case was negative for CD34. Fibrosarcoma is generally less pleomorphic, and sometimes shows a herringbone pattern. Malignant peripheral nerve sheath tumor is often associated with nerves and may show S-100 protein positivity. Leiomyosarcoma is defined as a sarcoma showing more than two of four known markers of smooth muscle differentiation [7], [8]. Our present case only shows positivity on smooth muscle actin, and thus does not satisfy the immunohistochemical criteria for leiomyosarcoma.
The rate of local recurrence for MFH ranges between 19% and 31% and metastasis occurs in 31–35% of patients after the tumor resection. The 5-year survival rate ranges from 65 to 70%. The common sites of metastasis are lung (90%), bone (8%), and liver (1%) [4]. In the present case, we estimated that the primary site was the right mandible, with metastases to the skin of the right temple as well as to the lung, bone and liver. Among the eight reported cases of cutaneous metastases of MFH, only two cases reported duration of survival; one case survived for 2 years and one survived for 10 weeks [3].
For the treatment of cutaneous MFH, it is essential to perform a wide excision of the tumor as early as possible [2]. Adjuvant radiotherapy may be effective in some cases, but the efficacy of chemotherapy remains questionable [1], [9], [10]. For cases with cutaneous metastases, the effect of these treatments is unclear due to the limited number of reported cases [3]. It is important to note that cutaneous MFH with metastases may result in abrupt death of the patient.




