Arrhythmogenic left atrial roof vein
Abstract
A seventy year-old male was referred to our hospital to undergo radiofrequency catheter ablation (RFCA) for drug-refractory paroxysmal atrial fibrillation (AF). Pre-operative three-dimensional computed tomography revealed a unique left atrial (LA) roof vein. Electrophysiological findings showed expansion of the myocardial sleeve and local firing in the LA roof vein. We performed isolation of this arrhythmogenic abnormal vein concomitant with general pulmonary vein isolation in this case, and AF did not recur after the procedure.
1 Introduction
It has been reported that arrhythmogenic local ectopy from pulmonary vein (PV) triggers atrial fibrillation (AF) [1]. Standard strategy of radiofrequency catheter ablation (RFCA) for paroxysmal AF (PAF) is used to perform complete bilateral PV isolation (PVI). However, anatomical diversity in the left atria (LA) and PVs may complicate PVI. We report a case of PAF patient with a large LA roof vein with arrhythmogenic properties, which was successfully isolated with RFCA.
2 Case
A seventy year-old male was referred to our hospital to undergo RFCA for PAF. Pre-performed three-dimensional computed tomography (3D-CT) revealed a relatively large LA roof vein [2], draining to the left side of LA roof (Fig. 1A). The electrophysiological study revealed that the LA roof vein had electrical activity apart from the LA body proven by a local electrogram, which was responsive to local pacing (Fig. 2A). An electro-anatomical mapping system (CARTO3®, Biosense-Webster, Diamond Bar, CA, USA) also demonstrated the electrical activity in the LA roof vein (Fig. 1B and C) recorded by PENTARAY® Nav Catheter (Biosense-Webster, Diamond Bar, CA, USA). The myocardial sleeve with electrical activity could be confirmed about 10 mm from ostium of the LA roof vein. Since 2 μg of isoproterenol repetitively induced local firing only in the roof vein (Fig. 2B), we performed roof vein isolation concomitant with standard bilateral encircling PVI (Fig. 1B and C) by THERMOCOOL® SMARTTOUCH™ (Biosense-Webster, Diamond Bar, CA, USA) with 20–30 W. The LA roof vein was isolated confirmed by local electrogram with PENTARAY® placed into the LA roof vein (Fig. 2D). We also confirmed the precise anatomical location with CARTO3® (Fig. 1B and C). To avoid stenosis of the roof vein by ablation at the vicinity of ostia, linear ablation was successfully performed at the LA adjacent to the roof vein (Fig. 1C white line), followed by disappearance of the electrical activities in the LA roof vein. Afterwards, AF could not be induced by rapid pacing nor high dose of isoproterenol infusion after PV and LA roof vein isolation. The roof vein in this case had a myocardial sleeve and arrhythmogenicity, which required isolation as well as PVs. Currently, AF has not recurred for over 13 months without any anti-arrhythmic drugs.
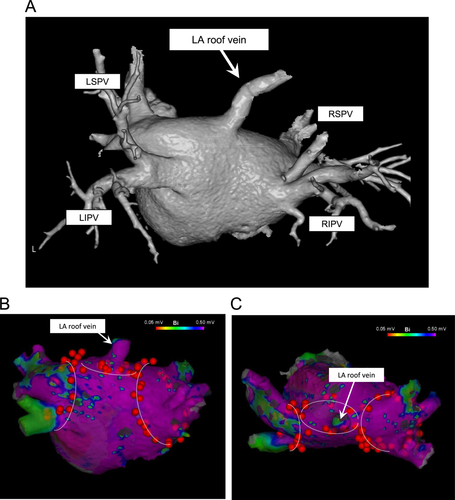
Pre-operative 3D-CT, voltage maps and ablation procedure. A: Three-dimensional computed tomography. Arrowhead indicates unique LA roof vein. B (posterior view) and C (superior view): Voltage mapping in CARTO3® electro-anatomical mapping system revealed electrical activities inside the LA roof vein and showed with ablation tags we performed to isolate the LA roof vein and general bilateral PVI. The added white line indicates the ablation lines we performed. LA: left atria, LSPV: left superior pulmonary vein, LIPV: left inferior pulmonary vein, RSPV: right superior pulmonary vein, RIPV: right inferior pulmonary vein.
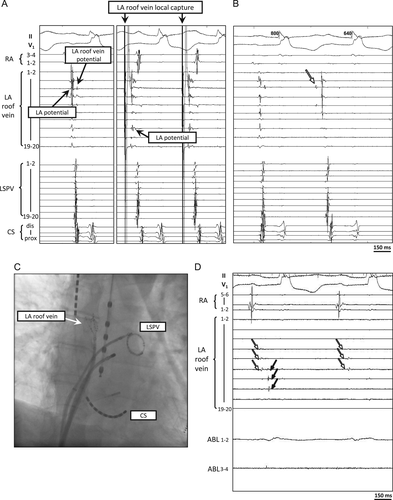
Electrophysiological study revealed electrical activity in the LA roof vein. A left: Local potential of the LA roof vein were seen after far-field LA potential. A right: Pacing in LA roof vein locally captured myocardial sleeve in LA roof vein apart from LA. B: Isoproterenol induced repeated firing (white arrow) from the LA roof vein. C: AP-Fluoroscopic view. PENTARAY® Nav Catheter was inserted into the LA roof vein. A 20 polar ring catheter was inserted in LSPV. D: The LA roof vein was isolated (black arrows) apart from LA (far-field small potentials with white arrows). RA: right atria, LA: left atria, LSPV: left superior pulmonary vein, CS: coronary sinus, ABL: ablation catheter.
3 Discussion
Complete elimination and/or isolation of triggered ectopy is the goal of RFCA treatment for PAF. Approximately 90% of triggered premature firing causing AF originates from PVs [1]. Therefore, PV isolation is the most important procedure for successful PAF treatment. Several anatomical PV diversities have been reported in approximately 20% of AF patients; common PVs [3], [4], supernumerary veins [5], and the LA roof vein [2]. These anatomical abnormalities sometimes complicate PVI, or may result in some remaining AF triggers. Pre-operative 3D-CT is useful to identify the anatomical diversity of LA and PVs [4]. Accessary “top vein” is also reported [4], draining to superior PVs. However, the LA roof vein draining to the LA roof area seen in this case is a highly rare abnormality. The operator should consider possible AF triggers from diversities in anatomy. Such a rare type of LA roof vein may not have been recognized if these pre-operative 3D-CT had not been performed in this case.
An original report of “LA roof vein” by Igawa et al. [2] demonstrated that an LA roof vein does not have a myocardial sleeve proven by histological evaluation in autopsy, i.e., which cannot cause AF. They reported the importance of recognition of LA roof vein as the risk of complication. In this case, however, the LA roof vein had electrical activity and recorded local spontaneous firing, suggesting that it can be the trigger of AF. This vein ran from the right superior lobe of the lung to the left side of LA roof; therefore, it may have a myocardial sleeve as same as general PVs.
In this case, an episodic AF trigged by ectopy from LA roof vein could not be demonstrated; however, since local ectopy only in LA roof vein was observed under adrenergic stimulation, i.e., no ectopies were observed from 4 PVs, superior vena cava or other area even under ISP infusion, we decided to isolate the LA roof vein concomitant with routine PVI. Currently, no recurrence of AF has been observed after RFCA for over 13 months.
4 Conclusion
We experienced a rare form of a LA roof vein with arrhythmogenicity. Given the confirmed abnormal electrical activities in this unusual vein, its isolation was necessary to eliminate AF triggers.
Conflict of interest
All authors declare no conflict of interest related to this study.
Acknowledgement
We thank Akikazu Takeda, Minami Sato, Yuka Kiriya-Sato, and Kasumi Wada for their excellent technical support as medical engineers to performed RFCA.




