Antiarrhythmogenic effect of omega-3 fatty acid ethyl esters in a patient treated with Omacor after a non-Q-wave myocardial infarction
Abstract
An 84-year-old man reported several episodes of palpitations over the previous 6 months. He had a history of a prior non-Q-wave myocardial infarction (MI) and had received a dual-chamber pacemaker for control of subsequent sick sinus syndrome. Pacemaker data revealed 8000 premature ventricular beats (PVBs) daily and nonsustained ventricular tachycardia (NSVT).
The patient agreed to add omega-3 fatty acid ethyl ester supplementation (1 g/day) to his treatment regimen. Pacemaker analyses 3 months later demonstrated no NSVT and only 215 PVBs daily. In more than 1 year of follow-up, the patient has remained well and has had no further ventricular arrhythmias. We conclude that omega-3 fatty acid ethyl ester supplementation may be beneficial in post-MI patients with pacemakers who develop ventricular arrhythmias.
1 Introduction
The management of patients with ischemic ventricular arrhythmias is complex and may consist of one or more of the following treatment options: placement of an implantable cardioverter defibrillator (ICD), use of radiofrequency ablation, and/or prescription of conventional antiarrhythmic drugs. The basis of treatment is technically challenging and may be associated with significant procedural risks. In this report, we present a case that illustrates the potential role of omega-3 fatty acid ethyl ester supplementation in the management of these difficult-to-treat patients.
2 Case Report
During a routine follow-up evaluation in December 2011, an 84-year-old man reported that he had experienced several episodes of palpitations over the previous 6 months, without associated symptoms of vertigo, presyncope, syncope, or angina.
The patient had previously experienced a non-Q-wave myocardial infarction (MI) in 2005. At the time, he had not been taking his prescribed medications regularly. He reported that he had been previously well and that he enjoyed strenuous physical activity, particularly hunting. He was referred to our clinic 2 years after the MI when he was diagnosed with sick sinus syndrome while being medically managed with a beta blocker (bisoprolol), aspirin, and an angiotensin-converting enzyme (ACE) inhibitor (perindopril). To treat his condition, we implanted an ALTRUA dual-chamber pacemaker (DDDR; Boston Scientific, MN, USA).
Analysis of the data in the pacemaker memory in December 2011 did not indicate any malfunction and showed that approximately 8000 premature ventricular beats (PVBs) and non-sustained ventricular tachycardia (NSVT) were occurring daily (Fig. 1). According to the patient's diary, the episodes of NSVT and PVBs coincided with his symptoms. Furthermore, the results of 24-h Holter monitoring corresponded with the pacemaker data. At this time, his body mass index (BMI) was 26.
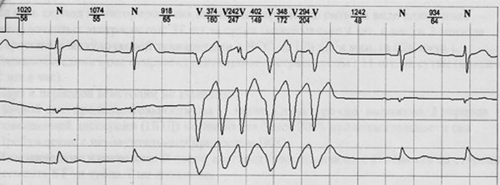
Episodes of nonsustained ventricular tachycardia (3 separate channels of Holter monitoring).
Echocardiography revealed a near-normal size of the left ventricular chamber, with preserved global systolic function. The patient's functional class, as rated by the New York Heart Association Functional Classification (NYHA-FC), was I–II. When we discussed his diet with him, we found that he typically ate less than 1 portion of oily fish per week.
The patient refused to undergo any interventional procedures (e.g. angiography or an electrophysiologic study) to evaluate the status of his coronary artery disease and to assess the possible need for upgrading his ICD. According to current guidelines [1] and in view of his poor dietary intake of polyunsaturated fatty acids (PUFAs), he agreed to add an omega-3 fatty acid ethyl ester supplement (Omacor, known as Lovaza in the US [1 g/day], Abbott Russia LLC) to his treatment regimen.
When the patient returned for his follow-up appointment 3 months later in March 2012, he noted that he felt well and that his palpitations had stopped. Pacemaker data and 24-h Holter monitoring performed in May 2012 demonstrated no NSVT and showed only 215 PVBs daily.
Since he began taking omega-3 fatty acid ethyl ester supplementation, the patient has remained well. At a follow-up review in of June 2012, he confirmed that he continues to be physically active and to enjoy hunting. He currently takes Omacor (1 g/day), statins, and aspirin, but he refuses to take beta blockers and ACE inhibitors. Importantly, he has experienced no further episodes of ventricular arrhythmias (Fig. 2); therefore, radiofrequency ablation or ICD placement has not yet been required.
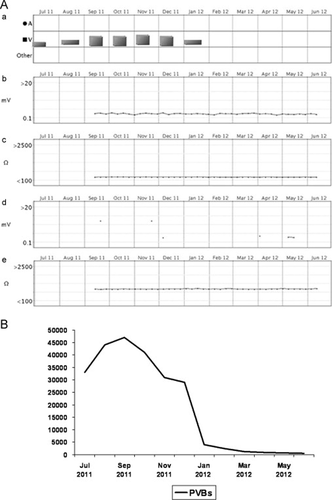
Frequency of ventricular events. (A) (a) Ventricular events, (b) P-wave amplitude, (c) A-pace impedance, (d) R-wave of Vamplitude, and (e) V-pace impedance from the pacemaker memory (June 19, 2012) illustrates the positive influence of Omacor intake (A, atrial events; V, ventricular events). (B) Graph of the number of premature ventricular beats (PVBs).
3 Discussion
Fish oil derivatives may protect against sudden cardiac death [2]. The Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico (GISSI-Prevention) Study of 11,324 patients who had survived a recent MI demonstrated a highly significant (45%) reduction in risk of sudden cardiac death in the group that received omega-3 fatty acid ethyl ester supplementation with Omacor [3]. The reduction in the rate of death caused by cardiac events was significant by month 4 (p=0.048) [4].
The effect of high-dose omega-3 fatty acids has been examined in 3 randomized controlled trials that focused specifically on ventricular arrhythmias in patients with ICDs for secondary prevention of MI [5]-[7]. The results of these 3 studies were inconsistent. The Study on Omega-3 Fatty Acids and Ventricular Arrhythmia (SOFA; n=546) reported a non-significant trend toward event-free survival in a subgroup with prior MI randomized to 2 g of fish oil per day (Table 1) [5], [8]. In the Fatty Acid Antiarrhythmia Trial (FAAT; n=402), the use of omega-3 fatty acids was associated with a significant extension (33%) of the time until the first use of ICD or death [6]. However, the third trial of 200 patients who received an ICD because of sustained ventricular tachycardia or ventricular fibrillation (and not after an MI) failed to show a reduction in episodes of ventricular tachyarrhythmia after routine supplementation with omega-3 fatty acids [7]. As suggested by the authors of a recent meta-analysis, the discrepancies in results among these 3 trials may be due to the use of different antiarrhythmic medications and/or due to the different interactions of these antiarrhythmic drugs with the omega-3 fatty acids. There was also heterogeneity among the study populations [9].
| Study (Reference) | No. of patients | Follow-up duration (months) | Daily dose (g) | Event rate | p Value | |
|---|---|---|---|---|---|---|
| Fish oil group (%) | Control group (%) | |||||
| SOFA [5] | 546 | 12 | 2 | 30 | 33 | 0.33 |
| FAAT [6] | 402 | 12 | 4 | 28 | 39 | 0.057 |
| Raitt et al. [7] | 200 | 24 | 1.8 | 65 | 59 | 0.19 |
- FAAT=Fatty Acid Antiarrhythmia Trial; SOFA=Study on Omega-3 Fatty Acids and Ventricular Arrhythmia.
Three possible mechanisms may underlie the decrease in the number of PVBs in the present patient: the first is the antiarrhythmic action of Omacor, the second is the natural time course of PVBs, and the third is the day-to-day variability in the number of PVBs. Therefore, we performed an additional evaluation in February2013. Based on the device interrogation data, which demonstrated that the total number of PVBs ranged from 400 to 2000 per month since March 2012 until recently, we believe that day-to-day variability of PVBs is the least likely reason for the decreased number of PVBs. Previous device testing (from June 2011 to Jan 2012) had shown up to 50,000 PVBs per month.
Data regarding the surrogate antiarrhythmogenic effect of PUFAs are currently rather controversial. Preliminary results from a pilot study showed that a single intravenous administration of 3.8 g of omega-3 marine triglycerides resulted in decreased induction of sustained ventricular tachycardia following programmed stimulation in 5 of 7 ischemic patients with inducible ventricular tachycardia [10]. A larger study involving 98 patients with ICDs and ischemic heart disease showed that higher plasma levels of n-3-PUFAs are associated with a lower incidence of ventricular arrhythmias [11].
Several studies have shown that omega-3 fatty acids utilize multiple antiarrhythmic mechanisms, including the inhibition of calcium overload by maintenance of l-type calcium channels during cellular stress, high activity of cardiac microsomal calcium ion–magnesium ion-adenosine triphosphate synthase (Ca2+/Mg2+-ATPase), and potent inhibition of voltage-gated sodium channels [12]-[14].
The present patient had a history of a prior non-Q-wave MI, episodes of mildly symptomatic NSVT, and preserved global systolic function of LV; he therefore corresponds to the GISSI-P trial profile. It is unclear whether the patient's arrhythmia was linked strictly to his prior MI and/or transient myocardial ischemia because he refused to undergo electrophysiologic study and angiography. We did not want to discontinue his treatment with Omacor and re-challenge him to confirm the efficacy of omega-3 fatty acids in this particular case. Therefore, the omega-3 index before and after treatment was not evaluated for this patient.
4 Conclusions
In the present case, there was a clear positive association between the commencement of treatment with Omacor and the cessation of palpitations, although any link must be considered speculative. The observed dramatic benefit has been sustained over 12 months of follow-up, in the absence of beta-blocker or ACE-inhibitor therapies, suggesting a genuine effect of Omacor. Therefore, we suggest that non-invasive omega-3 fatty acid ethyl ester supplementation with Omacor may be of benefit in post-MI patients with ICDs who develop ventricular arrhythmias.
Acknowledgments and funding
The authors acknowledge editorial support provided by Dr. Christine Smart, Adelphi Communications Ltd., UK.
The development of this paper was supported by an unrestricted educational grant from Abbott Products Operations AG, Allschwil, Switzerland.




