Natriuretic peptides for risk stratification of patients with acute coronary syndromes
Abstract
Natriuretic peptides (BNP and NT-proBNP) have been shown to be useful tools for risk stratification of patients with acute myocardial ischemia encompassing the whole spectrum of acute coronary syndromes (ACS), particularly for prediction of mortality. Both BNP and NT-proBNP possess several characteristics of the ideal biomarker, showing independent and incremental prognostic value above traditional clinical, electrocardiographic, and biochemical (particularly troponin) risk indicators. Specifically, in ACS patients, BNP and NT-proBNP have powerful prognostic value both in patients without a history of previous heart failure or without clinical or instrumental signs of left ventricular dysfunction on admission or during hospital stay. They can also be easily and rapidly measured in an emergency context. We have performed a meta-analysis of available studies concerning the prognostic value of natriuretic peptides. Our results show that the prognostic value of natriuretic peptides is similar: (1) both at short- and long-term; (2) when natriuretic peptides are measured at first patient contact or during hospital stay; (3) for BNP or NT-proBNP; and (4) in patients with ST elevation myocardial infarction or no ST elevation ACS. These data suggest that natriuretic peptide measurement should be integrated into routine evaluation of patients with an ACS.
1. Introduction
Risk stratification of patients with acute coronary syndromes (ACS), whether with ST-elevation myocardial infarction (STEMI) or without persistent ST-elevation (NSTE-ACS), is fundamental in determining prognosis and choosing appropriate care. This improves the cost-effectiveness of patient care since evidence-based treatments (such as anti-platelet, anti-thrombotic, and revascularization therapies) can be targeted at the patients who are most likely to benefit from their use.
Risk assessment is based on the clinical history, examination findings, electrocardiographic (ECG) changes, and markers of myocardial damage, particularly cardiac troponin 1–3. The prognostic indicators should be available at the time of initial patient evaluation, in order to maximize the potential benefit of early risk-assessment. Currently, despite careful integration of key prognostic variables, risk prediction based on clinical, electrocardiographic, and biochemical, i.e. cardiac troponin, markers is relatively inaccurate 4. Therefore, there is still room for new prognostic indicators. For this purpose, there is emerging evidence that natriuretic peptides possess several characteristics of the ideal biomarker; in addition, rapid immunoassays have recently become available at a reasonable cost.
There are three classes of natriuretic peptides 5,6. Both BNP and NT-proBNP have been shown to aid in the diagnosis of heart failure and to correlate with functional status among patients with CHF 7. Levels of BNP and NT-proBNP also correlate with left ventricular dilatation, remodelling, and dysfunction, as well as heart failure and death among patients presenting with acute myocardial infarction 8,9.
A robust association between BNP or NT-proBNP and the short- and long-term risk of death across the spectrum of ACS has recently been demonstrated 10–16,23. In some patients with ACS, elevated levels of BNP directly reflect the degree of left ventricular dysfunction resulting from acute myocardial infarction. However, the strong association between levels of BNP and NT-proBNP and mortality even among patients without myocyte necrosis (as detected by the release of cardiac troponin) indicate that the level of BNP may reflect the extent or severity of the ischemic insult, even when irreversible injury has not occurred.
In this paper we review the current evidence supporting the use of natriuretic peptides for early risk stratification of patients with ACS. For this purpose, we have combined the results of four published studies and one study published as an abstract, using meta-analysis techniques 11–14,16, in order to address some clinically relevant questions: (1) is the prognostic value of natriuretic peptides (BNP and NT-proBNP) similar both at short- and long-term=; (2) is the prognostic value similar when natriuretic peptides are measured at first patient contact or during hospital stay=; (3) is it better to measure BNP or NT-proBNP=; and (4) is the prognostic value similar in patients with STEMI or NSTE- ACS= Main characteristics of the included studies are summarized in Table 1.
| Study | Patients | Diagnosis (n) | Peptide/Assay | Median time from symptom onset to sampling | Median concentration |
|---|---|---|---|---|---|
| deLemos 15 | 2525 | STEMI (825) | BNP/Biosite | 40 h | 81.2 pg/ml |
| NSTE-ACS (1698) | immunoassay | ||||
| Omland 16 | 609 | STEMI (204) | N-BNP/Home made Ab | 3 days | 545 pmol/l |
| NSTE-ACS (405) | |||||
| Jernberg 14 | 775 | NSTE-ACS (407) | NT-proBNP/Roche | 6 h | 400 ng/l |
| assay | |||||
| Other (368) | |||||
| James 13 | 6809 | NSTE-ACS | NT-proBNP/Roche | 9.5 h | 669 ng/l |
| assay | |||||
| Galvani 18 | 1756 | STEMI (700) | NT-proBNP/Roche | 3 h | 353 ng/l |
| NSTE-ACS (1056) | assay |
- a Abbreviations: STEMI, ST-elevation myocardial infarction; NSTE-ACS, acute coronary syndrome without ST-elevation; BNP, B-type natriuretic peptide; NT-proBNP, N-terminal – pro B-type natriuretic peptide; Ab, antibody.
2. Natriuretic peptide release in acute myocardial ischemia
Elevated levels of natriuretic peptides have been detected in patients with ACS in the absence of detectable myocardial necrosis 17. It has been demonstrated that levels of BNP increase transiently after uncomplicated coronary angioplasty in the presence of stable intra-cardiac filling pressure, as well as after exercise-induced ischemia in patients with stable coronary artery disease 8. Together, these findings suggest that transient ischemia may induce BNP synthesis and release in proportion to the severity of myocardial ischemia. No such studies exist on ANP; furthermore, the different release kinetics and the different persistence in blood of BNP and NT-proBNP in comparison with ANP make the former a more attractive approach to risk-stratification of patients with ACS than the latter.
The mechanism of production of natriuretic peptides in myocardial ischemia is unclear. Myocardial ischemia in unstable angina may increase regional ventricular wall stretch owing to local depression of myocardial contraction. Mechanical stretch can activate the JAK/STAT pathway and may stimulate NT-proBNP secretion 18 and augment the messenger RNA expression of IL-6 and cardiotrophin 1 19. This common mechanism of stimulation may explain the correlation between NT-proBNP and cardiotrophin 1 in unstable angina. Alternatively, cardiotrophin 1 may directly promote myocardial transcription of BNP.
3. Natriuretic peptides concentrations in ACS
The interpretation of early natriuretic peptide measurement in ACS patients can be difficult since levels of BNP and NT-proBNP vary considerably according to index diagnosis 20 and rise continuously during the first 24 h after the onset of ischemia 21. It has been shown that natriuretic peptide levels are higher in patients with MI than in those with unstable angina, and in patients with STEMI than in those with NSTEMI, possibly reflecting the amount of myocardium at risk and the extent of myocardial necrosis. Concentrations increase very rapidly and steeply in the first day after the onset of myocardial ischemia, making the comparison of concentrations across different populations difficult. Finally, it must be acknowledged that BNP and NT-proBNP concentrations markedly differ by age, gender, and assay system 22.
It is therefore challenging to derive an optimal discriminatory prognostic cut-off according to these factors, possibly implying that a single cut-off level cannot be used in clinical practice. In the clinical studies, which we have taken into consideration, natriuretic peptide concentrations were reported as levels above or below the median value observed in the population under study, thus permitting a dichotomous approach to the interpretation of the results. For this reason, we have excluded studies where patients are classified according to the presence or the absence of elevations 10, and studies 7 where natriuretic peptide levels are divided into terciles.
4. Prognostic value of natriuretic peptides in ACS
The prognostic value of BNP and NT-proBNP, measured in the sub-acute phase, on mortality of patients with an ACS has been assessed in several studies. Omland et al. 15, in a nested case-control TIMI 11B sub-study, for the first time found higher NT-proBNP levels in patients with NSTE-ACS who died early than in those who survived. De Lemos et al. 13 included 2525 patients from one of the treatment arms of the OPUS-TIMI 16 trial. BNP, measured during the first few days after the onset of ischemic symptoms, was strongly and independently predictive of mortality at 10 months. Omland et al. also evaluated ‘real world’ patients in a study primarily designed to evaluate risk indicators in ACS 14. NT-proBNP was predictive of long-term mortality independently from Killip class, patient age, and left ventricular ejection fraction even in patients with no evidence of clinical heart failure.
The value of early measurement of natriuretic peptides has been less extensively studied. Jernberg et al. 12 measured NT-proBNP on admission in 755 patients admitted to the coronary care unit because of chest pain and no ST-segment elevation (54% with an ACS) at a median time of 6 h from the onset of symptoms. Compared to the lowest quartile, patients in the second, third and fourth quartiles had a relative risk of subsequent death of 4.2, 10.7 and 26.6, respectively. More recently, James et al. 11 measured NT-proBNP in 6809 out of 7800 ACS patients enrolled in the GUSTO-IV trial. Samples were obtained at a median of 9.5 h from symptom onset. The results of this study clearly showed that NT-proBNP was the strongest predictor of mortality, but was not an independent predictor of subsequent ischemic events. In fact, increasing quartiles of NT-proBNP were related to short- and long-term mortality that reached 1.8%, 3.9%, 7.7%, and 19.2% (P<0.001), respectively, at 1 year. Finally, we measured NT-proBNP at a median time of 3 h after symptom onset in 1756 patients with ACS 16. The outcome measure of our study was death at 30 days, which occurred in 113 patients. The median NT-proBNP level was 353 (107 to 1357) ng/l. Compared to the lowest quartile, patients in the second, third and fourth quartiles had a relative risk of subsequent death of 2.94, 5.32, and 11.5, respectively. NT-proBNP was independently associated with death in a logistic regression model, which included clinical variables, ECG, and troponin T both in patients with and without persistent ST-segment elevation. NT-proBNP was also an independent predictor of the short-term occurrence of severe heart failure.
All these studies are concordant in indicating that BNP and NT-proBNP are independent predictors of subsequent mortality. The prognostic information of natriuretic peptide measurement is in fact additional to several key prognostic variables. In particular, BNP and NT-proBNP allow to further stratify the risk of two important patient subgroups: those without overt signs of heart failure and those without troponin elevations on admission. Secondly, although being powerful predictors of the occurrence of heart failure, natriuretic peptides are not predictors of subsequent recurrent ischemic events, particularly non-fatal myocardial infarction. This is in keeping with the pathophysiology of BNP and NT-proBNP elevations, which are not causally linked to the progression of coronary thrombosis with its attendant ischemic complications.
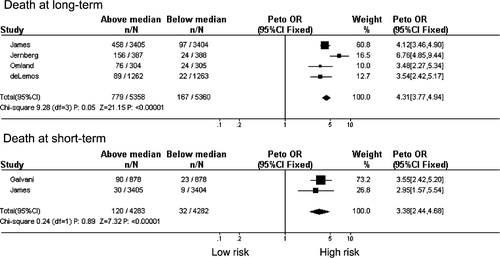
4.1. Short-term vs. long-term mortality
The results of our meta-analysis indicate that the prognostic value of BNP and NT-proBNP is similar both in the long-term (OR 4.31; 95% CI 3.77–4.94) and in the short-term (OR 3.38; 95% CI 2.44–4.68). This observation has important practical implications since the demonstration of a short-term prognostic value may justify research efforts directed to target specific interventions in patients with elevated natriuretic peptide levels during the acute phase of the disease (Fig. 1).
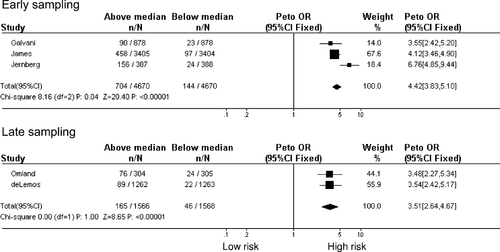
4.2. Early sampling vs. late sampling
The results of our meta-analysis also show that the prognostic value of natriuretic peptide measurement is similar when blood is obtained at the time of first patient contact (OR 4.42; 95% CI 3.83–5.10) or in the following hours or days after admission (OR 3.51; 95% CI 2.64–4.67). The prognostic value of natriuretic peptide measurement, when performed in the sub-acute phase of STEMI, is well established. The findings of the recent studies conducted on the whole spectrum of patients with ACS expand and reinforce this observation showing that the same prognostic discriminatory capacity is obtained when measurement is obtained as soon as possible, suggesting that the adverse prognosis associated with the finding of elevated natriuretic peptide levels might be favorably influenced by immediate or, at least, early therapeutic interventions (Fig. 2).
4.3. BNP vs. NT-proBNP
Plasma concentrations of BNP and NT-proBNP are correlated. However, in patients with left ventricular dysfunction, the proportional and absolute increase of NT-proBNP exceeds that of BNP, suggesting that NT-proBNP may be a more sensitive marker of left ventricular dysfunction 24.
There is only one study which evaluated the prognostic value of BNP 13; therefore a formal meta-analysis is not possible. In that study, the OR of death in patients with BNP levels above and below the median value of the population was 3.54 (95% CI 2.42–5.17). This value is only slightly lower than the OR ratio observed in studies with NT-proBNP (4.42; 95% CI 3.83-5.10) suggesting that both BNP and NT-proBNP can be used in clinical practice for prognostic purposes.
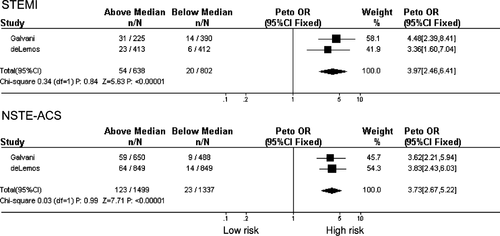
4.4. STEMI vs. NSTE-ACS
There were only two studies evaluating the whole spectrum of patients with ACS, thus allowing a direct comparison across patient sub-groups. In one study, blood was sampled very early; in the other study blood was obtained in the sub-acute phase. This difference was particularly pronounced in the case of patients with STEMI. It is interesting to observe that the prognostic value of natriuretic peptide measurement was remarkably similar in the two studies and across patient sub-groups. This finding suggests a role for early natriuretic peptide measurement even in patients with STEMI (Fig. 3).
5. Therapeutic interventions according to natriuretic peptide levels
In patients with NSTE-ACS, two studies have evaluated whether an invasive strategy is particularly effective in patients with elevated BNP and NT-proBNP levels, reporting apparently conflicting results.
Morrow et al. 10 evaluated BNP at baseline in 1676 patients randomized to early invasive vs. conservative management in the TACTICS-TIMI 18 trial. Patients with elevated BNP (≥80 pg/ml; n=320) were at higher risk of death at seven days (2.5% vs. 0.7%, P<0.006) and 6 months (8.4% vs. 1.8%, P<0.0001). No difference, however, was observed in the effect of invasive vs. conservative management when stratified by baseline levels of BNP (Pfor interaction=0.6). Patients with BNP levels ≥80 pg/ml had a 6 month mortality rate of 7.9% when assigned to an invasive strategy, and a mortality if 9.0% when assigned to a conservative approach (OR 0.87; 95% CI 0.4–1.9).
Jernberg et al. 7 examined whether measurements of NT-proBNP, in addition to troponin T and interleukin-6, improved the ability to identify high-risk patients who benefit from an early invasive strategy in 2019 patients randomized to an invasive or non-invasive strategy in the FRISC-II trial. Patients were followed up for 2 years to determine death and MI. Patients in the third NT-proBNP tertile had a 4.1-fold (95% CI 2.4–7.2) and 3.5-fold (95% CI 1.8–6.8) increased mortality in the non-invasive and invasive groups, respectively. In patients with increased levels of both NT-proBNP and IL-6, an early invasive strategy reduced mortality by 7.3% (risk ratio 0.46, 95% CI 0.21–1.00). In patients with lower NT-proBNP or IL-6 levels, the mortality was not reduced. Reasons for possible differences between the two studies are not completely clear 25. One possible reason is that NT-proBNP elevations, being more pronounced than those of BNP, identify a larger proportion of patients with elevations thus permitting a more balanced comparison between patients with and without elevations. Furthermore, in contrast with FRISC-II, the invasive approach did not reduce mortality in TACTICS-TIMI 18; this precludes detecting mortality differences in the subset of patients with BNP elevations. Nevertheless, the non-significant 13% relative reduction in 6-month mortality seen in TACTICS-TIMI-18 patients with BNP levels of ≥80 pg/ml (odds ratio 0.87, 95% CI 0.4–1.9) is not inconsistent with the 41% relative reduction in 2-year mortality seen in patients in the highest tertile of NT-proBNP levels in FRISC-II.
No data exist about the preferred therapeutic approach to patients with elevated natriuretic peptide levels in STEMI.
6. Conclusion
Natriuretic peptide measurement is a powerful tool to assess the risk of death in patients with ACS. The information provided by this biomarker is incremental to that offered by conventional risk markers. Given the ability to capture the risk of troponin negative patients, it offers promise to integrate troponin as first-line biomarker particularly when blood is sampled very early after the onset of ischemia. There are, however, pitfalls to its immediate implementation in clinical practice related to the application of decisional cut-off levels (which, in our opinion, should take into consideration age, sex, index diagnosis and time from symptom onset), and the identification of specific therapeutic approaches to patients with elevated natriuretic peptide levels.




