NT-proBNP in heart failure: therapy decisions and monitoring
Abstract
With increasing cardiac dysfunction, a complex neurohormonal response results in increasing circulating levels of an array of plasma hormones. Increments in plasma levels of atrial natriuretic peptide (ANP) and B-type natriuretic peptide (BNP) and their amino-terminal congeners are more closely related to cardiac structure and function and to cardiovascular prognosis than changes in other plasma neurohormones. Reports suggest that changes in plasma BNP levels in the course of treatment of acutely decompensated heart failure provide a more powerful prognostic indicator of the likelihood of survival or recurrent decompensation than symptomatic assessment. This observation requires a randomised controlled trial in which changes in peptide levels determine aggression and duration of in-patient therapy in order to establish whether this indicator can improve results from management of acute in-patient heart failure. Plasma BNP or NT-proBNP is a powerful independent predictor of mortality and morbidity in long-term follow-up of heart failure cohorts. In addition, it appears likely to be a good predictor of beneficial response to the addition of beta blockade to anti-heart failure pharmacotherapy. Finally, adjustment of therapy for heart failure according to serial measurements of NT-proBNP promises to improve outcomes in comparison with adjusting therapy according to unassisted clinical acumen.
1. Introduction
With increasing cardiac dysfunction, synthesis and release of cardiac natriuretic peptides rises incrementally in concert with other neurohormonal responses observed in heart failure. Plasma concentrations of the cardiac natriuretic peptides and their pro-hormone and amino-terminal congeners, are increased irrespective of whether the aetiology of heart failure is ischaemic, hypertensive, valvular or a primary cardiomyopathic process. Plasma atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP) levels correlate positively with cardiac filling pressures and volumes and are inversely-related to left ventricular ejection fraction 1–5.
Plasma concentrations of BNP and amino-terminal pro-B-type natriuretic peptide (NT-proBNP) are more closely related to measurements of cardiac structure and function and to cardiovascular prognosis than ANP or other circulating neurohumoral markers of cardiac disease 5–7. Therefore, measurements of BNP or NT-proBNP, taken together with conventional clinical assessment, may assist in the decision of whether or not to initiate anti-heart failure pharmacotherapy and also in serial adjustment of such treatment. To date, despite the plethora of publications confirming the relationship of plasma BNP and/or NT-proBNP with cardiac function and prognosis in a broad array of cardiovascular disease extending from acute coronary syndromes through to established heart failure, there is very little information available concerning the utility or otherwise of single or serial measurements of plasma NT-proBNP in therapeutic decision making. The following brief review summarises available information concerning the reported relationship between changes in plasma concentrations of BNP or NT-proBNP and clinical outcomes in patients admitted to hospital for management of decompensated heart failure. The relationship of these peptides to medium and longer term outcomes in established cardiac failure in the context of randomised controlled trials will also be discussed. Finally, the even more limited information concerning application of serial measurements of plasma hormones to adjust anti-heart failure pharmacotherapy will be summarised.
2. Acutely decompensated heart failure
Cheng et al. 8 employed a point of care immunoassay for BNP to assess changes in plasma BNP levels in 72 patients admitted with decompensated heart failure. They found an association between initial BNP measurement and pre-discharge BNP measurement and subsequent risk of death and/or 30-day readmission. Within this period, 22 adverse end points occurred including 13 deaths and nine readmissions to hospital. Notably in the patients destined to incur these adverse outcomes, plasma BNP levels were observed to increase during the hospital stay (mean increment 233 pg/ml, P<0.001). In contrast, in those patients surviving and avoiding readmission to hospital during the 30-day follow-up period, mean plasma levels of BNP fell (mean decrease 215 pg/ml). Univariate analyses indicated pre-discharge BNP was strongly associated with the risk of the combined adverse end point. The mean age of the study group was 68 years. The mean left ventricular ejection fraction was 37%. The predominant aetiology of heart failure was ischaemic. Significant associated renal failure was present in 25% of patients. The mean hospital stay was greater than 16 days. Parenteral anti-failure therapy and/or Swan–Ganz catheter placement were utilised in more than one-third of the study group. Overall, it appears that this was a group of patients with severe decompensated heart failure. Notably in those patients destined to escape an adverse 30-day outcome, NYHA class fell in parallel with change from admission to pre-discharge plasma BNP levels but this parallelism was absent in those incurring end points. In the latter sub-group, although NYHA status fell from class IV to class III (e.g. for those later readmitted within 30 days) plasma BNP levels clearly did not alter on average. In the case of those destined to die within 30 days of discharge, BNP levels frankly increased by at least 30% whilst NYHA class was unchanged or fell slightly. Hence, in those patients admitted acutely to hospital with frankly decompensated heart failure, change in plasma B-type natriuretic peptide concentrations over a period of several days of intensive therapy constituted a better guide to 30-day outcomes than did change in symptoms as indicated by NYHA class.
At the time of writing, no parallel data for measurements of plasma NT-proBNP are available in full published form. However, preliminary data from Bettencourt et al. in Portugal (see paper in this issue) in a study of 182 consecutive patients admitted with decompensated heart failure, the presence of a 30% or more elevation in NT-proBNP during the course of the hospital admission strongly predicted adverse outcomes over the following 6-month period.
A rational follow-on from these observations would be a randomised controlled trial of modification of treatment and discharge time according to change in plasma BNP or NT-proBNP from admission to the point where clinical compensation is thought to have been achieved. A trial, which randomises patients to discharge according to ‘usual practice’ compared with the possibility of being retained for a longer period of stay with introduction of more intensive therapy according to the presence or absence of a threshold level of NT-proBNP should be undertaken. The outcomes of this trial may have important consequences in terms of avoiding early readmission or mortality after a hospital stay for treatment of acutely decompensated heart failure. The choice of a particular threshold value of NT-proBNP or BNP vs. observation of a directional shift in the peptide during the course of the acute admission, is the subject of debate. It is likely that with severe residual cardiac dysfunction many patients will exhibit sustained high levels of plasma peptide in spite of clinical improvement and some decline in peptide concentrations during the course of intensive therapy. In view of this, it may be more practical to aim for a given percentage (e.g. 30% decline) change in peptide levels, taken in concert with resolution of clinical signs and symptoms, as a potential guideline for appropriate timing of discharge.
The longer term prognostic power of pre-discharge BNP or NT-proBNP plasma concentration measurements in patients completing a hospital stay for management of acute decompensated heart failure is not fully clear. The Christchurch Cardioendocrine Research Group has undertaken observations in 600 patients surviving an admission for decompensated heart failure. In these patients, pre-discharge blood samples were obtained for measurement of BNP, NT-proBNP, ANP and proANP (N-ANP) in addition to plasma renin activity and plasma concentrations of angiotensin II, aldosterone, norepinephrine, adrenomedullin and endothelin 1. Notably, at the point patients were considered fit for discharge, plasma concentrations of angiotensin II and aldosterone fell well within the normal range, although renin activity was increased (presumably reflecting the impact of converting enzyme inhibitor and/or diuretic therapy). Norepinephrine and adrenomedullin levels also fell within the normal range. However, on average, endothelin 1 levels clearly remained elevated beyond normal. Compared with these other circulating markers of cardiovascular status and prognosis, plasma concentrations of all four of the cardiac natriuretic peptides were markedly elevated beyond normal. In the case of ANP and BNP, this elevation was at three–four-fold the upper limit of normal. For proANP two-fold upper limit of normal, and in the case of NT-proBNP, close to five-fold the upper limit of normal using the Christchurch in-house radioimmunoassay 9. Pre-discharge NT-proBNP was 237 pmol/l (the normal range for this assay being 2–50 pmol/l).
The 600 patients have now been followed for a mean observation period of 2 years post-discharge and in that time it has become clear that BNP and NT-proBNP are the most powerful single circulating markers of risk of mortality. In the case of NT-proBNP, 168 deaths have occurred in the 296 patients with pre-discharge NT-proBNP levels above the elevated median level of 237 pmol/l (57% mortality). In the case of those with pre-discharge NT-proBNP concentrations below this median value, 86 deaths out of 295 patients have occurred (cumulative mortality of 29%). Thus, even in an extremely frail and ill group with a poor overall prognosis, division of the group above and below the median level of NT-proBNP (approx. five-fold upper limit of normal) still provides a powerful risk stratification with approximately two-fold risk of dying over the 2-year follow-up in those with above median levels of peptide (unpublished data).
3. B-type natriuretic peptides and prediction of response to anti-failure therapy
Neurohormonal sub-studies from landmark randomised controlled trials of converting enzyme inhibitors in heart failure have suggested that plasma neurohormonal status can predict benefit from introduction of such therapy. In an early trial of converting enzyme inhibition in severe heart failure 10 pre-randomisation measurements of norepinephrine, renin activity, angiotensin II, aldosterone and plasma atrial natriuretic peptide all indicated greater likelihood of benefit from introduction of enalapril. These findings were essentially supported by later reports from the V-HeFT 11 ValHeFT 7 and SAVE 12 studies. However, neither plasma BNP nor NT-proBNP was measured in neurohormonal sub-studies of randomised controlled trials of therapy in heart failure until the beta blocker therapy trials were launched. The Australia–New Zealand Heart Failure Group reported neurohormonal data from their ANZ Heart Failure Trial of carvedilol. In this study of 415 patients with confirmed ischaemic heart disease and ejection fractions of <45%, blood sampling was taken for a panel of neurohormones prior to randomisation to placebo or carvedilol in addition to established therapy with converting enzyme inhibitors and loop diuretics. The overall clinical result was a reduction in the composite end point of death and hospital admission. Pre-randomisation levels of BNP and NT-proBNP were both predictive of outcome irrespective of allocation to therapy with an above median level of either BNP or NT-proBNP conferring a two-fold risk of adverse end points, including readmission with heart failure during the trial follow-up period. In addition to this, both peptides appeared independently to predict a beneficial response to carvedilol 13,14. Recently, as yet unpublished, data from the COPERNICUS study in severe heart failure has suggested a similar trend with greater absolute benefit conferred by administration of carvedilol in the sub-group of patients with the most elevated NT-proBNP concentrations.
Reports from the ValHeFT trial of valsartan or placebo added to ACE inhibitor in patients with congestive heart failure (left ventricular ejection fraction <40%) have confirmed the predictive value of BNP with successive quartiles of plasma BNP levels being associated with an incremental increase in mortality over the time of the trial 7. BNP showed a far greater discriminatory power than plasma norepinephrine. Whether or not plasma BNP predicted more benefit from addition of valsartan to an ACE inhibitor is not yet reported.
4. Plasma NT-proBNP in titration of anti-heart failure treatment
Because of the well reported correlations between plasma BNP and NT-proBNP and concurrent haemodynamic measurements and indicators of left ventricular systolic function, it is possible that adjustment of anti-heart failure therapy according to serial measurements of BNP (in addition to standard clinical assessment) may offer improved outcomes. That converting enzyme inhibitors and diuretics lower BNP quite rapidly during the course of increased therapy in heart failure, has been well demonstrated 15. These findings taken together were the rationale for a treatment of heart failure guided by plasma NT-proBNP levels performed by the Christchurch Cardioendocrine Research Group 16. Based on the hypothesis that any treatment that reduced NT-proBNP levels below 200 pmol/l (in-house Christchurch Cardioendocrine Research Group radioimmunoassay) would reduce cardiac events, patients were recruited to the trial by virtue of having had recent decompensated heart failure in in-patient or outpatient settings coupled with an ejection fraction of ≤40%. They were randomised to treatment guided by serial measurement of NT-proBNP or according to a rigorously applied clinical algorithm, which was based on the Framingham criteria for diagnosis of heart failure. After baseline investigations, patients were followed at 3 monthly intervals provided their plasma NT-proBNP level fell below the target level or they satisfied the clinical criteria applied to determine cardiac compensation. If these targets were not met, then treatment was augmented in stepwise fashion according to a pre-determined algorithm with repeat measurements and increments in therapy occurring at 10–14-day intervals.
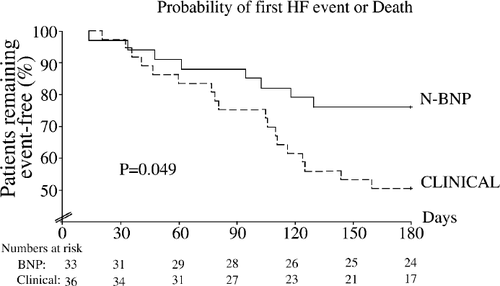
Mean plasma NT-proBNP levels fell in the hormone-guided group but not in the group managed clinically. The probability of a first heart failure event or mortality was significantly reduced in the heart failure group with a total of 19 cardiovascular events compared with 54 (Fig. 1). A multivariate analysis allowing for trends to difference in age, NYHA class, left ventricular ejection fraction, initial NT-proBNP, converting enzyme inhibitor dose, frusemide dose and systolic blood pressure gave a highly significant difference between the treatment groups in favour of the NT-proBNP-guided group (P<0.001). The investigators concluded that treatment of heart failure guided by NT-proBNP levels appeared to reduce cardiovascular events compared to intensive clinically guided treatment and this warranted further investigation. Subsequently, the Christchurch group has proceeded to initiate a further trial in a larger patient group with a broader spectrum of left ventricular function, age, co-morbidity and with a modernised drug algorithm. The ‘BATTLESCARRED’ trial (BNP Assisted Treatment To LEssen Serial CARdiac REadmissions and Death) admits all those over 18 years satisfying Framingham criteria for heart failure with or without reduced ejection fraction. To date over 200 patients have been enrolled.
In conclusion, use of NT-proBNP or BNP for management of heart failure is warranted in view of the increasing prevalence of this serious condition and the need to consider a broadening spectrum of dysfunction for treatment. In addition, the complexity of treatment is increasing with a number of agents demonstrated as effective through randomised controlled trials. There will be variable clinical expertise available to diagnose and manage the increasing cohort of heart failure patients with the passage of time, and an objective indicator to assist optimal prescription of medications is necessary. At present, plasma measurements of BNP or NT-proBNP constitute the best candidate for this function.




