N-terminal pro brain natriuretic peptide in arterial hypertension—a marker for left ventricular dimensions and prognosis
Abstract
In arterial hypertension risk factor evaluation, including LV mass measurements, and risk stratification using risk charts or programs, is generally recommended. In heart failure NT-proBNP has been shown to be a marker of LV dimensions and of prognosis. If the same diagnostic and prognostic value is present in arterial hypertension, risk factor evaluation would be easier. In 36 patients with arterial hypertension, electrocardiographic LV hypertrophy and preserved left ventricular function, NT-proBNP was eight-fold higher than in healthy subjects. The log NT-proBNP correlated with LV mass index (R=0.47, P=0.0002) measured by magnetic resonance imaging. In other subjects with arterial hypertension a significant but weak correlation to diastolic properties has been demonstrated. As for prognosis, a recent study in patients with hypertension, electrocardiographic left ventricular hypertrophy and preserved LV function demonstrated that NT-proBNP was a very strong prognostic marker, especially combined with a history of cardiovascular disease. Patients with high NT-proBNP and known cardiovascular disease had a seven-fold increase in CV events compared to patients with low NT-proBNP and no CV disease, while patients with either high NT-proBNP or CV disease had a three–four-fold increased risk. In conclusion NT-proBNP predicts LV mass in hypertensive patients and is a very strong prognostic marker in these patients. This could indicate a use of NT-proBNP in the future for risk stratification and perhaps monitoring of treatment in patients with arterial hypertension.
1. Introduction
Arterial hypertension is a major health problem, affecting approximately 25% of the adult population, and an increasing economic burden for the health care system due to cardiovascular complications and due to the growing use of antihypertensive drugs; 2–3 drugs are necessary in most patients to control blood pressure 1.
The cardiovascular risk in hypertensive patients is not only dependent on the magnitude of the elevation in blood pressure, but also on other risk factors, such as age, sex, smoking, cholesterol level, diabetes, etc. The global risk for the individual patient can be estimated using risk charts or computer programmes 2. In high risk patients intensive treatment including rigorous blood pressure control is warranted, while a less aggressive approach may be taken for the management of low risk patients.
A single powerful risk marker for use in clinical practice, alone or in combination with other means of risk stratification, would make assessment of these patients much easier. Brain natriuretic peptide (BNP) and its split product N-terminal pro BNP (NT-proBNP) are closely related to left ventricular (LV) dimensions, function and mass 3, and a valuable diagnostic 4 and prognostic tool 5 in patients with heart failure. These peptides are also strong prognostic markers in unselected populations 6, but the significance of the natriuretic peptides in patients with hypertension and preserved LV systolic function is largely unknown.
2. Evaluation of cardiac structure and function
As BNP primarily reflects myocyte stretch 7 it is possible that LV hypertrophy induces an increase in NT-proBNP. We investigated the relationship between NT-proBNP and cardiac structure and function evaluated using cardiac magnetic resonance imaging (MRI), which is a substantially more accurate and reproducible method than echocardiography 8.
2.1. Patients
The study population comprised of 18 male and two female normal volunteers with no history or evidence of hypertension or cardiac disease, and 27 male and nine female patients with hypertension, electrocardiographic evidence of LV hypertrophy and preserved LV systolic function by echocardiography, included in the Losartan Intervention for endpoint reduction in hypertension (LIFE) study. For demographics see Table 1.
| Normal volunteers (n=20) | LIFE study (n=38) | P Value | |
|---|---|---|---|
| Sex (% men) | 90 | 71 | 0.10 |
| Mean (range) age (years) | 60.6 (54–79) | 63.8 (56 – 81) | 0.20 |
| Mean (S.D.) height (cm) | 176 (5.66) | 172 (9.14) | 0.07 |
| Mean (S.D.) weight (kg) | 79.7 (12.4) | 81.9 (13.7) | 0.55 |
| Mean (S.D.) BSA (m2) | 1.97 (0.15) | 1.95 (0.20) | 0.73 |
| Mean (S.D.) LVEDVI (ml/m2) | 54.6 (12.8) | 61.5 (13.1) | 0.06 |
| Mean (S.D.) LVESVI (ml/m2) | 16.9 (4.89) | 22.6 (9.69) | 0.02 |
| Mean (S.D.) LVMI (g/m2) | 90.0 (14.8) | 106 (19.5) | 0.003 |
| Mean (S.D.) LVEF (fraction) | 0.69 (0.06) | 0.64 (0.12) | 0.09 |
| NT-proBNP (pg/ml)* | 16.2 (2.10) | 158 (2.95) | <0.0001 |
- a BSA=body surface area; LIFE=Losartan intervention for endpoint reduction in hypertension; LVEDVI=left ventricular end-diastolic volume index; LVEF=left ventricular ejection fraction; LVESVI=left ventricular end-systolic volume index; NT-proBNP=N-terminal pro brain natriuretic peptide; S.D.=standard deviation.
- * Log analysis.
2.2. MRI examination
The patients were investigated at baseline, when they were free of antihypertensive treatment. LV end-diastolic (LVEDV) and end-systolic (LVESV) volumes were measured using MR cinematographic (CINE) short axis imaging. From this LV ejection fraction (LVEF) was calculated using the formula: LVEF=LVEDV÷LVESV/LVEDV. LV mass was measured from the stack of end-diastolic CINE short-axis slices covering the left ventricle as the area enclosed by the epicardial and endocardial borders of the myocardium multiplied by a density factor of 1.05. LV mass index (LVMI) was calculated using body surface area calculated from height and weight 9.
2.3. Blood sampling
Blood was taken at baseline, centrifuged immediately and plasma frozen at −80 °C. After thawing, the plasma was analyzed for NT-proBNP using the commercially available Elecsys proBNP sandwich immunoassay on an Elecsys 2010 (Roche Diagnostics, Mannheim).
2.4. Results
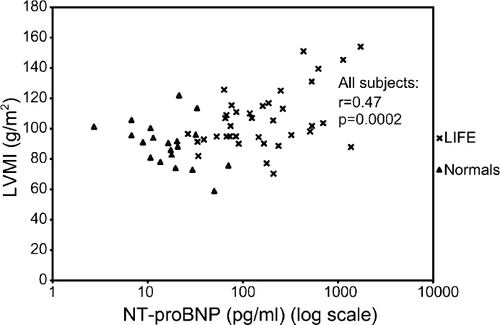
Demographic data for patients and normal controls are given in Table 1, LV dimensions and their relation to NT-proBNP are given in Table 2, and the association between LVMI and NT-proBNP is shown in Fig. 1. NT-proBNP was significantly higher in the LIFE patients than in the normal volunteers. There were no significant correlations between log NT-proBNP and any of the LV measures among the normal volunteers. In the LIFE patients, log NT-proBNP was significantly associated with LVMI (r=0.47, P=0.003), but not with any other LV measures. Overall, log NT-proBNP correlated with LVMI (r=0.47, P=0.0002), LVESVI (r=0.32, P=0.02), and LVEF (r=−0.25, P=0.06).
| Correlations with | Normal volunteers | LIFE study | All |
|---|---|---|---|
| log NT-proBNP | (n=20) | (n=38) | (n=58) |
| LVEDVI (r (P) values) | 0.22 (0.35) | 0.07 (0.69) | 0.18 (0.18) |
| LVESVI (r (P) values) | 0.24 (0.31) | 0.20 (0.23) | 0.32 (0.02) |
| LVMI (r (P) values) | 0.38 (0.10) | 0.47 (0.003) | 0.47 (0.0002) |
| LVEF (r (P) values) | −0.05 (0.85) | −0.15 (0.36) | −0.25 (0.06) |
- a LIFE=Losartan intervention for endpoint reduction in hypertension; LVEDVI=left ventricular end-diastolic volume index; LVEF=left ventricular ejection fraction; LVESVI=left ventricular end-systolic volume index; NT-proBNP=N-terminal pro brain natriuretic peptide.
2.5. Other studies
In a study using echocardiographic measurements Luchner et al. 10 demonstrated the value of NT-proBNP as a marker for LV mass, but with a large scatter of data. In the same study, BNP was significantly better than atrial natriuretic peptide (ANP) in predicting LV mass. In another LIFE sub-study of 180 patients a similar relationship between LV mass and NT-proBNP was demonstrated using echocardiography 11, but with a wider data scatter than our MRI sub-study found, probably due to a less accurate method for LV measurements. In the same study significant, but weak correlations were found between NT-proBNP and early systolic dysfunction as judged by midwall fractional shortening, and with some (E/A ratio, left atrial size) but not all (IVRT, deceleration time) echocardiographic surrogate measures of diastolic function. Regarding the mechanism for the increase in BNP/ NT-proBNP in patients with LV hypertrophy, it has been demonstrated that atrium-derived BNP is a significant predictor of LV mass index in patients with LV hypertrophy. The atrium-derived component contributes significantly to the elevation of plasma BNP/NT-proBNP, levels, probably reflecting atrial pressure and volume overload in LV hypertrophy, even in the absence of systolic dysfunction 12.
In a small study, Mussalo et al. 13 investigated BNP levels in patients with moderate renovascular hypertension and in patients with moderate and severe essential hypertension. The study demonstrated a four-fold higher BNP level in renovascular hypertension compared to patients with essential hypertension, while no difference was demonstrated between moderate and severe essential hypertension. The study was hampered by different blood pressure levels and different drug treatments in the three groups. Clarification of the diagnostic potential of BNP/NT-proBNP in renovascular hypertension awaits further studies.
3. Screening for hypertension/left ventricular hypertrophy
In population studies, patients with hypertension have a slightly or moderately elevated NT-proBNP plasma level compared with age- and sex matched volunteers without hypertension. In a recent report from the Framingham study 14 NT-proBNP appeared a useful method for screening for LV hypertrophy in the general population, but at a too high cost, due to a low prevalence of the disorder. In another report from the Framingham study, baseline BNP values in normotensive subjects did not predict development of hypertension four years later, and was only weakly associated with the risk of blood pressure progression 15.
4. Prognostic marker in hypertension
Information exists on the prognostic value of BNP or NT-proBNP in the general population, in patients with heart failure and in patients with acute coronary syndromes, while information on the prognostic value in other patient groups is generally sparse. In one small study Suzuki et al. 16 demonstrated a strong correlation between BNP and future cardiovascular events in patients with hypertension with and without LV hypertrophy.
- Low NT-proBNP and no known CVD: 4.3%;
- High NT-proBNP and no known CVD: 14.8%;
- Low NT-proBNP and known CVD: 18.2%; and
- High NT-proBNP and known CVD: 26.3%.
The differences between the groups were highly significant. Using NT-proBNP we were accordingly able to identify a low-risk group of approximately 1/3 of the patients in this otherwise high-risk group of patients with hypertension and electrocardiographic LV hypertrophy. Patients with an elevated NT-proBNP or known CVD had an approximately four-fold increase in event rate, while patients with a high plasma NT-proBNP as well as known CVD had a seven-fold increased risk. The strong prognostic value was still present with NT-proBNP measured after one year of treatment based on either a beta-receptor-blocker or an angiotensin-II receptor antagonist.
In addition, the prognostic value of NT-proBNP has been confirmed in another yet unpublished study. In a group of more than 200 unselected hypertensive patients with normal echocardiograms and without severe cardiovascular disease or diabetes, 3-year event rates were 2% and 11% in patients with NT-proBNP below or above the median value of 163 pg/ml, respectively.
In conclusion, available data suggest a strong prognostic value of NT-proBNP in patients with arterial hypertension.
5. Influence of treatment and treatment monitoring
For evaluation of a potential role for NT-proBNP in treatment monitoring, it is important to know the influence of different antihypertensive drugs on the plasma levels of the natriuretic peptides. As demonstrated in heart failure the Angiotensin II receptor blocker valsartan reduced the plasma level of BNP 18, and in the LIFE study the cardio-selective beta-blocker atenolol moderately increased the plasma NT-proBNP level. Studies in patients with heart failure have demonstrated similar changes during beta-blockade as well as a reduction in BNP/NT-proBNP levels during angiotensin converting enzyme (ACE) -inhibitor treatment 19,20.
No studies have been carried out to assess BNP/NT-proBNP as potential markers for treatment monitoring in patients with hypertension.
The finding that NT-proBNP even after one year of treatment was a strong prognostic marker suggests a role for NT-proBNP for monitoring even during aggressive treatment, but this clearly needs confirmation from prospective studies.
6. Conclusion
We have demonstrated that the plasma level of NT-proBNP is significantly increased in patients with essential hypertension and preserved LV systolic function compared to age- and sex matched normal volunteers. The plasma level of NT-proBNP partially reflects LV myocardial mass suggesting a potential role as a marker for LV hypertrophy in the evaluation of patients with essential hypertension.




