A novel method to rapidly calculate the urea clearance index and urea reduction rate based on parameters obtained during hemodialysis
Abstract
Background
The efficacy of hemodialysis (HD) is closely associated with patient survival time and quality of life. The classical method (CLM) to calculate the urea clearance index (Kt/V) and urea reduction rate (URR) requires multiple blood tests. A novel method that may be used as a noninvasive alternative to CLM is required.
Methods
Based on the urea kinetic model, a new method, named the “assessment method” (ASM), was established to calculate blood urea nitrogen after HD, based on parameters obtained during HD. The consistency of the Kt/V and URR values between the ASM and CLM was evaluated in 41 patients from the China–Japan Friendship Hospital between September 2017 and December 2018.
Results
Forty-one patients (24 males and 17 females; mean age, 55.7 ± 14.2 years) undergoing regular HD in our hospital were randomly selected for this study. The blood flow rate was 244.5 ± 19.6 mL/min and the dialysate flow rate was 500 mL/min. We obtained Kt/V (CLM = 1.40 ± 0.06, ASM = 1.37 ± 0.07) and URR (CLM = 68.6 ± 6.4%, ASM = 67.7 ± 7.2%) values. Paired t-test indicated no significant differences between the ASM- and CLM-derived values. The intraclass correlation coefficients were 0.907 and 0.916 for Kt/V and URR, respectively. Similarly, Bland–Altman plots suggested good concordance between the 2 methods.
Conclusions
The Kt/V and URR values calculated using the ASM and CLM were in significant agreement, and both can be used to effectively assess the adequacy of HD in patients undergoing maintenance HD. The ASM is an effective, rapid, inexpensive, and noninvasive alternative to the CLM for obtaining Kt/V and URR values. The ASM has good potential for clinical application, particularly for patients in areas of low socioeconomic status.
Introduction
Chronic renal failure (CRF) is the endpoint of many primary and secondary renal diseases. Renal replacement therapies, including renal transplantation, hemodialysis (HD), and peritoneal dialysis, are the most effective treatments for end-stage renal disease. Most CRF patients in China choose HD for renal replacement.1 The efficacy of HD is closely associated with patient survival time and quality of life.2,3 The urea clearance index (Kt/V, where K = dialyzer clearance of urea, t = dialysis time, and V = volume of distribution of urea) and urea reduction rate (URR) are the 2 most important indices for evaluating the adequacy of dialysis.3,4 These calculations are based on blood urea nitrogen (BUN) concentrations taken before and after dialysis. The classical method (CLM) of obtaining these values, based on the second-generation Daugirdas formula,5,6 is the most widely used method in clinical practice. However, serum samples must be collected from patients before and after dialysis and the BUN level must also be determined. Poor patient compliance with multiple blood draws and the high cost of repeated tests are the main barriers to frequent monitoring.
In this study, based on the urea kinetic model, we propose a novel method, which we call the “assessment method” (ASM), to calculate BUN after HD using parameters obtained during HD. The urea nitrogen ratio before and after dialysis can be used in the Kt/V and URR calculations. Although the ASM is not a simpler model for calculating normalized urea clearance, it is suitable for resource-limited regions. The cost of HD blood tests accounts for approximately 10% of the total cost of a single HD treatment. This is expensive for patients in areas of low socioeconomic status, particularly if they are required to pay for their own treatments.7 This is also the main reason for the reduced frequency of monitoring. The ASM effectively reduces the number of blood tests required and facilitates the monitoring of dialysis efficiency.
Methods
Ethical approval
This was an observational study. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and the Helsinki Declaration of 1975, as revised in 2013.
Modeling
The local urea dynamic model was proposed by Schuneditz et al in 1993.8 According to blood flow/water content, this model classifies human organs into organs with a high blood volume and low water content and those with low blood flow and high water content. During HD, it is assumed that organs with high blood flow and low water content receive 85% of the total body blood flow and contain 20% of the body fluid volume, while organs with low blood flow and high water content receive 15% of the total body blood flow and contain 80% of the body fluid volume. The calculation principles and processes are as follows:
 (Eq.(A.1))
(Eq.(A.1)) (Eq.(A.2))
(Eq.(A.2)) (Eq.(A.3))
(Eq.(A.3))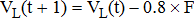 (Eq.(A.4))
(Eq.(A.4))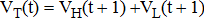 (Eq.(A.5))
(Eq.(A.5))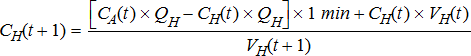 (Eq.(A.6))
(Eq.(A.6))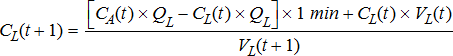 (Eq.(A.7))
(Eq.(A.7))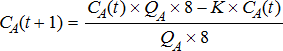 (Eq.(A.8))
(Eq.(A.8)) (Eq.(A.9))
(Eq.(A.9))Finally, the BUN before and after HD can then be substituted into the formula to calculate the values of Kt/V and URR. An online computing webpage based on the above principles was designed (http://www.ifmsoft.com.cn/i-DiaProKtV.html). First, the left column of the website was filled with the patient's most recent laboratory test and HD parameters. Then, the right column with HD parameters of the current and the values of Kt/V and URR were obtained directly.
Model validation
Patients undergoing maintenance HD who were admitted and treated at the China–Japan Friendship Hospital from September 2017 to December 2018 were selected for inclusion in this study. The inclusion criteria were as follows: 1. patients between 18 and 80 years of age; 2. maintenance HD for more than 3 months; 3. internal arteriovenous fistula was used to complete the HD treatment; and 4. blood flow of 200–300 mL/min. The exclusion criteria were as follows: 1. incomplete renal function test data before and after HD; 2. poor condition of the internal fistula or unstable intradialytic blood flow; 3. high metabolic conditions, such as tumor and acute infection, etc.; and 4. a lack of consent to participate in the study.
First, after patient enrollment, the BUN levels before and after HD in the patient's most recent routine laboratory tests and HD parameters during the current laboratory testing were used to calculate the required intermediate parameters. These parameters were then used to calculate the Kt/V and URR values of dialysis.
For CLM, BUN levels before and after HD were directly obtained by blood sample tests, and Kt/V and URR values were calculated using the classical formula.
For ASM, the BUN before HD in the patient's most recent laboratory test results and the dialysis parameters, including dialysis time, ultrafiltration volume, and urea clearance coefficient, were extracted and filled in the appropriate spaces in the left column of the website (http://www.ifmsoft.com.cn/i-DiaProKtV.html). Dialysis parameters of the current dialysis, including dialysis time, ultrafiltration volume, blood flow, and urea clearance coefficient of the dialyzer were filled in the appropriate spaces in the right column of the website (http://www.ifmsoft.com.cn/i-DiaProKtV.html), and the values of Kt/V and URR were obtained directly.
Statistical analyses
Statistical analyses were performed using SPSS 17.0 (IBM Corp., US). Normally distributed variables were expressed as mean ± standard deviation (SD), whereas non-normally distributed variables were expressed as median (lower quartile, upper quartile). Pairwise comparisons were made using paired t-tests for normally distributed data and the concordance test of the 2 methods was performed using intra-class correlation coefficients (ICC) and Bland–Altman plots. Statistical significance was set at P < 0.05.
The Bland–Altman plot is a graphical method for the comparison of 2 measurement techniques. In this graphical method, the differences between the 2 techniques are plotted against the averages of the 2 techniques.
Results
Basic characteristics of enrolled patients
Forty-one patients who underwent regular HD at the China–Japan Friendship Hospital and met the inclusion and exclusion criteria were randomly selected; the cohort contained 24 males and 17 females with a median age of 55.7 ± 14.2 years. Among the enrolled patients, 87.8% (36/41) had anemia, 39.0% (16/41) had coronary artery disease, 19.5% (8/41) had cerebrovascular disease, 82.9% (34/41) had hypertension, 51.2% (21/41) had diabetes mellitus, and 22.0% (9/41) had chronic obstructive pulmonary disease. The average BUN level before HD was 63.6 (57.2–81.0) mg/dL and after HD was 22.31 (15.7–28.9) mg/dL. HD time ranged from 3.5 to 4.0 h; the average blood flow was 244.5 ± 19.6 mL/min; the dialysate flow rate was 500 mL/min; the average ultrafiltration volume was 2.6 (1.6–3.3) L; the average body weight after dialysis was 64.4 (52.7–75.6) kg.
Concordance test between CLM and ASM
The BUN results for patients before and after dialysis were substituted into the second-generation Daugirdas formula to obtain Kt/V (CLM) = 1.40 ± 0.06. The relevant parameters of the HD process were substituted into the model to obtain Kt/V (ASM) = 1.37 ± 0.07. A paired t-test showed no significant difference between the 2 groups (t = - 1.902, P = 0.064). A concordance test suggested good data consistency between the methods (ICC = 0.907). To further intuitively assess the detection consistency of the 2 methods, we constructed a Bland–Altman plot (Fig. 1A), which showed that only 3 sets of data (3/41, 7.3%) were located outside the 95% consistency limit. When comparing the ASM with the CLM, the absolute value of the maximum difference was 0.25, and the mean difference was 0.03.
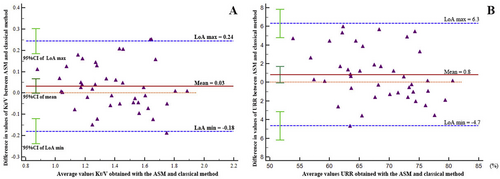
Analysis of the consistency of values obtained with the ASM and CLM using a Bland–Altman plot. A: urea clearance index (Kt/V); B: urea reduction rate (URR). ASM: assessment method; CLM: classical method.
The results obtained directly through the blood test and the results calculated according to the ASM are introduced into the formula to calculate URR. The values were 68.6 ± 6.4% and 67.7 ± 7.2%, respectively. A paired t-test showed no significant difference between the 2 groups (t = − 1.890, P = 0.066). A concordance test suggested good data consistency between the 2 methods (ICC = 0.916). A Bland–Altman plot was then constructed (Fig. 1B) which showed that all data were located inside the 95% consistency limit. When comparing the ASM with the CLM, the absolute value of the maximum difference was 6.0, and the mean difference was 0.8.
Discussion
The Kt/V and URR values have been recognized globally as the most important indicators for quantifying and monitoring the efficacy of dialysis.9,10 The traditional calculation of these values relies on BUN data from before and after each HD session. If Kt/V and URR need to be monitored, repeated blood sampling is required; otherwise, it is impossible to rapidly obtain the new value in a timely manner.
The results of this study show no significant difference between the ASM and CLM of calculation and the 2 methods had good consistency. The values of Kt/V and URR obtained with the ASM were slightly lower than those obtained using the CLM. This may be related to the fact that the CLM utilizes a one-compartment Kt/V model, which treats the body as a single compartment with an even distribution of solutes and ignores variables such as urea production and volume change during dialysis, as well as the intercompartmental transport coefficient of solutes, leading the CLM to overestimate the actual clearance amount. In addition, after dialysis is completed, urea with an unbalanced distribution between compartments slowly diffuses from a high-concentration compartment to a low-concentration compartment, referred to as the urea rebound phenomenon.11 Thus, the blood sample collected at the end of dialysis under uneven urea distribution conditions underestimates the BUN concentration, causing the calculated Kt/V and URR to be higher than actual values.
China's Clinical Practice Guideline for HD Adequacy12 published in 2015 recommends monitoring of the Kt/V and URR values once every 3 months, or once every month for HD centers where conditions permit. However, in reality, due to practical limitations, such as economic conditions, monitoring can only be performed once every 6 months in some regions, which is much lower than the standard recommended by guidelines in the United States10 and Europe.9
Patients in some areas refuse regular blood tests unless their life is threatened, and the HD machines in these areas often lack online clearance monitoring (OCM).13,14 Therefore, a large number of patients are in danger due to a lack of effective monitoring, which is associated with increased complications and a poor quality of life. We reported the preliminary results of the concordance between ASM- and CLM-derived parameters. The test suggested good consistency between the 2 methods. In the future, we plan to directly compare the ASM with the OCM to further verify the accuracy and reliability of the ASM.15
The ASM has a limitation in that changes in BUN over time may result in inaccurate Kt/V and URR values; therefore, we are currently conducting a longer-term evaluation of the ASM and CLM. In this study, the sample size was small and insufficient to draw exact conclusions. A multi-center clinical validation study with a larger sample size and more rigorous design is currently in progress.
Overall, this urea kinetic model-based assessment method simulates the dynamic process of toxin removal during dialysis. The ASM is an effective, rapid, inexpensive, and noninvasive alternative to the CLM for obtaining Kt/V and URR values. In future clinical practice, especially in HD departments in basic clinics and poor areas, the ASM has good clinical application potential and value.
Funding
This study was supported by a grant from Transverse Research Project of China-Japan Friendship Hospital (No: 2017-HX-9).
Conflicts of interest
None.