Unmet needs as indicator of improving chronic care delivery system in China
Abstract
In 2009, China strengthened its public health service system. Since then, the country has made remarkable achievements in community-based chronic disease prevention and control; however, certain groups still have unmet needs. During 2019 to 2029, China will consolidate the top-level design of its medical health system. During this period, the coordination of department policies, improvement of service delivery mechanisms, building an integrated health service system, and other issues will be highlighted. This study will provide a basis for designing China's chronic disease prevention and control system during the next stage of development. We will consider the unmet needs of patients with chronic diseases as an indicator for remodeling the prediction system in combination with the elements and structural theories of complex health systems. In this article, we first introduce the definition and measurement methods of unmet needs. Second, we identify the existing unmet needs found among patients with chronic diseases with reference to the chronic disease prevention and control policies of China as well as current service items. Finally, we propose the design of community chronic disease service package for the next development stage based on unmet needs of patients with chronic diseases. We also provide suggestions for how to improve China's chronic care delivery system.
Introduction
According to the definition of the World Health Organization (WHO), the term chronic diseases (the complete term is noncommunicable chronic diseases) refers to diseases that persist for a long time and are caused by the combined effects of genetic, physiological, environmental, and behavioral factors among others.1 Aging of the population and changes in individuals’ lifestyles, dietary habits, and work modes are producing increasingly more obvious impacts on health, and both incidence and mortality owing to chronic diseases are on the rise each year.2 According to the Report on the Nutrition and Chronic Diseases of Chinese Residents released by the National Health and Family Planning Commission of China in 2015, about 30% of the population in China has some type of chronic disease. In 2012, the mortality rate in Chinese residents with chronic diseases was 533 per 100,000. The percentage of deaths owing to chronic diseases over total deaths reached 86.6%, rising every year at a rate of 8.9%.3 Owing to the large number and high growth rate of patients with chronic diseases and the surge in medical expenses arising from chronic diseases, China is poised to enter a period of high economic burden caused by chronic diseases.4
Since 2009, the Chinese government has begun to systematically lay the foundations for a community-based network of chronic disease prevention and control and health services in its new medical reform planning. Some scholars have reviewed policies related to the prevention and control of chronic diseases issued by the government of China from 1984 to 2014. Among the 164 related laws and policies, no more than 2 were issued each year, on average, before 2000; however, an average 9 to 29 laws or policies were issued after 2009.5 Nevertheless, studies conducted in recent years have pointed out that chronic disease prevention and control “has a high standard in policy formulation but ends in poor implementation”; no effective monitoring and constraint systems have been established during policy implementation, and multi-sector cooperation is unsustainable, making it difficult to meet the requirements for long-term prevention and control of chronic diseases.6,7 Additionally, in the report from Innovative Care for Chronic Conditions issued by the WHO in 2005, it was suggested that because public health care systems that have evolved around the concept of acute conditions are unable to satisfy the health needs of many patients, especially those with chronic diseases, different types of public health systems are imperative for effective chronic disease prevention and control.8 Owing to the inadequate design of chronic disease prevention and control policies, incomplete chronic prevention and control service delivery systems, and low rates of application and promotion of these policies and systems in China, the needs of many patients with chronic diseases have not been met.2
Unmet needs is an indicator that is widely used to evaluate the service capability of a medical health system, as it relates to health outcomes, financial risk protection, improvement in efficiency, and responsiveness to individuals’ reasonable health expectations.9 It is beneficial for chronic disease prevention and control policy makers to determine priorities by accurately identifying and measuring the unmet needs of patients with chronic diseases10 and to better target chronic disease prevention and control policies.11 Hence, in this study, we provide suggestions for how to design a system of chronic care delivery in the public health system during the next development stage in China.
Unmet needs
Definition of unmet needs
Currently, no consensus has been reached on the definition of an unmet need in terms of policy. Fillenbaum et al12 was the first to propose the term unmet need that was used to assess the welfare of older adults. In recent years, further advancement has been made in academic circles with respect to research on the definition of an unmet need. Foot et al13 believed that unmet needs refer to medical treatment needs that cannot be met and solved through health service delivery in real-life settings, as reflected in patients’ clinical indicators and subjective needs of patients. Allin et al14 defined unmet needs as failure of an individual to have their need met for access to clinical or medical treatments that can improve their health conditions. From the perspective of whether individuals can obtain benefits, Harrison et al11 conceptualized the definition of unmet need as a situation in which individuals or groups fail to obtain benefits for various reasons, although they may do so from interventions or health service delivery. Reeves et al15 defined unmet need as the inability of individuals to receive medical treatment when they believe they have a medical need. Cohen et al16 believed that an unmet need is generally defined as insufficient availability and adequacy of drugs or other medical solutions. For example, drugs to treat some diseases do not exist, or, despite their existence, medical solutions become ineffective in their delivery mechanism or formulation.
By referring to the definitions of unmet needs given by the above scholars, we defined the unmet needs of patients with chronic diseases as needs that are not met by the local chronic care delivery system among the objective needs proposed by patients with chronic disease for prevention, medical treatment, rehabilitation, and health care according to gaps between their actual health conditions and their subjective ideal health status.
Measurement of unmet needs
Scholars have adopted different methods to measure unmet needs. Among these, Cavalieri et al17 pointed out that subjective evaluation by patients can better reflect their actual unmet needs than evaluation using clinical indicators. Subjective evaluation should be based on the assumption that patients best know their own health condition and are able to judge whether they have received the best medical services. In terms of measurement tools, self-report questionnaires or disease-specific scales have been adopted in many studies of unmet needs. This type of research generally analyzes the existing status of unmet needs among respondents and potential-influencing factors. For example, Pappa et al18 investigated the unmet needs in primary health care among a representative population of Greece.
Another method for measuring unmet needs is to use data retrieved from open-access databases such as that of the National Bureau of Statistics. For example, Vlachantoni et al19 used publicly available data from longitudinal research on aging in the United Kingdom and from the Special Survey on British Families to analyze the level of unmet needs in older people aged 75 years and above. In addition to subjective evaluation, questionnaires, and open-access databases, some scholars have suggested using the burden of disease or disability-adjusted life years (DALYs) to measure unmet needs.11
As seen from the above, there are many ways to measure unmet needs. Regardless of the method, it is necessary to consider the assumptions made in using a particular measurement method and the accuracy of the analysis process. Only by correctly identifying and measuring true unmet needs can positive impacts be made on the design of chronic disease prevention and control policies in China for the next development stage.
Current condition of China's chronic care delivery system
With respect to chronic disease prevention and control management, China has started from scratch and has undergone a process of transition from partial to overall improvements. The focus has been shifted from specific disease prevention and control to risk factors. A chronic disease prevention and control strategy has been established that prioritizes prevention, combines prevention and control, and shifts the focus of work. An integrated care delivery system that features government regulation, multi-sector collaboration, and full involvement has been developed.20 Here, we propose new strategies and measures for unsuitable aspects of the system by reviewing important policies on chronic diseases established since the implementation of the new medical reform plan of China in 2009. We sought to better understand the development trajectory of China's policies on chronic disease prevention and control and the service items in this regard to further improve China's chronic care delivery system.
Important policies on chronic disease prevention and control since China's medical reform
Since 2009 when China began its medical reform, the National People's Congress, the State Council, and related departments have formulated and implemented a series of public policies that are beneficial for the prevention and control of chronic diseases. Among these, policies that have produced major impacts on the system of service provision for the prevention and control of chronic diseases are shown in Table 1.
| Year | Policy | Related content of chronic disease care delivery |
|---|---|---|
| 2012 | China's Plan on the Prevention and Treatment of Chronic Diseases (2012–2015) | The plan proposes the cross-sector coordination mechanism featuring “government-led, multi-sector cooperation” and the development strategy of “integrating health into public policies.” 62 |
| 2015 | Guiding Opinions on Promoting the Building of the Graded Diagnosis and Treatment System | Chronic diseases such as hypertension, diabetes, tumors, cardiovascular, and cerebrovascular diseases are identified as focuses and graded diagnoses, and treatment is developed with the medical consortium as the starting point.63 |
| 2016 | Outline of “Healthy China 2030” Plan | It is necessary to control and prevent key chronic diseases. It is required to shift the focus of medical and health industry from disease diagnosis and treatment to prevention orientation and the combination of prevention and control, highlight the support on the building of primary medical and health service systems, and prevent and control diseases, especially chronic diseases based on community medical care.64 |
| 2016 | Thirteenth Five-Year Plan on Health and Wellness | It is necessary to enhance the building of national comprehensive prevention and control demonstration zones, make more efforts on screening and early detection of chronic diseases, improve monitoring of all causes of death, tumor registration reporting, and chronic disease and nutrition monitoring systems.65 |
| 2017 | China's Medium- and Long-term Plan for the Prevention and Treatment of Chronic Diseases (2017–2025) | Multi-sector cooperation is officially written into the chronic disease prevention and control plan. The health and family planning authorities are instructed to implement the plan and carry out supervision and evaluation in conjunction with other relevant departments. Among them, the development and reform authorities shall include chronic disease prevention and control in the economic and social development plan, and the financial authorities shall allocate relevant funds in place; and the human resources and social security authorities shall further improve the outpatient-related security policies and payment mechanism.66 |
| 2017 | Guiding Opinions on Promoting the Building and Development of Medical Consortia | Emphasize the promotion of the combination of prevention, treatment, and management of chronic diseases and promote the linkage among the building of medical consortiums, prevention, and health care.67 |
| 2019 | Opinions of the State Council on Implementing “Healthy China” Action | Prevent and control chronic diseases such as cardio-cerebrovascular diseases, chronic respiratory diseases, and diabetes; carry out comprehensive intervention of the factors that influence health; and take reasonable dietary actions, all-round fitness actions, and tobacco control actions.68 |
| 2020 | Opinions of the CPC Central Committee and the State Council on Deepening the Reform of the Medical Security System | Vigorously promote the application of big data, support the development of new models such as “Internet + medical treatment.” For diseases involving long-term hospitalization such as medical rehabilitation and chronic mental diseases, the bed costs should be paid by the day. For special outpatient chronic diseases, payment should be made according to the number of patients.69 |
In addition to these important policies directly related to chronic disease prevention and control, the State Council and other competent authorities have released a series of laws, regulations, or documents that have been beneficial for chronic disease prevention and control as improvements to the medical reforms, such as the National Standards for the Prevention and Control of Chronic Diseases in China, Several Opinions on Facilitating the Development of the Health Service Industry, Decisions on Strengthening Aging-Related Work, and Outline of China's Food and Nutrition Development (2014–2020) among others. Establishment of these laws, policies, regulations, and other related documents has provided strong support for the prevention and control of chronic diseases in China, allocating tasks in chronic disease prevention and control to various departments and shifting the focus of work from disease treatment to health management as well as integrated prevention and control.7
Although the Chinese government has issued many policies that are beneficial for development of its chronic disease prevention and control system, many issues remain. Zhang et al21 indicated that government-led multi-sector cooperation has only just begun; the environment of national policy support has not been yet fully formed. There is a lack of sustainability in multi-sector cooperation; human and financial resources as well as full public support are insufficient for chronic disease prevention and control, and specific implementation still confronts many challenges. Li et al22 showed that although the Chinese government has released many policies regarding chronic disease prevention and control, no concerted effort regarding these mechanisms has been made, and there is no consensus among members of Chinese society that preventing chronic diseases is a responsibility of the society. A huge gap remains in the development, perfection, unification, and sharing of a health information platform based on the information of residents in China. Thus, chronic disease prevention and control policies for the next development stage require further multi-sector coordination and cooperation, concerted support from all members of Chinese society, and long-term sustainability to conform to the characteristics of long cycles of chronic diseases.
Services provided by the existing China's chronic care delivery system
Since China implemented its medical reform plan in 2009, chronic disease management of patients with hypertension, diabetes, and severe mental disease has been included in the national basic public health service project. The services provided for the prevention and control of chronic diseases as part of national basic public health services are shown in Table 2.23
| Chronic diseases | Target population | Service items | Assessment indicators |
|---|---|---|---|
| Hypertension | Permanent residents suffering from primary hypertension and aged 35 years and above in their jurisdictions | Screening and behavioral intervention for hypertension; establishing health records for patients with confirmed hypertension; establishing a follow-up registration form and making at least four face-to-face visits per year; offering targeted education to all patients (including physical exercise, salt intake, and drinking); organizing patients to receive one health examination every year (including physical examination, auxiliary examination) | For residents aged 35 and above, initial visit pressure measurement rate;patients' filing rate, health examination rate, and need control rate |
| Type 2 diabetes | Permanent residents suffering from type 2 diabetes and aged 35 years and above in their jurisdictions | Type 2 diabetes screening and behavioral interventions; establishing health records; follow-up interventions (including measurement of blood glucose and blood pressure, measurement of weight, health education); health examinations (including physical examinations, auxiliary examinations) | Patients' record establishment rate, health examination rate, standardized management rate, and blood sugar control rate |
| Severe mental diseases | Residents who are clearly diagnosed with mental diseases and live at home in their jurisdictions | Providing full-time (part-time) personnel who have received training related to the management of severe mental diseases, conducting related health management work; establishing health records for patients with newly discovered severe mental diseases in their jurisdictions and update the records on time; making appointments for outpatient visits, following up patients by phone, making door-to-door visits; encouraging and assisting patients in rehabilitation training; guiding patients to participate in social activities and receive vocational training | Management rate of patients with severe mental diseases, standardized management rate of patients with severe mental diseases |
Health management services for patients with chronic diseases in the basic public health service package have played an important role in controlling the development of chronic diseases in China. The rate of standardized management for chronic diseases such as hypertension and diabetes has witnessed a significant increase.24 Community-based standardized management of chronic diseases involves health education, disease screening, creating health record, disease intervention and treatment, follow-up, rehabilitation, patient self-management, and other elements. Long-term standardized management can help control the onset of chronic disease, delay the process of disease progression, and improve quality of life among patients.
Unmet needs among patients with major chronic diseases in China
Although China's chronic diseases services delivery system provides screening, behavioral intervention, health education, health examination, and other services for patients with chronic diseases, there is a low rate of utilization of these services by patients that results in many unmet needs in the prevention and control of chronic diseases.25 Hypertension, diabetes, chronic obstructive pulmonary disease (COPD), and severe mental diseases are the most commonly seen chronic diseases with the widest range of influence, and these involve the highest disability and mortality rates as well as the heaviest socioeconomic burden.26,27 Thus, by reviewing the unmet needs of patients with these four types of chronic disease, we can further improve the design of a service package toward perfecting China's chronic disease prevention and control service delivery.
Unmet needs among patients with hypertension
Feng et al28 explored the current status of health service needs among patients with chronic diseases in the community using the Community Client Need Classification System (CCNCS); by selecting questionnaires from 240 patients with chronic diseases in three community health service centers, the author indicated that patients with hypertension have higher levels of unmet needs with respect to care evaluation, health education and promotion, and psychosocial needs compared with other patients groups, and this is owing to the high level of patients’ needs in these three areas. Han et al29 showed that the needs of community-dwelling patients with chronic diseases with respect to disease control, disease prevention, and health promotion accounted for 88.0%, 83.1%, and 75.5% of their total needs, respectively; however, the service delivery rates for these three aspects were 20.2%, 23.4%, and 16.4%, respectively. In addition, results of study on continuing care needs of elderly hypertensive patients show that the demand for better health promotion of prevention guidance, drug knowledge, and safe medication guidance is still as high as 71.86%.30 Ruddy et al31 stated that despite the adequate availability of antihypertension drugs, safer and more effective antihypertension solutions are needed. Thus, unmet needs remain for patients with hypertension with respect to antihypertension drugs and solutions.
Unmet needs among patients with diabetes
In 2013, one in four people with diabetes worldwide were in China, where 11.6% of adults had diabetes and 50.1% had prediabetes. Many were undiagnosed, untreated, or uncontrolled.32 In addition, community health care center physicians provided insufficient guidance to patients in terms of drug utilization and prevention of complications. Research of Corinne et al33 identified unmet needs of patients with type 2 diabetes in psychosocial care, such as no additional diabetes education, management of diabetes in patients, and counseling services; these needs were only met when patients were satisfied with the delivery of community-based chronic disease prevention and control services. In addition to unmet health services for patients with diabetes, caregivers have unmet health needs. Using a self-reported self–efficacy scale administered to caregivers of patients with type 2 diabetes, Mcewen et al34 found that caregivers had a desire for community-based medical assistance and a need for social support. These unmet needs should not be ignored in research among patients with diabetes in this regard; unmet needs of caregivers in terms of professional knowledge and psychological support directly affect the health needs of patients.
Unmet needs among patients with chronic obstructive pulmonary disease (COPD)
Among the major chronic diseases affecting human health in China, COPD ranks third in terms of cause of death and second in terms of overall burden of disease, following hypertension and diabetes. There is clearly insufficient awareness and attention paid to COPD in all sectors of the community, presenting a serious situation for prevention and control.35 Xu et al36 found that COPD is still not included in China's national chronic disease prevention and control system; no adequate support in terms of national policies is provided toward the prevention and control of COPD. Pulmonary function testing, an effective tool for the diagnosis of COPD, is not included as part of the standardized list of tools and related equipment needed in community health service centers. There are inadequate supplies of drugs to treat respiratory diseases in community health centers, and physicians have poor skills in diagnosing and treating COPD. Thus, patients with COPD in China have unmet needs in terms of prevention, diagnosis, and treatment. Research results of Peng et al37 showed that among community health service centers, 27.1% conducted COPD screening, 2.1% had established records of patients with COPD, 12.5% carried out COPD follow-up, 14.6% offered COPD health education, and 12.5% conducted training in COPD for medical staff. These indicators were all lower than those of institutions providing management of hypertension and diabetes.
Unmet needs among patients with severe mental diseases
Hunter et al38 found that severe depression and dementia among older people became the research frontier in the field of health management. Currently, the prevention of depression, dementia, and other severe mental diseases among older people, as well as counseling, are only carried out using a single form of health education with little effectiveness. The needs of individuals with mental diseases have thus failed to be satisfied. Dong et al39 found that community-based management of patients with severe mental diseases features insufficient human resources, inadequate support, and high mobility of team members. Hence, the needs of patients with severe mental diseases for disease management consultations have gone unmet, and these patients have low compliance with health management. The research of Li et al40 indicated that because of social prejudice and discrimination, inadequate management capacity of primary health care centers, and lack of professional and full-time medical staff, financing, and policy support, the rates of prevalence, standardized management, medication, and medication compliance are all far lower than the relevant requirements. This indicates that a large gap remains between the increasing service needs of Chinese patients with severe mental diseases and diagnosis, treatment, and management services provided.
Using the information regarding unmet needs among patients with hypertension, diabetes, COPD, and severe mental diseases, the current unmet needs of patients with chronic diseases in China can be expected to include those regarding care assessment, health education and promotion, psychosocial support, therapeutic drugs, behavioral interventions, professional training, psychological counseling for patient caregivers, and professional full-time management of medical staff among others. In particular, patients with severe mental diseases and COPD have many unmet health needs. In the next development stage, the health needs of these two patient groups should be highlighted in the design of China's chronic disease prevention and control service package.
Causes of unmet needs among chronic diseases patients in China
The fact that people are using the basic health services currently provided by the state does not mean that their needs are being systematically or adequately met if they encounter obstacles in accessing specific services and (may) delay or abandon the idea of finding the service they think they need; they may not be able to (completely) meet their needs. According to data from the national health surveys of the European Union and Organisation for Economic Cooperation and Development (OECD) countries, the main reasons for unmet health needs include long waiting times, small number and distance of health services, and personal financial problems.41
Causes of unmet needs among China's chronic disease patients in micro level
Chronic disease is a long-term process that is closely related to the lifestyle of the individual. Based on the study of the causes of chronic diseases in China, physical exercise, smoking, salt intake control, vegetable consumption, and other personal habits have a greater impact on the prevalence of chronic diseases.42 Additionally, Laura et al,43 through the REACH U.S. Risk Factor Survey where approximately 3001 Chinese individuals from high-density Asian American New York City areas were included, found that the elderly chronic disease prevalence rate and low degree of cultural crowd chronic disease prevalence are especially high and that there is a higher degree of unmet needs, mainly because the elderly and the less educated people lack the knowledge on hypertension prevention and control, and the awareness rate is low. Hence, patients with chronic diseases cannot play their active role in blood pressure management. Therefore, part of the reason why Chinese patients with chronic diseases cannot meet their health needs is that their knowledge on prevention and control of chronic diseases and their health literacy need to be improved.
Causes of unmet needs among China's chronic disease patients in medium level
The quantity and quality of the supply of doctors and nurses from community health service centers as providers of chronic disease services will affect the satisfaction of needs of patients with chronic illness. However, there are some problems in the staffing of community health service centers in China, such as less experience, fewer staff, lower education, lower professional title, and lower salary.44 Li et al45 pointed out in the analysis of the abnormal loss of human resources in community health service centers that owing to the limited number of staff, no autonomy, no promotion channels, and low position treatment, it leads to serious shortage of general practitioners and public health and clinical nursing staff and high rate of initiative loss that directly affects the development of “six in one” health service in community health service centers. Overall, most trainings did not achieve the expected results, as they lacked training knowledge in preventive health care, rehabilitation, and health education in the community. The shortage of personnel has been aggravated by the serious problems such as the mismatch between the training content and actual work needs, short training time, repetition of the training content, and lack of guidance.46
Causes of unmet needs among China's chronic disease patients in macro level
Although the government's attention and years of experience have provided certain conditions for the prevention and control of chronic diseases in China, there is a lack of multi-sector cooperation mechanisms and macro-policy breakthroughs, chronic disease prevention and control technology research projects, or pilot ways to carry out a planned exploratory research.47 The lack of research and analysis on the rationality, controllability, and manageability of technologies and measures for the prevention and control of chronic diseases has resulted in the lack of theoretical guidance in the promotion of these measures, resulting in a waste of human and material resources and low efficiency. In turn, the existing services cannot meet the needs of patients with chronic diseases. Therefore, the next stage of China's chronic disease prevention and control system from the macro-level is to form a set of mature chronic disease prevention and control technology and measures of theory and policy.
Design of China's chronic care delivery system for the next decade
Chronic disease prevention and control framework integrating individuals, institutions, and policies
Unmet needs for the prevention and control of chronic diseases in China involve patient, community, and policy levels. Currently, China's chronic disease prevention and control organizations have challenges such as an incomplete institutional system, insufficient institutional collaboration, inadequate discipline coordination, and poorly connected service links.40 According to the organizational framework at micro, middle, and macro levels of WHO's Innovative Care for Chronic Conditions, each level is not independent but rather interacts with the others. These levels do not have clear boundaries. Only through the effective advancement and successful operation of the three levels can multiple sectors in China's chronic disease prevention and control system satisfy the needs of patients with chronic diseases.8 The relationships among the micro, middle, and macro levels are shown in Fig. 1.
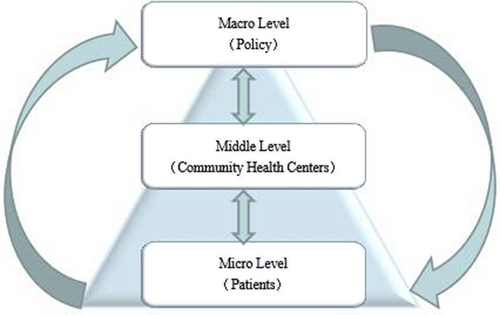
Organizational framework of chronic disease prevention and control system.
In this organizational framework, needs at micro, middle, and macro levels are met, population disease control is prioritized, and prevention is highlighted. As the largest differences are between chronic diseases and other diseases, the former has a long cycle of prevention and control, and the development of chronic disease is highly correlated with the daily lifestyle habits of patients. Thus, the three elements of patients at micro level, community health centers at the middle level, and policies at macro level must be combined to function effectively. When concerted efforts are made among these three elements, patients and caregivers become the main participants in prevention and control of chronic diseases under the guidance of community health centers and polices, and there are good communications between patients and community health centers. This way, the unmet needs of patients and patient caregivers will be greatly reduced.
Chronic disease prevention and control service package
Because the management of diseases such as hypertension, diabetes, COPD, and severe mental diseases shares similar service items and processes,26 we designed a service package for China's chronic disease prevention and control system in the next decade according to the framework above, at micro level (patients with chronic diseases), middle level (community health centers), and macro level (policies), as described in the Innovative Care for Chronic Conditions of the WHO.8
Micro level (patients with chronic disease). Because patients with chronic diseases must change their lifestyles and participate in self-management of their own health, they cannot be regarded as passive recipients of chronic disease prevention and control services. There is much evidence showing when patients take actions in caring for themselves, such as taking medicine, following physician's instructions, engaging in exercise, or quitting smoking. The health effects produced in these patients are far superior to those yielded via medical interventions.48,49 During the next development stage, China should focus on the important and positive role of patients in the design of its chronic care delivery system.
Middle level (community health centers). Much remains to be improved in the service capabilities of community health centers in providing adequate chronic disease services, such as regular in–home visits, disease screening, and health education.50 Therefore, increasing the number of health staffs and professional capabilities of chronic disease management personnel should be highlighted in the design of the service package for chronic disease prevention and control at the middle level in the next development stage.
Macro level (policies). The macro policy environment must inevitably be considered in the decision-making and planning for chronic disease prevention and control. In response to inadequate drug solutions for patients with chronic diseases, adequate professional capabilities of community health centers and effective disease prevention efforts should be designed at the policy level in the service package. Chronic disease service items at the micro, middle, and macro levels are shown in Table 3.
| Chronic disease delivery system | Service target | Service items |
|---|---|---|
| Micro level (patients) | Improve the control rate of chronic disease patients and the awareness toward chronic disease knowledge | Strengthen chronic disease management knowledge education and improve health literacy |
| Make patients active participants in chronic disease management and increase their compliance | Guide patients to set clear self-management goals | |
| Meet the psychological support and listening service needs of patients and their caregivers in a timely manner | Enable patients and their caregivers to have access to information and autonomous management support outside community health centers by phone or Internet | |
| Collect more real and accurate patient data to provide patients with accurate chronic disease management services | Design patient self-assessment questionnaires using Internet apps or applets to generate personalized self-management materials | |
| Middle level (community health centers) | Enable policymakers to understand more the patients' health service needs Solve the shortage of chronic disease managers in community health centers |
Establish a communication platform between patients and policy makers for chronic diseases Give full play to the role of community volunteers and provide patients with follow-up services that do not require special expertise |
| Solve the problem of low-quality care assessment for chronically ill patients | Improve the professional capabilities of chronic disease prevention and control managers in the community (Particularly, the care of severe mental diseases requires full-time personnel.) | |
| Macro level (policies) | Address patients' needs for safer and more effective new medical solutions | Formulate policies to encourage drug research and development in the chronic disease field |
| Accelerate the building of medical consortia and promote personnel linkage | A “hand-in-hand” training model for the experts in tertiary hospitals to train the staff of community health centers | |
| Form a prevention-focused policy orientation | Reasonably arrange fiscal funds for chronic disease prevention and control and increase the proportion of funds for chronic disease prevention | |
| Establish a “dedicated and integrated” team for COPD | Include chronic diseases of the respiratory system such as COPD into the national basic public health project |
Chronic care delivery system
According to Strengthening Health Systems to Improve Health Outcomes issued by the WHO in 2007, the six elements of a health system consist of an organizational framework, health human resources, health information system, health financing, drugs and materials, and incentives.51 In this study, we propose a design for China's chronic care delivery system during the next development stage according to these six elements of a health system (Fig. 2).
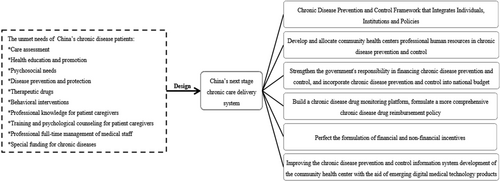
Design proposal for the next stage of China's chronic care delivery system.
Develop and allocate professional human resources in community health centers toward chronic disease prevention and control
With adequate available resources, a good health workforce should act in a responsible, fair, and efficient manner to achieve the best possible health outcomes.51 However, training personnel in chronic disease prevention and control should be intensified to improve the capabilities of professional community-based chronic disease prevention and control in terms of education. For example, the curricula of medical institutions or health care educational institutes should be updated to more completely address the needs of patients with chronic diseases. Decision-makers of the Ministry of Education play an important role in improving prevention and control of chronic diseases that cannot be ignored in planning chronic disease prevention and control systems. On the other hand, through personnel linkage with medical consortia, tertiary hospital experts provide training to primary community health centers staffs. This kind of training may take the form of expert consultation or systematic training workshops to improve chronic disease management expertise among general physicians and to comprehensively improve their management capabilities.
Strengthen government responsibility in financing chronic disease prevention and control and incorporate funds into the national budget
The raising of funds for prevention and control of chronic diseases is key to solving the unmet needs of patients with these diseases. From the perspective of the nature of chronic diseases, funds may be raised by government, society, and individuals.52 China has many problems in financing chronic disease prevention and control, including government investment that is seriously lacking, which places a heavy financial burden on patients, and the medical insurance system is incomplete among others.53 Thus, in the next development stage, China should strengthen government responsibility and include funds for chronic disease prevention and control in the national budget to ensure long-term sustainable investment in chronic disease prevention and control. China should also pay greater attention to the allocation of funds for the prevention and control of chronic diseases and provide more investment in chronic diseases prevention to reduce the incidence of chronic diseases and improve efficient utilization of funds.
Build chronic disease drug monitoring platform and formulate more comprehensive reimbursement policy
Within the context of high drug prices, patients with chronic diseases are faced with a high burden of disease, especially with respect to drug costs.54 Research by Tang et al55 showed that among patients with chronic diseases, the comprehensive drug welfare level among patients with COPD was evaluated and rated as average, and drug accessibility and equity were rated as low. That is, because drugs commonly used for respiratory diseases are lacking on the market, the needs of patients regarding these drug purchases cannot be met. Respiratory disease medications are not included in the permanent prescription list for inpatient with chronic diseases.56 Aimed at the problem of drug accessibility, it is necessary to build a chronic disease drug monitoring platform to understand, in real time, the research and development, production, distribution, and management of chronic disease drugs to prevent shortages of these drugs. In addition, it is essential to perfect the medical insurance reimbursement system for chronic disease drugs, include expansion of the catalog for drug reimbursement, increase the proportion of drugs for which reimbursement is available, improve availability of drugs for patients with chronic diseases, and reduce the financial burden on patients.
Perfect the formulation of financial and nonfinancial incentives
Incentives are the means for managers to reasonably improve labor efficiency. Incentives for patients, patients’ caregivers, and community health center medical staff are needed in the process of chronic disease management, which involves a long cycle. Nonfinancial incentives should be adopted for patients with chronic diseases and their caregivers, including the following: identifying daily health management tasks for patients, giving timely feedback regarding health status,57 and timely communication with patients by community-based chronic disease management personnel among others.58 These nonfinancial incentives can motivate patients to insist on prevention and treatment of chronic diseases. In addition, financial incentives should be adopted for chronic disease management personnel in the community, with nonfinancial incentives as supportive measures. Financial incentives include improving salary levels, increasing training opportunities, providing specific career development paths, and stimulating the motivation for work (e.g., fostering a sense of achievement by establishing honorary awards).59 Attractive incentives can facilitate long-term sustainability of chronic disease prevention and control efforts.
Improve chronic disease prevention and control information systems in community health centers using emerging digital medical technology
The new chronic disease management model requires not only specialized medical staff but also various types of medical application software for chronic disease management.60,61 With the aid of emerging digital medical technology products, patients with chronic diseases can receive standardized disease management guidance and personalized medical service at home to improve self-management, treatment compliance, and life quality. Thus, in the next stage of chronic disease prevention and control, such useful resources should be integrated to improve chronic disease management information systems using current big data and considering as the central needs of patients with chronic diseases.
Conclusions
Unmet need is used as an indicator that is broadly applicable to health system capability assessment. This study provides a basis for the future direction of China's chronic disease prevention and control system in the next stage of development, regarding the unmet needs of patients with chronic diseases as an indicator in combination with micro, middle, and macro level structure theory and six-element health system. In the design of China's chronic disease prevention and control system for the next decade, the unmet needs of patients with chronic diseases such as hypertension, diabetes, COPD, and severe mental diseases require special attention to reduce burden of disease from both patient and population levels. In measuring unmet needs of patients with chronic diseases, a communication platform for community health centers should be established to provide relevant chronic disease services in an accurate manner in real time. In the organization framework, the middle level connecting the micro and macro levels is the weakest, as there are insufficient full-time professional personnel for chronic disease management in primary community health centers. The organizational framework is the most important element of a complex health system, as chronic disease prevention and control is a lengthy process requiring concerted efforts of individuals, institutions, and policies to achieve sustainable and coordinated development of a system of chronic disease prevention and control.
Funding
This study was supported by the grants from National Natural Science Foundation of China (No. 71603278), Key Program of the National Natural Science Foundation of China (No.71734003), Youth Project of Educational Reform of China Pharmaceutical University (No. 2017XJQN32), and a research project on postgraduate educational reform under “double first-class” capability construction from China Pharmaceutical University (No. 3151920118).
Declaration of competing interest
None.