[123I]-phenylpentadecanoic acid uptake in patients with dilated cardiomyopathy
Abstract
Background
The rate constant for global fatty acid influx (k1) was studied in 12 male patients with dilated cardiomyopathy (DCM). Method: 10 normal subjects served as controls. 201-Thallium (201TI) and [123I]-phenyl-pentadecanoic acid (IPPA) were administered during bicycle exercise under fasting conditions.
Results
All patients showed non-homogeneous tracer uptake defects for 201TI and IPPA. k1 was significantly higher in DCM patients than controls. k1 showed significant inverse correlation between cardiac index, left-ventricular ejection fraction, left-ventricular enddiastolic pressure and echocardiographic left-ventricular ejection fraction.
Conclusion
We presume that an increased regional rate constant of IPPA influx into the myocardial tissue in patients with DCM reflects a compensatory mechanism of altered myocardium.
1. Introduction
Fatty acids are the major energy source of the myocardium 1,2. Several studies with different 123I-labeled fatty acids have been performed to investigate myocardial metabolism in patients with hypertrophic 3–10 dilated cardiomyopathy 11–15 and in patients with ischemic heart disease 16–18. We previously described a method for calculation of the rate constant of IPPA influx (k1) for a quantitative analysis of normal and altered fatty acid metabolism 19. In addition, there is evidence of a carrier-mediated transport of fatty acid into the myocardium and liver 20,21. The aim of our study was to investigate qualitative and quantitative parameters of myocardial fatty acid metabolism in patients with dilated cardiomyopathy (DCM), using the aforementioned mathematical theorem. We compared our results with the clinical and hemodynamic findings.
2. Methods
2.1. Subject population
12 male patients (mean age 48.2±8.9) with DCM were studied. Two patients were in NYHA class I, 4 in class II, 3 in class III and 3 patients in class IV. All patients underwent selective coronary and left-ventricular biplane cineangiography. Coronary angiogram and ventricular cineangiography were reviewed by at least two experienced angiographers. Hemodynamic data were obtained during catheterization. Calculation of left-ventricular ejection fraction was carried out using the Simpson's rule. Cardiac output was determined by the Fick principle. Transthoracic echocardiography was carried out in the left lateral position with parasternal and transverse bidimensional and M-mode view. Calculation of echocardiographic ejection fraction was performed using the Teichholz formula.
The etiology of DCM was a condition after myocarditis in 5 patients. The etiology in the remaining patients was unknown as no certain anamnestic data from these patients were available. Patients with a history of hypertension and coronary artery disease or angiographic signs of coronary sclerosis were excluded. All patients were on medication with ACE inhibitors, 8 (66.6%) with diuretics, 7 (58.3%) with digitalis and 4 (33.3%) with betablockers.
The study was conducted according to a study protocol approved by the Committee on Ethics of Human Investigators of the Heart Center Northrhine-Westphalia, Bad Oeynhausen, FRG. Base line data of all patients with DCM are listed in Table 1.
| Age (years) | 48±9 |
| NYHA class | 2.6±1.1 |
| Cardiac index (l/min/m2) | 2.4±0.6 |
| PAP (mmHg) | 28±12 |
| LVEF (%) | 30±12 |
- a NYHA: New York Heart Association; PAP: mean pulmonary artery pressure; LVEF: Left ventricular ejection fraction by angiography.
2.2. Control group
The study was performed in 10 control subjects (3 female, 7 male, mean age 46.4±7.1) without history of hypertension or angiographic evidence of coronary artery disease. Maximal workload during bicycle ergometry was 130±53.7 W.
2.3. Determination of myocardial fatty acid extraction

and IPPA:

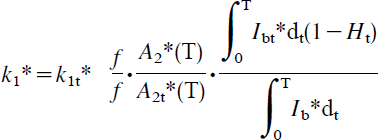
registered in a region of interest selected over a blood region in IPPA and 201TI integral images obtained in the first 10 min after indicator application. In this formula, f represents the regional myocardial blood flow and, as evident in this formula, the flow component can be eliminated. Ht indicates the hematocrit level.
During indicator application, a dynamic dual-isotope study at a left anterior oblique angle (LAO) of 30° was started. Total collection period was 10 min. For detection of emission we used a single-crystal camera (DATAMO, Picker, Cleveland). Dual-channel analyzer windows were centered at 75 (201TI) and 160 keV (123I) for dual-isotope counting. Subsequently, static images (anterior, LAO 45°, 75°) were collected in a supine position in front of the single-crystal camera (Dyna 4/15, Picker). The collection period was 6 min for each image. All scintigrams were corrected for crossover effects and for background activity using a modified algorithm described by Goris 22.
The semiquantitative circumferential analysis was performed by two experienced investigators. The degree of the tracer uptake defect with 201TI and IPPA was classified as none, mild or severe. Severe tracer uptake defects were then semiqualitatively classified as a defect involving less or more than 50% of the zone of interest in the corresponding imaging plane. Corresponding defects occurring both in 201TI and in IPPA were declared as matching defects for each imaging plane. A mismatch was presumed in non-corresponding defects of tracer uptake.
3. Statistical analysis
Base line data are given as mean value±standard deviation. We used a standard regression and correlation model for statistical evidence between fatty acid influx and hemodynamic data. The Students t-Test was performed to calculate the statistical significance between the rate constant of fatty influx (k1), hemodynamic and clinical data. An error probability of P<0.05 was considered statistically significant.
4. Results
The base line data of the investigated patients and the corresponding hemodynamic values and nuclear imaging data are listed in Table 2.
| No, pat. | Age | k1 | NYHA | Work | CI | LVEF | LVEDP | Nuclear | Nuclear defect |
|---|---|---|---|---|---|---|---|---|---|
| (years) | (min−1) | load (W) | (l/min/m2) | (%) | (mmHg) | defect | characterization | ||
| 1, V | 56 | 0.320 | 2 | 75 | 3.2 | 49 | 10 | Moderate | FA<50% |
| 2, S | 40 | 0.605 | 4 | 50 | 1.4 | 17 | 36 | Severe | FA>50% |
| 3, F | 45 | 0.475 | 4 | 75 | 1.9 | 24 | 17 | Moderate | TH-FA<50% |
| 4, G | 59 | 0.462 | 2 | 100 | 2.2 | 33 | 15 | Moderate | TH-FA<50% |
| 5, R | 33 | 0.572 | 4 | 25 | 2.2 | 31 | 28 | Severe | TH-FA>50% |
| 6, M | 50 | 0.515 | 2 | 100 | 2.5 | 19 | 20 | Severe | TH-FA>50% |
| 7, R | 62 | 0.380 | 1 | 125 | 3.3 | 38 | 20 | Severe | FA>50% |
| 8, S | 42 | 0.480 | 3 | 100 | 1.9 | 43 | 24 | Severe | TH>50% |
| 9, L | 57 | 0.460 | 1 | 100 | 2.7 | 41 | 10 | Moderate | TH-FA<50% |
| 10, S | 50 | 0.510 | 3 | 125 | 2.9 | 29 | 15 | Severe | FA>50% |
| 11, K | 40 | 0.550 | 3 | 125 | 1.6 | 9 | 35 | Moderate | TH<50% |
| 12, N | 44 | 0.430 | 2 | 75 | 3.0 | 24 | 31 | Moderate | TH-FA<50% |
- a k1: rate constant of fatty acid influx; NYHA: New York Heart Association; CI: cardiac index; LVEF: left-ventricular ejection fraction by angiography; LVEDP: left-ventricular enddiastolic pressure; TH: thallium, FA: fatty acid defect>(over)-(equal to) < (under) 50% circumferential extension.
4.1. Nuclear imaging
All patients showed non-homogeneous tracer uptake of 201TI and IPPA. In 6 of 12 patients (50%) the nuclear imaging defect was severe as indicated by a circumferential extension of more than 50%. The remaining patients had a moderate nuclear imaging defect. A mismatch in tracer uptake was observed in 6 patients, and matched regional uptake defects in the remaining patients. In 4 of 6 patients classified as demonstrating a mismatch, the defect was considered severe. Fatty acid uptake was predominantly compromised in 4 (3 severe defects, 1 with moderate defect) and thallium uptake in the other 2 patients (1 with severe defect, 1 with moderate defect) with a mismatch. Of the 6 patients with matched defects, the defect was severe in 2 of them, with a circumferential extension of >50%.
Regional distribution of tracer uptake defects was found as follows: 4 apex, 2 apex-lateral, 1 apex-septum, 1 apex-anterior, 1 septum-anterolateral, 1 septum-apex-inferior, and in the remaining patients diffuse defects.
No statistically significant differences could be shown between the severity of the nuclear defect (severe vs. moderate), the kind of nuclear defect (predominantly fatty acid defect vs. remaining defects) and hemodynamic, echocardiographic data, global fatty acid extraction and the k1 value.
Determination of the rate constant of the global fatty acid influx (k1) revealed significantly higher values in patients with DCM than in the control group (0.48±0.08 vs. 0.39±0.05, P<0.01). In the patients with DCM there was also a marked difference in k1 between those classified NYHA I/II and those NYHA III/IV (0.43±0.07 vs. 0.53±0.05, P<0.05).
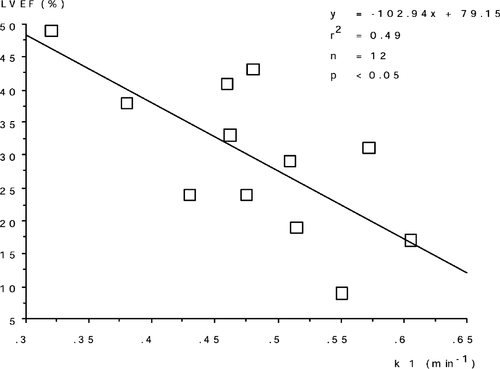
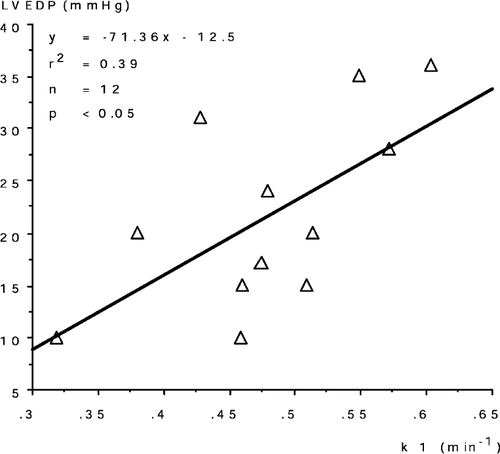
We could demonstrate a significant inverse correlation between k1 and cardiac index (r2-0.59, P<0.005, Fig. 1), angiographic left-ventricular ejection fraction (r2-0.49, P<0.05, Fig. 2) and echocardiographic left-ventricular ejection fraction (r2-0.49, P<0.05). There was a positive correlation between k1 and left-ventricular enddiastolic pressure (r2-0.40, P<0.05, Fig. 3). No correlation was found between k1 and left-ventricular enddiastolic volume, pulmonary artery pressure and left-ventricular mass determined by echocardiography.

5. Discussion
Our study investigated altered fatty acid metabolism in patients with dilated cardiomyopathy using 201TI as a perfusion tracer and [123I]-phenyl-pentadecanoic acid as a metabolic tracer. Furthermore, a mathematical theorem was adopted to calculate the rate constant k1 or the global fatty acid influx 16.
5.1. Thallium scintigraphy
In accordance with other studies with both the SPECT technique 23 and planar scintigraphy mn 24–27 we found a non-homogeneous distribution of 201-Thallium defects. The cause of such an inhomogeneity remains unclear. One explanation may derive from the fact that, in patients with dilated cardiomyopathy, increased myocardial fibrosis is often found and represents the end stage of the disease 28. In contrast to the hypothesis of increased fibrosis in the study carried out by Dunn et al., at autopsy they found no increased fibrosis in the respective areas of a complete Thallium defect. An explanation of these findings was given by Hoffmeister 23 in which the non-homogeneously reduced left ventricular function in dilated cardiomyopathy 29 may cause the inhomogeneity of the thallium defects. This possibly leads to an increased left ventricular wall stress caused by myocardial wall motion abnormalities and heterogenous tracer uptake 30. Similar observations derived from an animal study in which changes in left ventricular geometry or contraction pattern cause a relative difference in the density of radioactivity per unit area of myocardium 31. Furthermore, the prognostic value of Thallium defects and their degree remains uncertain. Tamai et al. 32 and Takata et al. 33 could demonstrate a worse outcome in patients with large Thallium defects, whereas no significant correlation to patient outcome could be identified in other investigations 34,35.
5.2. IPPA scintigraphy
Similar to our findings with 201TI scintigraphy, all our patients showed a non-homogeneous pattern of the IPPA uptake. Heterogeneous spotty myocardial uptake as an indicator of disturbance in fatty acid utilization [17–123I] iodoheptadecanoic acid was similar to our findings demonstrated by Höck et al. 36 in patients with idiopathic congestive cardiomyopathy. Ugolini and colleagues 12 demonstrated in patients with DCM a more rapid percent washout rate of IPPA than control subjects and the degree of heterogeneity of IPPA uptake was significantly related to the patients’ New York Heart Association functional class. In contrast, Feinendegen et al. 14 could not demonstrate a difference in regional uptake in a dual tracer approach using 15-Ortho-[123I]-phenyl-pentadecanoic acid (oPPA) and 15-para-[123I]-phenyl-pentadecanoic acid (pPPA), the latter being the same tracer used in our study. An explanation regarding the lack of heterogenous uptake was attributed to the use of planar scintigraphy or the different kinetics of uptake of IPPA vs. I-hepadecanoic acid. Narita 13 and Torizuka 37 used beta-methyl-p-[123I]-iodophenyl-pentadecanoic acid (BMIPP) in contrast to the [123I]-iodophenyl-pentadecanoic acid (IPPA) in our study. Their results suggest that in patients with DCM, disturbance of myocardial fatty acid metabolism appeared before perfusion abnormality and/or myocardial necrosis developed. The quantification of BMIPP imaging may be useful for assessing the prognosis in patients with DCM. Nevertheless, it seems that various labeled fatty acids are superior in detecting altered metabolism in patients with DCM, as could be noted in our study population, where predominant IPPA defects (> 50% circumferential extension) occurred in the group of patients representing a mismatch.
5.3. Rate constant of global fatty acid influx
In normal human myocardium we could demonstrate a homogeneous distribution of fatty acid uptake and present the method for measuring IPPA influx 19. We presumed that, under pathological conditions, with the overlapping of normal and pathological tissue, homogeneous behavior of myocardium cannot be expected. In our study population we therefore used a regional calculation of IPPA influx and, instead of planar scintigraphy, a single photon tomography to minimize errors deriving from areas of low activity accumulation. The sum of each regionally calculated (k1) led to the global k1 value. For the first time the global rate of IPPA influx, representing the heterogeneity of fatty acid uptake, was calculated and demonstrated as an inverse correlation, with hemodynamic results and a clinical stage in this study population. Interpretation of our results remains speculative. IPPA is metabolized by β-oxidation in the mitochondria in a similar way in the myocardium as palmitic acid 38. An alteration in myocardial metabolism represented by different kinetic patterns in a dual tracer study (oPPA and pPPA) was presumed by Feinendegen et al. 14 in their study in patients with dilated cardiomyopathy. This led to a classification of three types of kinetic pattern representing the following subtypes or stages in DCM: (1) predominantly increased β-oxidation; (2) predominantly decreased β-oxidation with increased backdiffusion and (3) predominantly increased backdiffusion. Our findings with a non-homogeneous distribution of IPPA uptake in patients with DCM possibly reflects various areas of the myocardium representing various stages of damage and repair. Possibly those areas in a state of repair represented by a higher fatty acid uptake are zones with increased β-oxidation at the level of the mitochondria. This is supported by electron microscopy, where in patients with dilated and hypertrophic cardiomyopathy the number of mitochondriae are elevated 39,40. Contradictorally, Thies et al. 41, using the same theoretical and mathematical theorem in eight young patients with DCM (age 0.2–18 years), were unable to demonstrate a significant higher fatty acid uptake, possibly due to the fact that the investigation was carried out in a predominantly pediatric population. Another explanation is given by Ugolini et al 12. They hypothesize that heterogeneity and the more rapid myocardial clearance of IPPA assessed by SPECT imaging could be related to increased levels of circulating catecholamines that favor more rapid fatty acid metabolism.
Another explanation for non-homogenous distribution of IPPA uptake may derive from the fact that different stages of myocardial injury can be detected by monoclonal antimyosin uptake. Obrador et al. 42 could identify patients with chronic dilated cardiomyopathy with myocyte damage detected by monoclonal antimyosin uptake with negative endomyocardial biopsies. Yamada et al. 43 described various forms of antimyosin uptake in patients with dilated cardiomyopathy. Localized, intense and diffuse antimyosin uptake with no perfusion abnormalities (active myocarditis) and no antimyosin uptake without perfusion abnormalities (healed myocarditis). Patients with dilated cardiomyopathy and without positive endomyocardial biopsy showed diffuse or localized antimyosin uptake and inhomogenous or localized perfusion defects. IPPA uptake with a non-homogenous distribution possibly reflects various areas with different stages of myocardial injury.
One could suggest that our results may be influenced by different coronary flow patterns within the various myocardial regions, as shown by Reske et al. 44. Such a regional coronary flow dependent accumulation and elimination of IPPA was considered in our mathematical theorem, as demonstrated above. Using the mathematical formula, the flow component was eliminated.
We therefore hypothesize that, in patients with DCM, a globally higher uptake of IPPA calculated by the rate constant k1 represents the compensatory reaction of the damaged myocardium. This does not exclude that different stages of myocardial damage are reflected by IPPA imaging planes in the same patient, where areas with predominant fibrosis are found beneath areas with higher metabolic activity. Our results, obtained in a relatively small number of patients, could be of importance in identifying those patients with DCM with the additional potential for a repair process, indicated by a higher fatty acid uptake. As demonstrated by different patterns in antimyosin uptake, thallium perfusion abnormalities and non-homogenous IPPA uptake, dilated cardiomyopathy demonstrates a clinical condition with heterogenous findings from cardiac imaging techniques that should be clarified by endomyocardial biopsy studies.
6. Study limitations
In this study, neither invasive nor nuclear medical investigation was performed at a given control period since such investigation was not permitted by the Ethics Committee. In this population study, we did not carry out any electron microscopy or histological examination of myocardial tissue. This would be of importance regarding those patients with histological findings corresponding to acute myocarditis with respect to the metabolic state investigated by IPPA uptake. Furthermore, the determination of catecholamine plasma levels was not carried out, so that the hypothesis that higher plasma levels lead to an enhanced uptake of fatty acids could not be confirmed. Nevertheless, the amount of circulating catecholamines is not representative of the effect they have on the ultrastructural level regarding mitrochondrial energy processes and lipid turnover.
7 Acknowledgements
The authors wish to thank Mrs Sarah L. Kirkby for her assistance in preparing this manuscript.




