Carbon dioxide-enhanced virtual MDCT cholangiopancreatography
Abstract
Background/Purpose
We investigated the feasibility of new carbon dioxide-enhanced virtual multidetector computed tomography (MDCT) cholangiopancreatography (CMCP) for intraluminal exploration in 73 patients with hepatobiliary and pancreatic disease.
Methods
CMCP was performed via a percutaneous or transpapillary drainage tube, and, synchronously, intravenous contrast material was employed for virtual angiography; three-dimensional (3D) virtual reality was incorporated using OsiriX and Fovia applications. The capability of carbon dioxide to delineate the biliary and pancreatic system was evaluated.
Results
All CMCPs showed complete technical success; complications including pancreatitis or pain never occurred. The incidences of visible third- and fourth-order biliary branches were 100 and 86.0%. The capability of carbon dioxide to pass an obstruction through an occluded hilar bile duct malignancy was 80.0%; it provided feasible information on additional bile duct segments. The full extent of the gallbladder was depicted in 72.7% of the studies. Minimum 2-mm lesions of biliary stones or gallbladder polyps were clearly detected. The main or second-order pancreatic ducts were visible in 100 and 83.3% of the studies, respectively. Carbon dioxide enabled the replacement of mucin and pancreatic juice and facilitated the detection of cystic lesions of intraductal papillary-mucinous neoplasm (IPMN) in 75.0% of the studies. We succeeded in achieving 3D spatial recognition of vascular structures in the cholangiopancreatic region, through the fusion of CMCP and 3DCT arteriography and venography in a single image scanning, and radiation time was decreased. This combined modality proved to be feasible for planning operations and for image-guided navigated surgery in the resection of a malignancy.
Conclusions
To our knowledge, this is the first report to demonstrate the diagnostic accuracy of carbon dioxide MDCT cholangiopancreatography and the use of this modality for depicting biliary, pancreatic, and fusion blood vessels simultaneously. Carbon dioxide possesses many advantages over conventional iodinated contrast agents, and it might replace more invasive diagnostic measures in the near future.
Introduction
Recently, the imaging of biliary and pancreatic ducts has advanced dramatically, allowing accurate diagnosis and the selection of appropriate surgical procedures. Although several less invasive techniques now exist for cholangiopancreatography, including drip infusion cholangiography (DIC), computed tomography (CT), DIC-CT, magnetic resonance imaging (MRI), MR-cholangiopancreatography (MRCP), three-dimensional (3D) CT, and color-flow and duplex sonography, the gold standard against which these techniques are compared remains direct catheter cholangiography or endoscopic retrograde cholangiopancreatography (ERCP). However, despite the development of lowosmolar contrast agents, premedication regimens, and careful patient selection, adverse reactions to contrast material, including idiosyncratic reactions and contrast-induced nephropathy, continue to occur in a small number of patients.
Carbon dioxide (CO2) as a contrast agent in cholangiography has been developed as an alternative to iodinated contrast material to avoid these problems 1-4. Once the behavior of intraluminal CO2 gas, the methods of safe delivery, and the principles of successful imaging are understood, the use of CO2 as a contrast agent during cholangiopancreatography will allow accurate imaging with little risk.
CT and MRI have greatly altered the paradigm of diagnostic imaging, with recent progress in imaging techniques and workstation-assisted image reconstruction providing benefits for pancreato-biliary diseases. Multidetector CT (MDCT) has recently brought new techniques for the rendering of volumetric data that have to be clinically tested: a new perspective on conventional MDCT imaging is given by the computer-simulated intraluminal viewing of human body cavities. Virtual reality systems have been proposed for virtual cholangiography and pancreatography, as well as for the 3D reconstruction of liver, bile duct, and pancreas, with surrounding organ anatomy, and hollow viscera allowing virtual endoscopic 3D reconstruction that has also been applied to various other regions of the human body. Utilizing recent dramatic advances in MDCT imaging techniques and workstation-assisted image reconstruction, 3D virtual cholangiopancreatic reconstruction with CO2 gas as a negative contrast agent may be demonstrated to be useful in clinical practice. The impact of these systems in preoperative diagnostics has not been established, due to the lack of large clinical series evaluating their reliability. We investigated the feasibility of CO2 MDCT cholangiopancreatography (CMCP) for intraluminal exploration in patients with hepatobiliary and pancreatic disease.
Subjects
From September 2004 to May 2008, we selected a total of 73 patients (48 men and 25 women; age, 33–93 years; mean age ± SD, 67.5 ± 13.7 years) presenting to the Department of Surgery, Teikyo University Chiba Medical center (Chiba, Japan) with suspected hepatobiliary and pancreatic disease (Table 1), who had clinically required external drainage of the bile or pancreatic duct.
| Total patient number | 73 |
| Men | 48 |
| Women | 25 |
| Age (years) | 33–93 |
| Mean | 67.5 |
| Standard deviation | 13.7 |
| Disease | Patients |
| Biliary disease | 61 |
| Biliary malignancy | 21 |
| Cholecystitis | 25 |
| Benign biliary obstruction | 4 |
| Biliary stone | 4 |
| Gallstone | 3 |
| Gallbladder polyp | 2 |
| Hepatic peribiliary cyst | 1 |
| Cholangiocellular carcinoma | 1 |
| Pancreatic disease | 12 |
| Pancreatic malignancy | 3 |
| Intraductal papillary mucinous adenoma (IPMA) | 8 |
| Serous cyst adenoma | 1 |
- Includes duplication
- Teikyo University Chiba Medical Center, September 2004 to May 2008
Informed consent was obtained from all the patients after procedures had been explained to them. The institutional review board approved this study. Patients with advanced age, respiratory disorder, liver failure, renal failure, or a history of allergic reaction to iodinated contrast agent were excluded from the study.
Methods
MDCT examinations were performed using a 16-MDCT scanner (LightSpeed Ultra 16; GE Healthcare, Milwaukee, WI, USA). Imaging parameters were collimation, 16 × 0.625 mm; 0.8-s rotation; 120 kVp; and 350 mAs, and mean scanning time was approximately 25 s.
Pure CO2 was sucked into a sterile syringe through a sterile gas filter from a CO2 gas Dispenser (Gaster, Cathex, Tokyo, Japan) (Fig. 1). First, 3–5 ml of pure CO2 was injected in approximately 5 s by hand via a percutaneous or transnasal biliary/pancreatic catheter, which had been placed 2 days before the procedure. After an uneventful test examination, biliary and pancreatic distention was achieved with approximately 20–60 ml for cholangiography and 10–20 ml for pancreatography at approximately 1 ml per s (less than 5 mmH2O of intraluminal pressure) by manual insufflations. Synchronously, intravenous iodinated contrast material was applied for virtual angiography. Images were obtained with the patient in the supine position and, when needed to optimally distend the right or left bile duct and pancreatic duct, in the right or left lateral decubitus position. All examinations were closely monitored by one of two body-imaging radiologists who assessed CO2 distention and determined the need for imaging in addition to imaging with the patient supine and prone. Two-dimensional images in the axial, coronal, and sagittal planes and volume-rendered 3D reconstructions were incorporated. Data were analyzed and processed using the commercially available software Advantage Workstation and Navigator medical image processing system (GE Healthcare) provided with the MDCT system.

The data were also incorporated into a virtual reality software system developed on a Macintosh platform with the MacOS X operating system with a MacPro (Apple, Cupertino, CA, USA) and an open-source DICOM viewer OsiriX 3.5 (OsiriX Foundation, Geneva, Switzerland) [5-7] and Fovia plug-in (Fovia., Palo Alto, CA, USA).
The aim of this study was to evaluate the accuracy of biliary and pancreatic anatomy depiction and the quality of biliary and pancreatic tract visualization of CMCP. The capability of CO2 to delineate distal parts of the biliary and pancreatic ducts was evaluated. All patients underwent conventional MRCP, ERCP, or DIC-CT. Two surgeons or radiologists who were blind to the results of the conventional imaging evaluated the image data. The feasibility of CMCP for use in operative navigation for surgical procedures was also evaluated.
Results
Technical feasibility
All consecutive CMCPs showed complete technical success; with a 0% morbidity rate. All CMCPs were performed without the occurrence of cholangitis, pancreatitis, increasing of hepatic or pancreatic enzymes, hepatic dysfunction, or organ injuries. The patients had no pain after the examination. The time required for reconstructing the images into virtual reality was within 5 min.
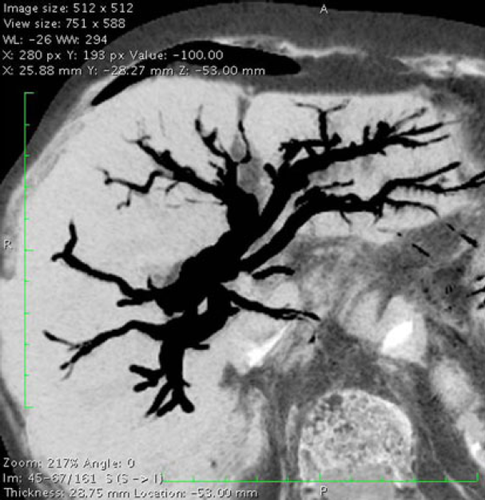
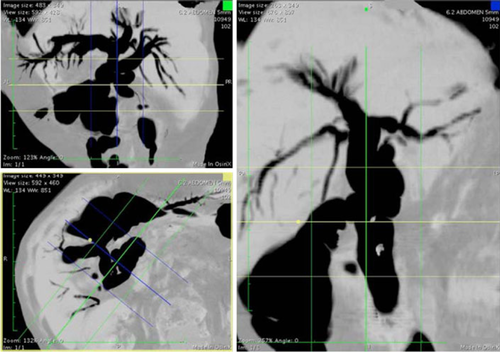
CO2 virtual cholangiography
The capability of CO2 to delineate distal parts of the biliary or pancreatic ducts is summarized in Table 2. CMCP revealed excellent visualization of the biliary and pancreatic duct system by replacing the intraductal fluid with carbon dioxide (Figs. 2, 3). There was good observer agreement in the depiction of biliary and pancreatic anatomy in all CMCP image sets (Tables 2, 3).
| Insufflation route of CO2 | Excellent depiction | Incidence |
|---|---|---|
| Common bile duct (n = 50) | Third-order biliary branches | 100.0% (50/50) |
| Fourth-order biliary branches | 86.0% (43/50) | |
| Occluded distal segment in hilar carcinoma | 80.0% (4/5) | |
| Gallbladder (n = 11) | Extension of the gallbladder mucosa | 72.7% (8/11) |
- Teikyo University Chiba Medical Center, September 2004 to May 2008
| Insufflation route of CO2 | Excellent depiction | Incidence |
|---|---|---|
| Pancreatic duct (n = 12) | Main pancreatic duct | 100.0% (12/12) |
| Second-order pancreatic branches | 83.3% (10/12) | |
| Cystic lesions of IPMN communicating with the main pancreatic duct | 75.0% (6/8) |
- Teikyo University Chiba Medical Center, September 2004 to May 2008
- IPMN intraductal papillary-mucinous neoplasm
The incidence of visible third- or fourth-order biliary branches was 100% (50/50) and 86.0% (43/50) on CO2 cholangiography (Fig. 4). The capability of CO2 to pass an obstruction through an occluded hilar bile duct malignancy via percutaneous transhepatic cholangiodrainage (PTCD) was 80.0% (4/5); it provided feasible information on additional bile duct segments (Fig. 5).
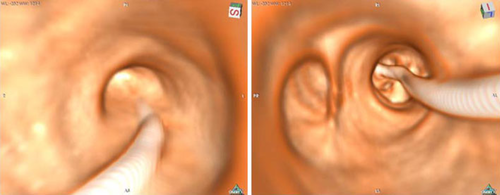
Virtual endoscopy of the bile duct was clearly reproduced. It revealed the full extent of ductal involvement and branches due to fulfilling CO2 (Fig. 6). The full extent of the gallbladder mucosa was depicted in 72.7% of the studies (8/11) using gallbladder insufflations through percutaneous transhepatic gallbladder drainage/endoscopic naso-gallbladder drainage (PTGBD/ENGBD). Minimum 2-mm diameter lesions of biliary stones and gallbladder polyps were clearly detected (Fig. 7).
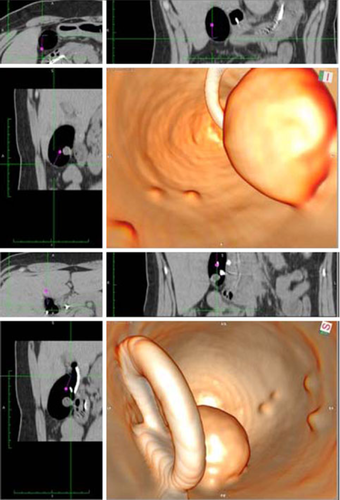
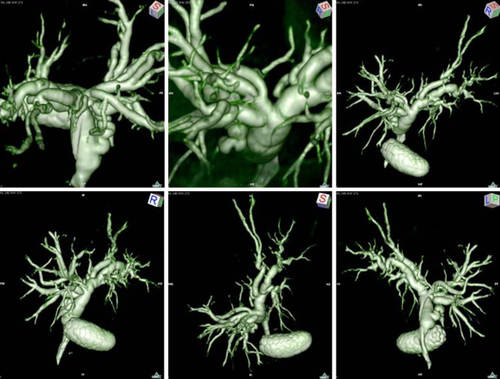
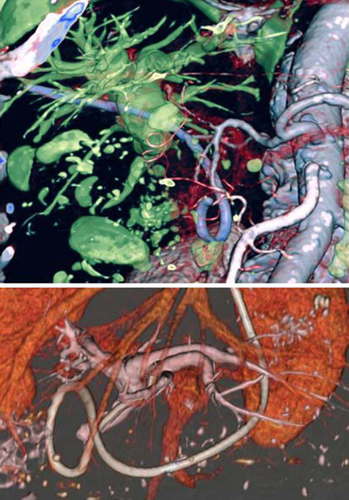
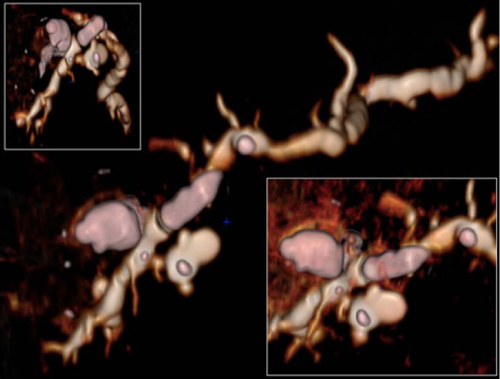
We succeeded in achieving 3D spatial recognition of vascular structures in the cholangiopancreatic region, through the fusion of CMCP and 3DCT arteriography and venography in a single image scanning (synchronous fusion), and radiation time was decreased (Fig. 8).
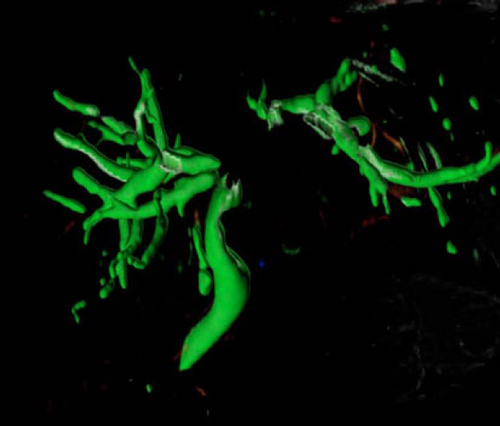
CO2 virtual pancreatography
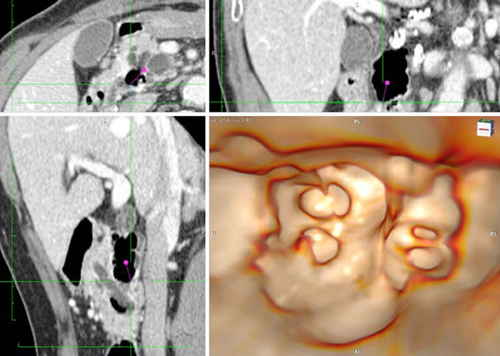
The incidence of a visible main pancreatic duct or second-order pancreatic banches was 100% (12/12) and 83.3% (10/12) on CO2 pancreatography (Table 3). CO2 enabled the replacement of mucin and pancreatic juice, and facilitated the detection of small cystic lesions of intraductal papillary-mucinous neoplasm (IPMN) communicating with the main pancreatic duct in 75.0% (6/8) of the studies. Side-branch IPMN lesions appeared as grape-like clusters associated with the pancreatic ductal system (Fig. 9).
A diffusely dilated main pancreatic duct containing mucinous filling defects was diagnostic of main-duct IPMN (Fig. 10). We succeeded in achieving 3D spatial recognition of vascular structures in the pancreatic region. Virtual CO2 pancreatoscopy using MDCT also revealed excellent endoluminal visualization of a diffusely dilated main pancreatic duct containing mucinous filling defects in main-duct IPMN (Fig. 11).

Discussion
Our study demonstrates the potential utility of CMCP in the preoperative assessment of the biliary and pancreatic systems. To our knowledge, our study is the first to demonstrate the diagnostic accuracy of CO2-enhanced cholangiopancreatography at MDCT for depicting biliary, pancreatic, and blood vessel anatomy simultaneously. Traditionally, invasive techniques, including PTCD and ERCP, have been considered indispensable for the evaluation of biliary tract cancer. Persistently repeated biliary drainage and cholangiography prolong preoperative and total hospitalization periods. During this period, cholangitis and the patient's nutritional state are often adversely affected, with a poorer prognosis due to the delay in the initiation of treatment and surgery, often resulting in a reduction in patients' quality of life.
The clinical application of CO2 has been established in laparoscopic surgery, with some reports of intravascular [8, 9] and intrabiliary [1, 2] administration in clinical practice. As a gaseous contrast agent, its physicochemical properties have special requirements concerning the radiologists' knowledge, the X-ray equipment, the infuser and the catheters. In a recent clinical trial, CO2 infusion was more effective than hydration in the prevention of contrast-induced nephropathy 10.
We prefer CO2 as a contrast medium because it is not nephrotoxic, does not cause vascular volume expansion, has low viscosity for better visualization of the portal vein without staining the hepatic parenchyma, and reduces the risks of hepatic injury and mortality 11. CO2 administered in the biliary or pancreatic duct is rapidly eliminated. MDCT exposure, causing no pain or complications, either during or following administration, has no adverse events associated with intrabiliary CO2 administration. At our institution, more than 100 consecutive performances of intrabiliary or intrapancreatic CO2 administration have been applied without the occurrence of any pain or complications, including bilio-pancreatic anatomical injuries, pancreatitis, cholangitis, or hepatic dysfunction 12. The results of the present study demonstrated the reliable capability of CO2 to delineate distal parts of the biliary duct (Table 2). Because of its low viscosity, CO2 was a useful contrast medium to visualize the extrahepatic biliary system before performing external–internal biliary drainage in conditions of biliary obstruction. Unnecessary percutaneous intraductal manipulations may be reduced 2. Our results were clinically feasible, in that the incidences of visible third- and fourth-order biliary branches were 100 and 86.0%, and the capability of CO2 to pass an obstruction through an occluded hilar bile duct malignancy was 80.0%. These results provided feasible information on additional bile duct segments and helped the surgeon to determine the surgical margins at bile duct resection (Fig. 5).
The 3D virtual cholangioscopy provides detailed preoperative reconstruction of the biliary anatomy. Using CO2 insufflations into the bile duct, it was easy to reveal the full extent of ductal involvement and branches, including the gallbladder, due to CO2 (Fig. 6). The incidence of depiction of the gallbladder mucosa was 72.7% using the gallbladder insufflations. Even the minimum 2-mm diameter lesions of biliary stones and gallbladder polyps were clearly detected (Fig. 7).
We succeeded in achieving 3D spatial recognition of vascular structures in the cholangiopancreatic region, through the fusion of CMCP and 3DCT arteriography and venography in a single image scanning (synchronous fusion) (Fig. 8). The volume rendering of the biliary tree provided valuable information for planning surgery, including the location of the obstruction and its relationship to the surrounding vessels. Our data emphasize that 3D and synchronous fusion imaging was an accurate and routinely applicable tool for the diagnosis and therapeutic management of patients with biliary diseases. Synchronous fusion enabled the reduction of unnecessary multiphase scanning, and it decreased both the examination time and radiation time.
CO2 virtual pancreatography
CT is an excellent test for cystic lesions of the pancreas because of its widespread availability and ability to detect cysts 13. MR imaging is used increasingly because of its ability to determine whether there is involvement of the main pancreatic duct 14. Both these imaging modalities offer diagnostic strengths. CT is often the initial modality with which a cystic lesion is suspected or diagnosed. However, CT is relatively poor for the diagnosis of malignant transformation 15. MR imaging can reveal the full extent of ductal involvement, particularly when obstructing mucus prevents the diagnostic opacification of the entire duct, and this imaging is much less invasive than ERCP. The most specific signs of malignancy with CT are a solid mass, main pancreatic duct dilatation greater than 10 mm, diffuse or multifocal involvement, and attenuating or calcified intraluminal content 16. Despite these imaging features, the ability of CT and MR to accurately diagnose a specific cystic lesion and to determine whether malignancy is present remains uncertain. One of the most difficult problems in imaging intraductal papillary-mucinous neoplasm (IPMN) is the secretion of intraductal mucin. In the present study, CO2 enabled the replacement of the mucin and pancreatic juice and facilitated the detection of small cystic lesions of the IPMN communicating with the main pancreatic duct in 75.0% of the studies. When communication with the main pancreatic duct exists, virtual CO2 pancreatography and pancreatoscopy using MDCT would reveal side-branch IPMN lesions as grape-like clusters associated with the pancreatic ductal system, and main-duct IPMN would be depicted as diffusely dilated main pancreatic duct containing mucinous filling defects (Figs. 9-11).
Synchronous fusion cholangiopancreatography and angiography
Recently, the high-speed imaging capacity of MDCT has been utilized in virtual 3D construction of structures and vascularity on 3D-CT angiography (3DCTA). In clinical practice, a multiphase fusion approach is employed, involving construction and final fusion of 3DCTA. We succeeded in enhancing 3D spatial recognition of vascular structures in the cholangiopancreatic region, through the fusion of CMCP and 3DCTA (Fig. 10). In this fusion approach, the use of CO2 provides a negative contrast effect, with high contrast against intravascular medium, allowing simultaneous cholangiopancreatography and angiography in a single image scan (synchronous fusion). As multiphase fusion produces synthetic images in different temporal phases, there is a possibility that subtle respiratory or body fluctuations may cause “gaps” in image slices. In contrast, the CO2 MDCT technique produces complete synchronization, allowing 3D diagnosis based on more accurate spatial recognition. CMCP (CMCPA) therefore produces improvements, including shorter diagnostic imaging time, enhanced analysis, and an earlier start to treatment and surgery, contributing to improvement in patients' quality of life.
At present, there is no consensus on surgical indications and procedures for pancreato-biliary cancer, with substantial variation among institutions. Favorable long-term prognosis is unlikely without radical resection. For achieving accurate diagnosis of progress by dependable preoperative diagnostic imaging plus procedural simulations, CMCPA enabled the synchronous visualization of hepatobiliary pancreatic and abdominal vessels to provide accurate information for localizing hepatobiliary pancreatic malignancies and their relationship to the vessels. CMCPA was feasible for planning operations and for image-guided navigated surgery in the resection of tumors, dissection of lymph nodes, and preserving organ function.
The CMCPA approach is considered to be amenable to repetition compared to conventional techniques, due to its low invasiveness and convenience. However, it does require advanced catheterization of the biliary tract, warranting careful determination of the diagnostic significance and indications. If using 3D reconstructions could prevent even a small number of biliary tract injuries by preoperative identification of anatomic abnormalities, it may turn out to be actually cost-effective.
Virtual reality for surgical navigation by OsiriX
The introduction of the free DICOM viewer OsiriX [5-7] will allow surgeons to easily and directly perform 3D image analysis from the perspective of an operator. This removes the requirement for the expertise of radiologists or technicians and special equipment, a more effective approach for clinical practice. The availability and application of this approach for other organs and systems is likely to increase in the future, offering great potential for expansion of the scope of indications.
Virtual reality reconstructions have some limitations. Despite the improvements in data analysis performed by the software, the restrictions of MDCT remain even with 3D reconstruction. The most important disadvantage is that the reconstructions are still based on the original data of the MDCT. A natural advantage of using virtual reality is that the reconstruction is not just a better image but that it is also a real 3D virtual representation. This means that one is able to become engrossed in the image, navigate through the system, and cooperate with the image 17. In the near future, communication with the image will likely enable the performance of virtual biliary and pancreatic surgery on actual patient data.
In conclusion, CO2 possesses many advantages over conventional iodinated contrast agents used for cholangiopancreatography. Our results indicate that CMCP provided accurate visualization of hepatobiliary pancreatic disorders and detailed preoperative reconstruction of hepatobiliary pancreatic anatomy in safety. However, further technical maturation is required for further improvements in the diagnostic capability of CPMC at MDCT. Further studies are required to evaluate the safety of this method and to develop an improved delivery of CO2 gas for this application. Newer software developments may further enhance its accuracy, so that CMCP might challenge or replace more invasive diagnostic measures in the near future.
Acknowledgments
The authors thank Professor Toshiyuki Ohkubo MD and Mr. Yasuhiro Fujiwara, Department of Radiology, Teikyo University Chiba Medical Center; Professor Katsuhiro Uchiyama MD, Sannoh Hospital Medical Center; and Doctor Kazuhiro Sato MD, Advanced Research Institute Of Gastroenterological Imaging, for their valuable suggestions. This study was partially supported by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science, a JFE Grant from the Japanese Foundation for Research and Promotion of Endoscopy, and a Teikyo University Tomoko Fujii Memorial Research Grant for young medical researchers.