Intraoperative exploration of biliary anatomy using fluorescence imaging of indocyanine green in experimental and clinical cholecystectomies
Abstract
Background/purpose
We evaluated the usefulness of intraoperative exploration of the biliary anatomy using fluorescence imaging with indocyanine green (ICG) in experimental and clinical cholecystectomies.
Methods
The experimental study was done using two 40-kg pigs and the clinical study was done in 12 patients for whom cholecystectomy was planned from January 2009 to June 2009. Initially we used a laparoscopic approach for the evaluation of fluorescence imaging of the biliary system in the two pigs. Then the clinical study was started on the basis of these experimental results. ICG (1.0 ml/body of 2.5 mg/ml ICG) was infused 1–2 h before surgery. With the subjects under general anesthesia we observed in real time the condition of the biliary tract under the guidance of fluorescence imaging employing an infrared camera or a prototype laparoscope. ICG was added intravenously to observe the location or flow condition of the cystic artery.
Results
We obtained a clear view of the biliary tract and the location of the cystic duct in the two pigs. Local compression with a transparent hemispherical plastic device was effective for offering a clearer view. The biliary tract, except for the gallbladder, was clearly recognized in all clinical subjects. Local compression with a transparent hemispherical plastic device for open cholecystectomy and a flat plastic device for laparoscopy provided clearer visualization of the confluence between the cystic duct and common bile duct or common hepatic duct. The location of the cystic artery was revealed after division of the connective tissues, and the flow condition of the cystic artery was confirmed 7–10 s after intravenous re-infusion of ICG. There were no adverse events related to the intraoperative procedure or the ICG itself.
Conclusions
This method is safe and easy for the identification of the biliary anatomy, without requiring cannulation into the cystic duct, X-ray equipment, or the use of radioactive materials. Although fluorescence imaging is still at an early stage of application in comparison with ordinary intraoperative cholangiography, we expect that this method will become routine, offering a lower degree of invasiveness that will help avoid bile duct injury.
Introduction
The laparoscopic management of biliary diseases has become widely accepted and practiced. In particular, laparoscopic cholecystectomy has become a standard procedure for gallbladder disorders. However, even after the acquisition of laparoscopy skills, iatrogenic biliary injury still occurs during laparoscopic cholecystectomy, and can seriously compromise the outcome. Although intraoperative cholangiography (IOC) is a useful tool for the confirmation of biliary anatomy or injury, a small orifice needs to be created in the cystic duct in order to perform IOC. If, in doing so, the common bile duct is mistaken for the cystic duct, then biliary injury is inevitable. Therefore, a new form of intraoperative assessment is needed to prevent or reduce bile duct injuries. Here we introduce a new method for the intraoperative exploration of the biliary anatomy, using fluorescence imaging with indocyanine green (ICG; Diagnogreen; Daiichi Sankyo, Tokyo, Japan). ICG is widely available and has one of the lowest reported toxicities of any clinically employed dye [1, 2]. Recently, its characteristics have been exploited for the identification of sentinel lymph nodes in patients with breast [3, 4] or gastrointestinal 5 cancers, for confirming the patency of vascular reconstruction during liver transplantation 6, and for lymphography in patients with secondary lymphedema 7. There have been few previous reports on the use of fluorescence imaging of the biliary tract, in either experimental [8, 9] or clinical 10 studies. We evaluated our intraoperative exploration of the biliary anatomy using fluorescence imaging with intravenous ICG in experimental and clinical cholecystectomies. This is the first report of laparoscopic observation employing fluorescence imaging guidance in humans.
Patients, materials, and methods
The experimental study was done using two 40-kg pigs and the clinical study was done in 12 patients for whom cholecystectomy was planned from January 2009 to June 2009. Initially we used a laparoscopic approach for the evaluation of fluorescence imaging of the biliary system in the two pigs. Then the clinical study was started on the basis of these experimental results. Clinically, laparoscopy was performed in 8 of the patients, and an open approach was used in the other 4 patients (who had acute or chronic cholecystitis). ICG (1.0 ml/body of 2.5 mg/ml ICG) was infused 1–2 h before surgery.
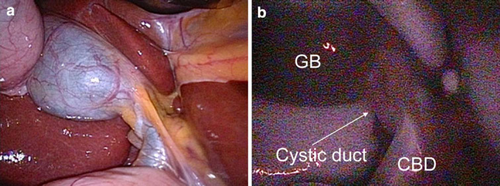
Laparoscopic approach in the experimental study
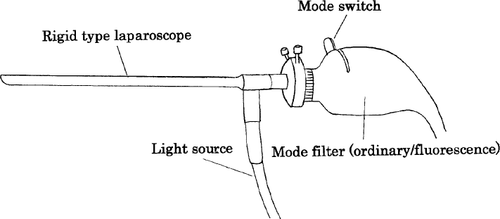
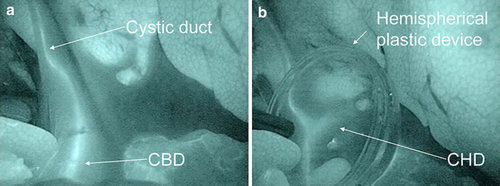
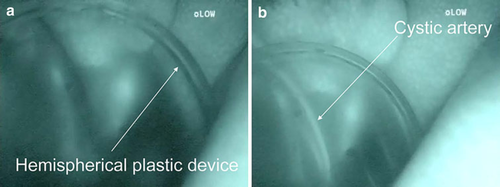
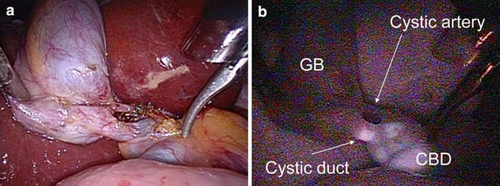
With the animal under general anesthesia we created four ports (12-mm ports at the center of the midline, and three 5mm ports in the subxiphoid and the right subcostal regions) into the peritoneal cavity after obtaining pneumoperitoneum by CO2 insufflation. We observed the area from the hepatic hilum to the duodenum under the guidance of fluorescence imaging with a prototype infrared camera connected to a laparoscope (Fig. 1) (Harada et al. 11 reported the usefulness of an ICG fluorescence endoscope for observing the placental vascular network) at the point of initial insertion of the laparoscope, during the division of the connective tissues, and after the identification and dissection of the cystic duct and artery, respectively. An originally manufactured transparent hemispherical plastic device was used to obtain local compression with clearer fluorescence imaging over the biliary tract (Fig. 2a, b). To observe the flow in the cystic artery, ICG (2.5 mg/ml) was re-administered intravenously through the venous line after identifying the vessel structure (Fig. 3a, b).
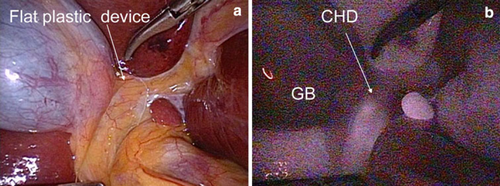
Laparoscopic approach in clinical study
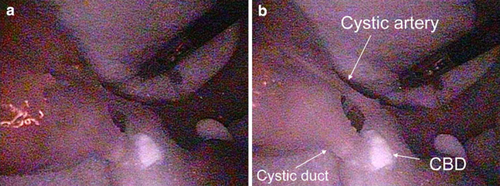
With the patient under general anesthesia we created four ports (12-mm ports at the umbilicus and subxiphoid, respectively, and two 5-mm ports in the right subcostal region) into the peritoneal cavity after obtaining pneumoperitoneum by CO2 insufflation. We observed the same area as that observed in the experimental study using a prototype infrared camera connected to a laparoscope at the point of initial insertion of the laparoscope (Fig. 4a, b), during the division, and after identification and the dissection of the cystic duct and artery (Fig. 5a, b), respectively. An originally manufactured transparent hemispherical or flat (Fig. 6) plastic device was used to obtain local compression with clearer fluorescence imaging over the biliary tract (Fig. 7a, b). To observe the flow in the cystic artery, ICG (2.5 mg/ml) was re-administered intravenously through the venous line after identifying the vessel structure (Fig. 8a, b). Intraoperative cholangiography was also performed for comparison with fluorescence imaging of the biliary tract in the human patients.

Open approach in clinical study
With the patient under general anesthesia we also observed the condition of the biliary tract or cystic artery using an infrared camera system (PDE; photodynamic eye; Hamamatsu Photonics, Shizuoka, Japan) at the same point as that used for the laparoscopic approach. This system is equipped with a light-emitting diode that produces light with a wavelength of 760 nm, together with a chargedcoupled device camera with a filter. A transparent hemispherical plastic device was also used to facilitate clearer fluorescence imaging during the open approach.
Results
Laparoscopic approach in experimental study
We were able to clearly visualize the biliary tract in the two pigs. The cystic duct, common bile duct, common hepatic duct, and gallbladder were identified via the laparoscope. Local compression with our original transparent hemispherical plastic device provided a clearer view of the biliary tract. In particular, the confluence between the cystic duct and the common bile duct was sharply identified. The location and flow condition of the cystic artery were also confirmed beside the cystic duct 7–8 s after intravenous re-infusion of ICG.
Laparoscopic approach in clinical study
We were able to clearly visualize the biliary tract in the 8 patients. The cystic duct, common bile duct, and common hepatic duct were identified via the laparoscope. The gallbladder was not clearly visualized by fluorescence imaging due to inflammation or obstruction of the cystic duct. Local compression with our original transparent flat plastic device provided a clearer view of the biliary tract. In particular, the confluence between the cystic duct and the common bile duct was sharply identified. In 4 patients, the location and flow condition of the cystic artery were not easily confirmed via the laparoscope, even after division of the cystic artery. However, the flow in the cystic artery was identified in these patients after compression with the transparent flat plastic device. There were no adverse events related to the intraoperative procedure or the use of ICG itself.
Open approach in clinical study
We obtained a clear view of the biliary tract in the 4 patients. The cystic duct, common bile duct, and common hepatic duct were also identified by the PDE. In two of the patients, we were unable to obtain fluorescence imaging within the gallbladder. Local compression with the transparent hemispherical plastic device also provided a clearer view of the confluence between the cystic duct and the common bile duct. The location of the cystic artery could not be identified before its dissection. After identifying the cystic duct and artery, the flow in the cystic artery was confirmed about 10 s after intravenous re-infusion of ICG. In this approach also, there were no adverse events related to the intraoperative procedure or to the use of ICG itself.
Discussion
Indocyanine green is a dye used routinely for the evaluation of liver or cardiovascular function. ICG binds to serum protein and is absorbed and transferred to the lymphatic vessels immediately. Its peak wavelength of absorption shifts from 785 nm in water to 805 nm in serum 12. ICG is stabilized in serum, and has a peak fluorescence wavelength of 845 nm when exposed to near-infrared radiation with a wavelength of 760 nm. ICG is known to be safe at the doses used in routine clinical procedures. ICG is administered at only 1 ml/body (0.04–0.05 mg/kg) at a concentration of 2.5 mg/ml for intraoperative exploration of the biliary tract. We think that if adverse events were to occur, then they would have only a minimal influence on the human body.
Hepatocytes specifically take up ICG when it is infused intravenously, and the ICG is then secreted into the bile juice. If patients have obstructive jaundice or liver dysfunction such as steatosis, fibrosis, or portal hypertension, then fluorescence imaging of the hepatobiliary system may be complicated by delayed secretion of ICG from hepatocytes. Therefore, the timing of ICG injection is an important consideration. Mitsuhashi et al. 10 infused ICG intravenously at 1 ml/body about 30 min before cholecystectomy surgery in human patients, having determined from an animal model that this timing was optimal. This resulted in strong fluorescence in the biliary tract including the gallbladder, whereas fluorescence in the liver was slightly decreased 40 min after the intravenous injection of ICG. On the basis of this report, and our results using animals, we decided that ICG infusion at 1–2 h before surgery would result in a minimal shine-through effect from the liver. We think that this timing of ICG administration is optimal for fluorescent imaging of the hepatobiliary system.
The depth of penetration of infrared light is limited, and the thickness of tissues strongly affects the intensity of fluorescence; the light required to create fluorescence can penetrate to a tissue of only 3–5 mm 10. In the human body, the thickness of an organ or its adjacent connective tissues is affected by several factors, including obesity or edema and dense adhesion due to inflammation. Therefore, we applied an originally manufactured transparent hemispherical or flat plastic device to obtain a clearer fluorescence image. Compression with these devices can reduce the thickness of the extramural tissue, their transparency can provide clear vision, and their shape can increase the intensity of compression at local points. We believe that these devices are useful for identification of the biliary anatomy.
The results obtained by compression with these plastic devices were similar to those of ordinary IOC using a contrast medium under X-ray guidance. The advantages of this method are that it requires no cannulation into the cystic duct, no special arrangements for X-ray equipment, and no exposure to radioactivity. Fluorescence imaging can be done easily by switching to the infrared camera, and there is no need for an additional procedure. The location of blood vessels around the cystic duct can be visualized repeatedly by re-infusion of ICG. This method is very useful for exploration of the biliary anatomy without the risk of bile duct and blood vessel injury. Furthermore, when we performed ordinary IOC after fluorescence imaging, it was easy to recognize leakage of fluorescent bile juice from the small orifice in the cystic duct created for insertion of the cannula. In cases where bile duct injury is not recognized during surgery, we expect that early recognition of bile leakage will be possible using the infrared camera, thus facilitating early treatment and minimization of bile duct injury.
There are several problems that need to be considered when performing this exploration procedure. Firstly, to allow easy identification by fluorescence imaging, another reagent with a high intensity of fluorescence, or a near-infrared fluorophore such as the carboxylic acid form of IRDye 800 CW (CW800-CA, LI-COR, Lincoln, NE) 9, would be preferable. This is because it is very difficult to gain adequate recognition of the biliary anatomy using ICG in the presence of dense connective tissues or thickening due to inflammation. Secondly, although ordinary IOC can detect stones in the common bile duct as defects, this method still leaves uncertainty with the recognition of common bile duct stones. Preoperative evaluation using interventional radiology is therefore still mandatory for treatment of stones in the common bile duct. Thirdly, anatomical anomalies of the bile duct or hepatic artery are often encountered during hepatobiliary surgery. Although this method may not clearly depict such biliary anomalies, the location of the hepatic artery or its branches can be recognized by re-infusion of ICG. Further studies are needed to investigate these problems.
In conclusion, the present method using ICG is safe and allows easy identification of the biliary anatomy without the need for cannulation into the cystic duct, X-ray equipment, or the use of radioactive materials. Although fluorescence imaging is still at an early stage of development relative to established IOC, we expect that this method will become a routine procedure that is less invasive and minimizes bile duct injury.