Where do neurodevelopmental conditions fit in transdiagnostic psychiatric frameworks? Incorporating a new neurodevelopmental spectrum
Abstract
Features of autism spectrum disorder, attention-deficit/hyperactivity disorder, learning disorders, intellectual disabilities, and communication and motor disorders usually emerge early in life and are associated with atypical neurodevelopment. These “neurodevelopmental conditions” are grouped together in the DSM-5 and ICD-11 to reflect their shared characteristics. Yet, reliance on categorical diagnoses poses significant challenges in both research and clinical settings (e.g., high co-occurrence, arbitrary diagnostic boundaries, high within-disorder heterogeneity). Taking a transdiagnostic dimensional approach provides a useful alternative for addressing these limitations, accounting for shared underpinnings across neurodevelopmental conditions, and characterizing their common co-occurrence and developmental continuity with other psychiatric conditions. Neurodevelopmental features have not been adequately considered in transdiagnostic psychiatric frameworks, although this would have fundamental implications for research and clinical practices. Growing evidence from studies on the structure of neurodevelopmental and other psychiatric conditions indicates that features of neurodevelopmental conditions cluster together, delineating a “neurodevelopmental spectrum” ranging from normative to impairing profiles. Studies on shared genetic underpinnings, overlapping cognitive and neural profiles, and similar developmental course and efficacy of support/treatment strategies indicate the validity of this neurodevelopmental spectrum. Further, characterizing this spectrum alongside other psychiatric dimensions has clinical utility, as it provides a fuller view of an individual's needs and strengths, and greater prognostic utility than diagnostic categories. Based on this compelling body of evidence, we argue that incorporating a new neurodevelopmental spectrum into transdiagnostic frameworks has considerable potential for transforming our understanding, classification, assessment, and clinical practices around neurodevelopmental and other psychiatric conditions.
Difficulties with social communication, attention, learning, motor and cognitive abilities during development affect up to 15% of individuals worldwide, with many more experiencing subthreshold problems1, 2. These features are listed as criteria for conditions including autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD), intellectual disabilities, learning disorders, motor disorders (e.g., Tourette's syndrome, developmental coordination disorder), and various disorders of speech, language and communication (e.g., social pragmatic communication disorder) in traditional diagnostic manuals.
The latest editions of these manuals, the DSM-53 and the ICD-114, classify these conditions jointly as Neurodevelopmental Disorders, based on the “neurodevelopmental cluster” previously proposed within the DSM/ICD meta-structure5, 6. The primary reasons that led to their inclusion in this DSM/ICD grouping are their early age of onset, relatively persistent course, salient cognitive difficulties, and high levels of co-occurrence with one another5.
The limitations of categorical diagnostic systems for classifying neurodevelopmental and other psychiatric conditions are well documented7-13. Most notably, and of particular relevance to neurodevelopmental conditions, these systems do not provide effective tools to consider the widespread co-occurrence and overlap between purportedly distinct conditions, nor their within-disorder heterogeneity. Co-occurrence and heterogeneity pose serious barriers in both research (e.g., biomarker identification) and clinical (e.g., treatment planning) settings. Binary diagnostic categories also fail to recognize individuals with subthreshold but significantly impairing presentations, who would benefit from early support/treatment.
Transdiagnostic dimensional approaches – including the Hierarchical Taxonomy of Psychopathology (HiTOP)8, hierarchical causal taxonomies12, 14, and the Research Domain Criteria (RDoC)15, 16 – offer alternative solutions by providing empirically-based frameworks for conceptualizing psychiatric conditions dimensionally. These models include dimensional constructs that cut across multiple conditions and account for their widespread co-occurrence.
Specific clinical features of many traditionally-defined disorders (e.g., psychotic, depressive and anxiety disorders) are well classified within most transdiagnostic dimensional models, for example through spectra/dimensions such as internalizing, externalizing and psychosis17-19. However, to date, the vast majority of studies examining the co-occurrence and structure of psychiatric conditions that inform current transdiagnostic frameworks have been limited to features of only some neurodevelopmental conditions (i.e., ADHD8, 14, 20). In addition, this literature (with few notable exceptions21-23) has predominantly focused on adult samples and paid limited attention to developmental processes8, 14, 20. As a result, current transdiagnostic dimensional frameworks largely omit the clinical features that characterize neurodevelopmental conditions.
More recently, researchers and clinicians have started to consider a transdiagnostic lens toward neurodevelopmental conditions7, 24-26, rather than focusing on individual disorders. These recent conceptualizations expand upon the DSM/ICD Neurodevelopmental Disorders grouping, which includes severity ratings for conditions such as ASD and intellectual disabilities, and conceptualizations of autism as belonging to an “autism spectrum”3, 4. They are also broadly consistent with the notion of neurodiversity27-29, which originated from an advocacy-based movement and has more recently been used as an umbrella term encompassing individual differences related to neurodevelopmental conditions.
As emphasized in some of these previous accounts7, 24-26, a transdiagnostic approach to neurodevelopmental conditions can promote a better understanding of the frequent co-occurrence of these conditions and their heterogeneity, both between individuals and within an individual across time7, 24, 26. Moreover, there have as yet been limited efforts toward taking an even broader transdiagnostic approach that spans across neurodevelopmental conditions and other psychiatric conditions to place the former within a broader psychiatric framework.
Individuals with neurodevelopmental conditions often experience other psychiatric conditions, such as internalizing and externalizing problems, either concurrently or at later stages of development30, 31. Yet, these co-occurring or later emerging conditions are often neglected in clinical settings, so that people with neurodevelopmental diagnoses face significant barriers in receiving support for these additional conditions32. In response to these issues, individuals with neurodevelopmental conditions worldwide have ranked understanding the co-occurrence with other conditions and removing the above barriers as top priorities32-35. A joint transdiagnostic focus integrating both neurodevelopmental and other psychiatric conditions is essential for promoting more effective and holistic approaches to support people with neurodevelopmental and concurrent/subsequent mental health difficulties across the lifespan.
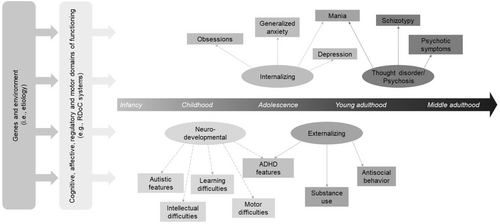
This paper aims to advance the transdiagnostic approach to neurodevelopmental conditions by formally introducing a new transdiagnostic “neurodevelopmental spectrum” and integrating it into extant transdiagnostic dimensional frameworks of psychiatric conditions (see Figure 1). We provide a broad review of the accumulating evidence in support of this proposed neurodevelopmental spectrum, including its structural (psychometric) coherence, validity and practical utility, and its placement within broader transdiagnostic frameworks of psychiatric conditions. Based on this evidence, we conceptualize this spectrum as a broad latent dimension reflecting the shared features and underpinnings of individual differences in attention, social communication, learning, motor and cognitive abilities that are most often expressed early in development, with a relatively stable developmental course, and accompanied by partly overlapping brain and socio-cognitive profiles.
We conclude that a critical mass of evidence has now accumulated supporting this new transdiagnostic neurodevelopmental spectrum. In contrast to the discrete DSM/ICD Neurodevelopmental Disorders diagnoses, this spectrum explicitly accounts for the co-occurrence between features of neurodevelopmental conditions, their heterogeneous presentation, their different severity throughout the population, and their intra-individual variability across diagnostic boundaries (i.e., an individual shifting from below to above the diagnostic threshold of a given condition, e.g. ASD, or between boundaries of different conditions, e.g. ASD and ADHD36).
Critically, our proposal also situates the neurodevelopmental spectrum into transdiagnostic frameworks of psychiatric conditions more broadly. Its explicit inclusion in these frameworks, already including spectra/dimensions capturing other clinical features, can promote a new understanding of the interplay between neurodevelopmental and other psychiatric conditions, thereby directly impacting future research and clinical practices.
It is worth noting from the outset that our use of the term “neurodevelopmental” is intended here as a label for the proposed new spectrum. The advantage of using this term is that it is in line with the terminology adopted in the DSM and ICD, and in most of the structural literature reviewed in this paper. Our use of the term does not imply that the “neural” developmental origins of these conditions have been fully elucidated, nor that other psychiatric conditions may not also have their roots in the brain or emerge early in development. For example, there have been proposals to recognize the “neurodevelopmental” origin of schizophrenia, given its overlap in etiological mechanisms with earlier-onset neurodevelopmental conditions37, 38. Rare genetic syndromes, such as fragile-X and Prader-Willi syndromes, have also been considered neurodevelopmental disorders39. The proposed neurodevelopmental spectrum does not currently consider features of these other psychiatric and genetic conditions. However, the greater consideration of a cross-disorder and developmental perspective promoted by the inclusion of this spectrum in transdiagnostic frameworks offers the potential to enhance our understanding of the developmental pathways to other psychiatric conditions and the co-occurrence between a broad range of clinical features (including neurodevelopmental and behavioral challenges in individuals with genetic syndromes).
STRUCTURAL EVIDENCE
Building on research and clinical observations regarding the co-occurrence among neurodevelopmental conditions40 and between these conditions and other psychiatric conditions31, 41, a growing number of factor analytic studies have included assessments of neurodevelopmental features. This has allowed for investigation of covariation within and across neurodevelopmental and other psychiatric conditions, with available studies providing key evidence for a neurodevelopmental spectrum and supporting its placement among other more established spectra/dimensions in transdiagnostic frameworks.
Studies that identified a neurodevelopmental factor
A factor explicitly called “neurodevelopmental” was first delineated alongside other psychiatric dimensions in a study using exploratory factor analysis on items of the Child Behavior Checklist (CBCL) in almost 10,000 children from the Adolescent Brain Cognitive Development (ABCD) study25. Results showed a transdiagnostic structure including a neurodevelopmental factor along with externalizing, internalizing, somatoform and detachment factors. This neurodevelopmental factor included features of ADHD (e.g., inattention, hyperactivity), aspects of motor disorders (e.g., poor coordination, twitching), features conceptually overlapping between ASD and obsessive-compulsive disorder (OCD) (e.g., repetitive thoughts/obsessions and behaviors/compulsions, strange ideas), and poor school performance. A narrower inattentive neurodevelopmental factor, mainly defined by ADHD features, was also delineated using Adult-Self Report (ASR) items in adult parents of ABCD participants.
Interestingly, these neurodevelopmental factors first emerging in three-factor models were highly correlated with both broad internalizing and externalizing factors in the higher-level two-factor models. This finding suggests that the newly emerging factor is not a mere partition of a higher-order externalizing spectrum/dimension, but rather has associations with both internalizing and externalizing problems.
The neurodevelopmental factor was replicated in six subsequent studies. Using an equivalent analytic approach to the aforementioned ABCD study25, a neurodevelopmental factor capturing inattention, hyperactivity/impulsivity, executive function problems, and learning difficulties was identified in a transdiagnostic sample enriched for problems with attention and learning42. This factor emerged along with internalizing and social maladjustment factors. A study on the Avon Longitudinal Study of Parents and Children (ALSPAC) cohort at ages 7 and 13 years showed superior fit of correlated factor and bifactor models including a neurodevelopmental factor (ADHD and ASD scales) alongside emotional and behavioral factors relative to models only including two emotional and behavioral/neurodevelopmental factors43.
Further, two studies of several hundreds of thousands children and adults from the Swedish population tested a neurodevelopmental factor (defined by diagnoses) within bifactor structures also including other specific factors (e.g., externalizing, internalizing) and a general psychopathology (p) factor44, 45. One of these studies also modeled an ADHD factor separately and showed significantly stronger phenotypic and genetic associations of this factor with the neurodevelopmental factor than with externalizing and internalizing factors when controlling for p, congruent with the inclusion of ADHD in a neurodevelopmental spectrum (rather than in the externalizing spectrum).
Another recent study of Swedish adult twins identified a neurodevelopmental factor, capturing features of ADHD (inattention and disorganization) and ASD (social difficulties), along with internalizing, substance and impulsivity factors46. Finally, a recent study exploring the data-driven hierarchical structure of the full set of DSM-5 clinical features in separate primary and hold-out adult population-based samples revealed a neurodevelopmental factor along with other major transdiagnostic dimensions47. This broad neurodevelopmental factor included features of ASD, ADHD, and learning, communication, language and speech difficulties.
Findings from these studies are also in line with two additional studies that modeled a neurodevelopmental factor using various neurodevelopmental features and traits through confirmatory factor analysis48, 49. However, as these studies did not include other psychiatric features alongside neurodevelopmental indicators, they cannot be used to determine the placement of the neurodevelopmental factor within a broader transdiagnostic structure.
Other evidence supporting the delineation of a neurodevelopmental spectrum
Several other lines of research, despite not explicitly using the term “neurodevelopmental”, support the integration of the proposed spectrum into transdiagnostic dimensional models. First, an exploratory factor analysis50 and subsequent confirmatory factor analysis51 of the CBCL and a questionnaire assessing ASD and related developmental problems (Children's Social Behavior Questionnaire), in an epidemiological child and adolescent cohort, found “attention and orientation” and ASD factors, together with internalizing, externalizing and p factors. Of note, ADHD features did not cluster with externalizing, but rather with orientation features of ASD, and several ASD scales had significant loadings from both the attention and orientation factor and the ASD factor. Moreover, item-level analyses suggested that ASD and ADHD features clustered together in a model including an ASD/ADHD factor and internalizing and externalizing factors, and only differentiated into two separate factors in models with at least eight narrower factors52. This indicates that some features of ASD and ADHD may form a broad spectrum that may be further differentiated in more specific factors52.
Second, studies incorporating both personality and mental health measures have identified factors similar to the neurodevelopmental spectrum. A recent exploratory factor analysis of items from ADHD, ASD, and questionnaires measuring normal-range personality and psychopathology in adults, found that inattention, hyperactivity/impulsivity, and pragmatic language difficulties clustered together, whereas aloofness loaded onto detachment factors53, 54. Another study in children and adolescents found that items of distractibility, organization, achievement, hyperactivity, and intelligence loaded together on an “organization” factor and separately from items belonging to positive personality, behavior problems, and internalizing factors55.
Third, several previous studies using bifactor models in samples of children, adolescents and adults showed that indicators of ASD or ADHD (especially inattention) were solely or predominantly captured by the p factor, with minor or non-significant loadings onto the externalizing factor56-64. This suggests that ASD and ADHD may be better captured by a different factor not modeled in these studies, such as a neurodevelopmental factor. Similarly, factor analytic studies using measures from the Achenbach System of Empirically Based Assessment (ASEBA) in dozens of samples from preschool to old adult age, and across societies and raters, indicate that the attention problems scale is not subsumed within the externalizing scale (aggregating rule breaking and aggression) or the internalizing scale (anxious/depressed, withdrawn/depressed, somatic complaints)21, 65-71. This is consistent with studies identifying a factor capturing features of ADHD separately from externalizing factors72-80.
Summary of the structural evidence
Overall, the studies reviewed here provide accumulating evidence supporting the robust factor structure of the neurodevelopmental spectrum alongside other transdiagnostic spectra/dimensions, providing a strong argument for the inclusion of this spectrum in transdiagnostic dimensional frameworks. Available studies indicate that features of ADHD, ASD, intellectual disability, and learning, communication and motor disorders can be conceptualized within this dimension (see Table 1).
| Diagnoses | Features/symptoms/traits | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ADHD | ASD | LD | ID | Motor | ODD | Inatt | Hyp/Imp | Aut | Soc | Tho | Lear | Cog | Com | Mot | Con | Opp | Other | |
| Neurodevelopmental factor | ||||||||||||||||||
| First order | ||||||||||||||||||
| Martin et al48 | + | + | + | + | ||||||||||||||
| Michelini et al25 | + | + | + | + | + | + | + | |||||||||||
| Addicoat et al49 | + | + | + | + | ||||||||||||||
| Holmes et al42 | + | + | + | + | ||||||||||||||
| Pettersson et al46 | + | + | + | |||||||||||||||
| Forbes et al47 | + | + | + | + | + | |||||||||||||
| Bifactor | ||||||||||||||||||
| Du Rietz et al44 | + | + | + | + | ||||||||||||||
| Pettersson et al45 | + | + | ||||||||||||||||
| Riglin et al43 | + | + | + | |||||||||||||||
| Similar factor | ||||||||||||||||||
| First order | ||||||||||||||||||
| Hartman et al72 | + | + | + | + | ||||||||||||||
| Lahey et al79 | + | + | + | |||||||||||||||
| Hartman et al52 | + | + | + | |||||||||||||||
| Ivanova et al67 | + | |||||||||||||||||
| Farmer et al80 | + | + | ||||||||||||||||
| Slobodskaya55 | + | + | ||||||||||||||||
| Noordhof et al50 | + | + | ||||||||||||||||
| Niarchou et al74 | + | + | ||||||||||||||||
| Pettersson et al75 | + | + | ||||||||||||||||
| Haltigan et al71 | + | |||||||||||||||||
| Moore et al76 | + | + | + | + | + | |||||||||||||
| Clark et al78 | + | + | + | + | ||||||||||||||
| Stanton et al53 | + | + | + | + | ||||||||||||||
| Stanton et al54 | + | + | + | + | ||||||||||||||
| Bifactor | ||||||||||||||||||
| Murray et al73 | + | + | ||||||||||||||||
| Bloemen et al51 | + | + | ||||||||||||||||
| McElroy et al70 | + | |||||||||||||||||
| Miller et al77 | + | |||||||||||||||||
- Studies are split between those that modeled a neurodevelopmental (or similar) factor as a first-order one (e.g., within correlated factor models) and those that modeled it as a specific factor in a bifactor model (i.e., where some of the variance in relevant indicators was captured by a general psychopathology factor).
- The + means that the indicator was included in the analysis and loaded ≥0.30 onto neurodevelopmental (or similar) factor. ADHD – attention-deficit/hyperactivity disorder, ASD – autism spectrum disorder, LD – learning disorders, ID – intellectual disabilities, Motor – motor disorders, ODD – oppositional defiant disorder, Inatt – inattention/attention problems, Hyp/Imp – hyperactivity/impulsivity, Aut – autism spectrum features, Soc – social problems, Tho – thought problems, Lear – learning difficulties, Cog – general or specific (e.g., executive functioning) cognitive abilities, Com – communication, language and speech difficulties, Mot – motor features, Con – conduct problems, Opp – oppositionality, Other – features of poor functioning or general psychopathology not belonging to specific conditions.
The studies reviewed here suggest the inclusion of ADHD features, particularly inattention, in the proposed neurodevelopmental spectrum, with impulsivity being captured by both neurodevelopmental and externalizing spectra in some studies25, 42. This is inconsistent with studies that modeled ADHD exclusively as an indicator of externalizing factors81-89, which informed current transdiagnostic frameworks typically placing ADHD under a (disinhibited) externalizing spectrum14, 18.
However, it should be noted that, unlike recent studies identifying a neurodevelopmental or neurodevelopmental-consistent factor, the studies placing ADHD under externalizing factors did not include features of other neurodevelopmental conditions. Further, these studies only examined diagnoses or scale total scores, resulting in only one or two ADHD indicators – an insufficient number for the emergence of a separate neurodevelopmental/ADHD factor. The use of diagnoses in this context may also be particularly problematic, because children with ADHD with high hyperactivity-impulsivity are more likely to receive an ADHD diagnosis, especially when comorbid with oppositional defiant disorder (ODD) or conduct disorder (CD), compared to children only showing inattentive features, who are often misdiagnosed or underdiagnosed90. This artificially inflates the covariation between ADHD and ODD/CD and may result in an incorrect placement within the externalizing spectrum.
Crucially, before the DSM-5 and ICD-11, ADHD and ASD could not be diagnosed together in the same individual, and, since ASD is typically diagnosed earlier in development, an additional ADHD diagnosis was not possible91. Studies including ADHD diagnoses prior to the latest editions of those diagnostic manuals, therefore, likely missed a sizeable portion of the ADHD population with predominant neurodevelopmental and autistic features.
A few limitations of the available literature should be noted. Most of the studies used samples with wide age ranges and cross-sectional designs, precluding the examination of developmental effects. This limitation is common to many studies on the structure of psychiatric conditions, but especially problematic for delineating a neurodevelopmental spectrum with its roots in early development. Another limitation is that the majority of studies focused on ADHD and to a lesser extent ASD, while only a minority included learning, motor, intellectual and communication difficulties (see Table 1). While the few available studies consistently support the inclusion of these latter conditions in a neurodevelopmental spectrum, future studies with broad assessments of neurodevelopmental features are warranted.
VALIDITY EVIDENCE
Besides evidence of its structural coherence, the proposed neurodevelopmental spectrum is supported by multiple lines of research establishing its validity, in line with validators commonly used in psychiatric nosology5, 17-19.
Genetics
Neurodevelopmental conditions run in families, with higher rates in family members of affected individuals92. Twin studies provide strong evidence that neurodevelopmental conditions are highly heritable (with an average meta-analytic heritability of 0.66, ranging from 0.62 for specific learning disorders to 0.86 for intellectual disabilities).
Further, these conditions share a substantial degree of genetic influences with one another (the meta-analytic genetic correlation across neurodevelopmental conditions is 0.36, ranging from 0.07 for ADHD-specific learning disorders to 0.90 for ADHD-motor disorders)92, consistent with a neurodevelopmental spectrum, and show a more modest genetic overlap with other psychiatric conditions (e.g., 0.10 to 0.31 with schizophrenia, but also 0.62 with disruptive disorders)1, 93-96.
Notably, the strong shared genetic influences between ASD, ADHD, the broader autism phenotype, intellectual disabilities; coordination, speech and language problems; and other social problems95, 97-104 can be captured by a latent genetic neurodevelopmental factor105. Recent meta-analyses and reviews of twin and family studies indicate that up to ~80% of the phenotypic correlation between ASD, ADHD and other neurodevelopmental conditions, as well as conditions that also typically emerge earlier in development, such as OCD, can be explained by shared genetic influences92, 93, 106.
Consistent with findings from twin studies, recent genome-wide association studies (GWAS) have also found evidence of considerable genetic overlap between neurodevelopmental conditions at the level of common single nucleotide polymorphisms (SNPs)107-111. In the largest GWAS conducted on ASD to date (18,000 cases and 28,000 controls), one of the most robust genetic correlations was between ASD and ADHD (rg=.36)108.
To model the genetic covariance structure among multiple conditions/traits (including ASD and ADHD) using GWAS summary statistics, factor analytic methods such as genomic structural equation modeling (GenomicSEM) have been developed112. Recent findings using this approach have shed new light on the genetic basis of a neurodevelopmental factor that appears to include ASD, ADHD and Tourette's syndrome109, 113-115. Further, findings from GenomicSEM studies have thus far consistently converged on the existence of a neurodevelopmental factor that is genetically separable from other factors (i.e., internalizing, externalizing, psychosis114, 115).
Several of the genes associated with ADHD107 and ASD108 are also more generally involved in neurodevelopmental processes. Regarding ADHD, FOXP2 is involved in synapse formation and speech and learning development108, 116-118; SORCS3 encodes a brain-expressed transmembrane receptor important for neuronal development and plasticity119, 120; SEMA6D appears to play a role in neuronal wiring during embryonic brain development120, 121; and ST3GAL3 and MEF2C have been associated with severe intellectual disability120, 122-124. Similarly, regarding ASD, strong enrichment was observed for regulatory elements in the brain regions involved in prenatal neurodevelopment108. This is in line with studies of genes (e.g., SHANK3, MEF2C) that disrupt early synaptic function in genetic syndromes such as the Rett syndrome and the Phelan-McDermid syndrome, which often show intellectual disability, autistic features, and ADHD features125.
Building on GWAS discoveries, polygenic risk scores seem to show robust associations across neurodevelopmental features, rather than just for individual neurodevelopmental conditions126, 127. For example, in a large cohort study of children, an ADHD polygenic risk score was associated with inattention and hyperactivity but also language difficulties, and an ASD polygenic risk score was associated with inattention, hyperactivity, language and motor difficulties, whereas a schizophrenia polygenic risk score did not show significant associations with neurodevelopmental features128. Both ADHD and ASD polygenic risk scores further predicted a neurodevelopmental spectrum based on exploratory factor analysis delineated in the ABCD study129.
It is important to note that genomic studies of most psychiatric conditions are still in their infancy. As such, the genetic architecture of neurodevelopmental and other psychiatric conditions may change as sample sizes increase and new genomic data become available. Although GenomicSEM research has now been conducted with ASD and ADHD, other conditions that are hypothesized to be included in the neurodevelopmental spectrum, such as motor disorders and intellectual disabilities, have yet to be considered, due to the absence of GWAS of these phenotypes. It is critical that these omissions are addressed in future genomic studies of the neurodevelopmental spectrum.
Environmental risk factors
While the above-reviewed research indicates relatively large genetic influences for neurodevelopmental conditions and their covariation, meta-analytic evidence also demonstrates modest to moderate environmental influences92. Associations have been found of various forms of pre- and peri-natal stress130-134, preterm birth135, 136 and environmental toxicant exposure (e.g., lead)137-141 with neurodevelopmental conditions, including ASD, ADHD, intellectual disabilities, and learning and motor difficulties, as well as associated cognitive profiles. This pattern is consistent with an underlying dimension of liability to all neurodevelopmental conditions influenced by the aforementioned environmental exposures.
However, there are two important caveats when interpreting this evidence. First, it remains unclear whether and how specific these associations are to clinical features of the proposed neurodevelopmental spectrum relative to features captured by other spectra/dimensions133, 142. Shared environmental risk factors, similar to genetics, may contribute to the co-occurrence between neurodevelopmental conditions and other psychiatric conditions. Yet, it is also possible that the same environmental factors are associated with different transdiagnostic conditions at different points in development, pointing to some specificity. For example, the same environmental exposure may increase risk for neurodevelopmental conditions in infancy/childhood and for psychosis in adolescence/adulthood. Second, establishing an association between environmental risk factors and neurodevelopmental conditions does not necessarily imply a causal effect. For example, accounting for familial and other confounders often results in attenuated associations135, 143. However, a recent systematic review of twin and sibling studies, which controlled for familial and other shared confounders, did find suggestive evidence of a causal effect of pre-natal exposures for ASD and ADHD130.
Developmental course
Additional evidence supporting the validity of the proposed neurodevelopmental spectrum pertains to the similarities in developmental course displayed by features clustering in this dimension. A key characteristic of all neurodevelopmental conditions is that they typically emerge early in development. The first features of some conditions – such as ASD, language and communication disorders, and developmental coordination disorder – are often recognizable before school age144-150. Other conditions, such as ADHD and learning disabilities, may be detected during the preschool period, but formal diagnosis usually does not occur until the child enters the school system and the skills associated with these conditions are evaluated31, 151. Nevertheless, on average, neurodevelopmental features tend to emerge earlier than most other psychiatric conditions152 (see Figure 1).
Regarding developmental trajectories, individuals with neurodevelopmental conditions tend to show persisting features over development, with some degree of improvement often seen with maturation31, 153, 154. Rates of diagnostic stability vary widely between studies (from ~20% to 100%)31, 155-159, particularly for ADHD and ASD. This instability may be explained by methodological differences, with lower persistence rates generally reported in population-based samples than in clinical samples and in studies relying on strict diagnostic thresholds31, 36, 160, 161. Nevertheless, research has shown that most individuals with neurodevelopmental conditions show worse functional outcomes into adulthood relative to neurotypical individuals31, 154, 162, 163.
With regard to specific clinical features, inattention and socio-communication difficulties follow a relatively stable developmental pattern154, 164, while other features may change or be manifested differently with age and development, or even be replaced by features of other psychiatric conditions (heterotypic continuity). As an example, motor hyperactivity tends to decline over childhood and adolescence, but is often replaced by a feeling of inner restlessness in adulthood, which is also common in internalizing conditions31. In addition, it has been suggested that support strategies and interventions may not alter the natural course of neurodevelopmental conditions, but rather provide skills to compensate for stable underlying problems31.
Altogether, evidence suggests similarities in developmental course between different neurodevelopmental conditions, namely an early onset and persistent course, with some degree of heterogeneity among individuals with the same condition7, 165, 166. Transdiagnostic approaches seeking to parse individuals with different neurodevelopmental conditions through more specific data-driven subdimensions cutting across diagnostic boundaries are particularly valuable for characterizing variability in developmental course7, 167. For example, individuals with features of multiple neurodevelopmental conditions – consistent with high score on an overarching neurodevelopmental spectrum – commonly display more persisting symptom trajectories and worse long-term outcomes, including psychiatric comorbidities153, 154, 168. Future research should systematically evaluate the presence of different transdiagnostic neurodevelopmental subdimensions and how they may be linked to other psychiatric conditions, which could inform the design of transdiagnostic early interventions and support strategies.
Temperamental antecedents and personality
There appears to be both consistency and specificity in the temperamental traits that characterize neurodevelopmental conditions, though most of the existing research has been limited to ASD and ADHD, and to a lesser extent intellectual disabilities and communication disorders.
Lower levels of effortful control are common across all neurodevelopmental conditions169-178. Higher levels of negative emotionality are also frequent across these conditions, though the expression of this domain may partly differ across conditions, with distress, fear, shyness and sadness predominant in ASD and intellectual disabilities, while anger predominates in ADHD169, 179. Positive emotionality/surgency also shows specificity across neurodevelopmental conditions, with higher levels in ADHD but lower levels in ASD and intellectual disabilities169, 170, 178-181.
Although less common, longitudinal prospective studies highlight early temperamental indicators of lower effortful control, and higher negative emotionality and positive emotionality/surgency, as predicting ADHD symptom trajectories182; and lower effortful control in toddlerhood as predicting ASD diagnosis in early childhood183. Of note, lower effortful control and higher negative emotionality have also been associated with other psychiatric conditions, and may represent more general transdiagnostic indicators182, 184.
Cognitive and socio-emotional profiles
Neurodevelopmental conditions are characterized by difficulties in cognition, social interaction, and communication that emerge early in development and persist into later life5, 146. Early cognitive challenges are a key feature of these conditions, though the nature of challenges may vary among different conditions, ranging from impairments specific to core processes and abilities, while other capacities are relatively preserved, to more generalized problems185-187.
Executive functioning deficits cut across ASD, ADHD, motor disorders, and learning disabilities7, 31, 188, 189. The ABCD study found that, among transdiagnostic dimensions, the neurodevelopmental factor showed the strongest association with executive functioning190.
Studies directly comparing children with ASD and ADHD showed similarities during early development in attention, response inhibition, working memory, verbal fluency, preparatory processes, and concept formation, with some differences more likely to be quantitative rather than qualitative145, 191, 192. Similar cognitive challenges have also been reported in other neurodevelopmental conditions, such as language disorders, developmental coordination disorder, and Tourette's syndrome193-195, but transdiagnostic comparison studies are lacking.
Early atypicalities in sensory processing (e.g., hyper-sensitivity) have been consistently reported in autistic children196, 197, but are also found in children with ADHD198. Further, motor skills, such as motor coordination, are impaired across developmental coordination disorder, Tourette's syndrome, ASD and ADHD145, 158, 199, and communication/language problems characterize not just language and speech disorders but also to some extent ASD and ADHD145, 195, 200.
With regard to social skills, children with ASD, ADHD, motor disorders and learning disabilities show social impairments relative to their peers7, 193, 201, 202. There does appear to be some specificity in social impairment, with autistic children showing more atypical social skills7, 189, 203, 204, whereas children with ADHD show relatively intact social skills knowledge but more maladaptive social behavior205. Perhaps due to impairments in self-regulation and inhibitory control206, both ASD and ADHD are also associated with elevated emotional dysregulation, including emotional lability and irritability207-209.
Although there is evidence of characteristic cognitive and socio-emotional profiles for neurodevelopmental conditions, similar cognitive challenges have also been found for other psychiatric conditions51, 210. However, because few studies comprehensively examined cognitive functions across the above conditions (with the notable exception of ADHD and disruptive behavior disorders211, 212), the specificity of these cognitive profiles to neurodevelopmental conditions remains to be clarified in future transdiagnostic studies. Another important direction will be to address the wide heterogeneity in cognitive and socio-emotional profiles across neurodevelopmental conditions more systematically, by developing multidimensional models that integrate both clinical features and functioning abilities.
Neurobiological profiles: neuroimaging
Structural and functional magnetic resonance imaging (MRI) studies suggest largely shared patterns of brain structure and functioning in networks important for executive function and cognitive/motor control across neurodevelopmental conditions213-217, supporting the proposed neurodevelopmental spectrum.
Specifically, similar patterns of grey matter structure have been observed in frontal, temporal, parietal and striato-thalamic networks supporting cognitive control and goal-directed decision-making across ASD and ADHD218-224. Mega- and meta-analyses have found associations of ASD and ADHD with lower grey matter volume in ventromedial orbitofrontal cortex and basal ganglia, amygdala and hippocampus, and with lower cortical surface area and thickness in frontal, temporal and parietal regions220-222, 225-232. Neuroanatomical findings may, however, vary with development (e.g., evidence of increased total brain volume in ASD during infancy/early childhood224) and have been somewhat less consistent in studies of ASD compared to ADHD.
Few studies have compared neurodevelopmental conditions directly, but these findings are consistent with a recent cross-disorder study showing commonalities in cortical regions implicated in socio-emotional and executive functions across ASD and ADHD (as well as OCD)233. Additional cross-disorder mega- and meta-analyses further indicate a range of structural brain features shared between ASD and ADHD, such as lower cortical thickness and surface area, though some divergent findings have also been observed, possibly due to the fact that some studies analyzed summary statistics rather than raw data234-236.
While the majority of studies have focused on ASD and ADHD, structural MRI studies of other neurodevelopmental conditions have shown more mixed findings, likely owing to the use of smaller samples237-242. Larger comparative studies investigating all neurodevelopmental conditions, as well as other psychiatric conditions, are needed.
As to brain functioning, atypical activations within fronto-striatal brain circuitry and basal ganglia appear to be most commonly implicated across ASD, ADHD, and speech and language disorders. Meta-analyses show underactivation related to cognitive and inhibitory control in lateral/medial fronto-striatal networks in ADHD222, 243, 244. Similarly, a whole-brain meta-analysis of functional MRI studies of cognitive control in ASD found underactivation in salience and executive networks, including lateral and medial frontal regions and left cerebellum, and overactivation in right temporo-parietal regions, including areas of the default-mode network218, 221. Moreover, shared reductions in dorsolateral prefrontal cortex and precuneus activation during higher-order cognitive functions and resting state have been observed across ASD and ADHD245-248.
Fewer studies have investigated the neural underpinnings of other neurodevelopmental conditions using functional MRI. Regarding specific learning disabilities, dyslexia has been associated with primarily left-lateralized underactivation in lateral temporal, inferior parietal, and fusiform regions, as well as overactivation in motor cortex and the anterior insula249-251, whereas dyscalculia is associated with number-relevant parietal regions and prefrontal and occipital regions252. Initial data in Tourette's syndrome suggest that functional dysregulation in basal ganglia and limbic regions related to the suppression of tics may overlap with functional abnormalities and related cognitive control difficulties seen in ADHD253.
Shared alterations across ASD and ADHD have been found in structural connectivity, particularly in white matter tracts connecting prefrontal regions to other regions254, 255, as well as in functional connectivity in large-scale brain networks, particularly in the default-mode network and fronto-parietal attention-related salience networks248, 256-261. Such cross-disorder overlap is also reflected in recent data from the ABCD study showing the association between a neurodevelopmental factor derived from exploratory factor analysis25 and resting state functional connectivity involving the default-model, cingulo-opercular and dorsal attention networks262. Associations with functional connectivity were significant even after controlling for a general psychopathology factor and did not emerge for other psychopathological dimensions (e.g., internalizing, externalizing), suggesting the specificity of these atypical functional connectivity profiles to neurodevelopmental features.
Functional connectivity studies in motor disorders are somewhat more limited, but those directly comparing developmental coordination disorder and ADHD have found evidence for shared abnormalities across disorders in motor circuitry, pointing to a common neural substrate263, 264.
Overall, the available evidence indicates an overlap in candidate diagnostic biomarkers of brain structure and functioning across neurodevelopmental conditions, particularly ASD and ADHD. Structural and functional atypicalities in frontal and striato-thalamic regions implicated in attention and cognitive control, and abnormalities in resting-state functional connectivity networks, particularly the default mode and dorsal attention networks, may be a unifying feature across a neurodevelopmental spectrum. While initial evidence points to brain patterns that may be common across neurodevelopmental features but discriminate them from other psychiatric features262, future studies should systematically assess the extent of possible neurodevelopmental-specific neuroimaging biomarkers.
Neurobiological profiles: neurophysiology
Evidence from neurophysiological studies, particularly based on electroencephalography (EEG), complements knowledge from neuroimaging studies. Reductions in event-related potentials (ERP) amplitudes reflecting early sensory perception, such as N1 and mismatch negativity (MMN), have been commonly reported in ASD265, 266 and dyslexia267, 268, whereas associations with ADHD and developmental coordination disorder appear more consistent for reduced MMN265, 269 than for N1 components270.
Atypical N170 amplitudes in response to facial stimuli have been studied almost exclusively in ASD, and large studies in other conditions are needed271, 272. Studies of ERPs indexing goal-directed behavior indicate reduced N2 and error-related negativity (ERN) components in ASD266, 273, ADHD273, 274, specific learning disabilities275, 276 and developmental coordination disorder277, whereas increased ERNs are commonly associated with Tourette's syndrome273. The latter finding might be explained by the close link between Tourette's syndrome and OCD, as OCD is also associated with increased ERN, potentially suggesting that Tourette's syndrome might be jointly captured by internalizing and neurodevelopmental spectra. Further, reduced P3 components in response to visual and auditory stimuli have been repeatedly associated with ASD278, 279, ADHD280, 281, specific learning disabilities276, Tourette's syndrome282, and developmental coordination disorder269, 283, 284.
With regard to resting-state EEG studies, elevated power in slow oscillations (delta and theta), thought to reflect delayed cortical maturation, have repeatedly been associated with ASD285, ADHD286, 287, and learning difficulties288, 289. Reduced alpha and beta power have also commonly been associated with these conditions290-292, although findings for alpha power have been more mixed in ADHD287, 293. Emerging findings suggest shared alterations in intra-individual EEG variability294, 295 and EEG connectivity296-298 between ASD and ADHD. Similarly, a recent study of children with ASD or ADHD and controls found a data-driven cluster largely reflecting a transdiagnostic neurodevelopmental subgroup based on functional connectivity measured with magnetoencephalography (MEG)299.
These findings support the validity of the proposed neurodevelopmental spectrum, in that they delineate neurophysiological profiles mapping onto neural mechanisms shared across neurodevelopmental conditions. However, similar to the neuroimaging literature, the strongest evidence pertains to ASD and ADHD, warranting replication and extension in transdiagnostic studies of neurodevelopmental and other psychiatric conditions.
Other neurobiological profiles
The literature on peripheral diagnostic biomarkers provides further evidence in support of the neurodevelopmental spectrum. Meta-analyses and reviews indicate that reduced levels of serum vitamin D levels300-303 and blood zinc levels304-307 are associated with ASD, ADHD, intellectual and learning difficulties. Blood levels of brain-derived neurotrophic factor (BDNF) were found elevated in both ASD and ADHD308, 309. However, the strength of the evidence for these biomarkers varied in these meta-analyses and was often rated as weak, indicating that larger and more rigorous studies are needed.
Service organization and efficacy of support and intervention approaches
Patterns of service organization and efficacy of support and intervention strategies provide additional evidence for the validity of the proposed neurodevelopmental spectrum.
Given the high rates of co-occurrence across neurodevelopmental conditions, the need for multifaceted professional care that adequately addresses varied symptom presentations and needs beyond diagnostic categories has been widely advocated310, 311. In fact, in several countries, clinical services are already organized to provide care for features spanning the neurodevelopmental conditions312, with service-user organizations actively advocating for a shift toward transdiagnostic neurodevelopmental services in countries where care is still based on discrete conditions313.
Evidence from treatment studies shows that stimulant medication broadly improves features of inattention, hyperactivity and impulsivity314; academic performance in math productivity, math accuracy and reading speed315; outcomes related to motor coordination316, and cognitive performance in children with ADHD but also ASD317. These effects across neurodevelopmental conditions suggest that medication is not acting upon mechanisms specific for one diagnostic category, but instead on shared underlying processes315, 317, 318. It is important to note, however, that some core features of ASD, such as social interaction and stereotypical behaviors, do not show improvements with stimulants318, highlighting heterogeneity.
Regarding response to psychosocial interventions, initial evidence indicates that transdiagnostic traits (executive functioning and emotion regulation) predict efficacy of an intensive behavioral treatment program targeting school readiness over and above ASD and ADHD diagnoses206, further supporting the validity of the proposed spectrum. Since most transdiagnostic studies have focused on ASD and ADHD, additional research is needed to conclusively determine whether transdiagnostic psychosocial interventions can provide similarly efficacious benefits across other neurodevelopmental conditions.
Summary of the validity evidence
Overall, there is a broad degree of similarity in genetic, neuroimaging, neurophysiological and other biomarkers, as well as in developmental, cognitive, socio-emotional, temperamental/personality profiles, and patterns of service organization and treatment efficacy, across neurodevelopmental conditions (see Table 2). Evidence is most convincing for ASD and ADHD, as these conditions have been investigated to a much greater extent than other neurodevelopmental conditions.
| Diagnoses/features | Neurodevelopmental (or similar) factor | ||||||
|---|---|---|---|---|---|---|---|
| ADHD | ASD | Learn | ID | Comm | Motor | ||
| Genetics | |||||||
| Family/twin studies | ++ | ++ | + | + | + | + | + |
| Molecular genetics/genomics | + | + | + | + | + | ||
| Environmental risk | |||||||
| Early stress exposure | ++ | ++ | + | + | + | ||
| Preterm birth | + | + | |||||
| Toxicant exposure (e.g., lead) | + | ++ | + | + | |||
| Developmental course | |||||||
| Early age of onset | + | ++ | + | + | ++ | ++ | |
| High chronicity/stability | + | ++ | + | + | ++ | + | |
| Temperamental antecedents | |||||||
| Low effortful control | ++ | + | + | + | + | + | |
| High negative emotionality | ++ | ++ | + | + | + | + | |
| High positive emotionality | + | ||||||
| Low positive emotionality | + | + | |||||
| Cognitive and socio-emotional difficulties | |||||||
| Executive functioning | ++ | ++ | ++ | + | ++ | + | |
| Sensory processing | ++ | ++ | |||||
| Motor coordination | + | + | ++ | ||||
| Language problems | + | + | ++ | ||||
| Theory of mind | + | ++ | |||||
| Emotional dysregulation | ++ | + | |||||
| Neurobiology | |||||||
| Brain volumes | ++ | + | + | + | |||
| Brain activity (fMRI) | ++ | ++ | + | + | + | ||
| Structural connectivity | + | + | |||||
| Functional connectivity | + | + | + | + | |||
| Event-related potentials | ++ | ++ | + | + | + | ||
| EEG spectral power | + | + | + | + | + | ||
| Other biomarkers | |||||||
| Reduced serum vitamin D | + | + | + | + | |||
| Reduced blood zinc | + | + | + | + | |||
| Elevated BDNF expression | + | + | |||||
| Service organization and treatment | |||||||
| Broad neurodevelopmental services | + | + | + | + | + | + | |
| Efficacy of stimulant medication | ++ | + | + | ||||
- ++ means repeatedly replicated finding, + means some evidence for effect. ADHD – attention-deficit/hyperactivity disorder/features, ASD – autism spectrum disorder/ features, Learn – learning disorders/problems, ID – intellectual disabilities, Comm – communication disorders/problems, Motor – motor disorders/features, fMRI – functional magnetic resonance imaging, EEG – electroencephalography, BDNF – brain-derived neurotrophic factor.
Many studies support a dimensional approach, highlighting within-diagnosis variability and between-diagnosis overlap, motivating the search for shared patterns of brain-behavior associations across neurodevelopmental conditions. However, most studies have only considered one condition or symptom dimension in small samples, highlighting an acute need for larger studies using transdiagnostic samples with neurodevelopmental and other psychiatric conditions.
Besides broad similarities supporting the coherence of a neurodevelopmental spectrum, findings suggesting some differences between neurodevelopmental conditions, if replicated, would be consistent with the possible delineation of subdimensions (e.g., inattention, social difficulties) within this broad spectrum.
Two points are worth noting. First, multiple and different causes and configurations of underlying mechanisms may give rise to shared phenotypes across neurodevelopmental and other psychiatric conditions (i.e., equifinality319). At the same time, the same underlying cause or mechanism may result in phenotypic variation and different outcomes within neurodevelopmental conditions (i.e., multifinality319). Further transdiagnostic research using etiological and developmental approaches will be important for elucidating these equifinal and multifinal pathways, and for informing clinical decisions and applications based on underlying mechanisms and developmental processes.
Second, while the reviewed validity evidence points to commonalities across neurodevelopmental conditions, the extent of the overlap with other psychiatric conditions remains largely unclear. For example, similar temperamental, cognitive and neural profiles may also be found in the context of later-onset psychiatric conditions, such as depressive and psychotic disorders9. Yet, studies of other psychiatric conditions rarely examine whether these findings may be explained by co-occurrence with earlier-onset features of neurodevelopmental conditions. The systematic inclusion of neurodevelopmental features and conditions in future longitudinal transdiagnostic studies will be crucial to clarify this issue.
UTILITY EVIDENCE
Although a DSM/ICD-based categorical approach for research and practice still represents the status quo, transdiagnostic dimensional approaches are increasingly being adopted in research as well as clinical services for neurodevelopmental conditions7, 26, 320, supported by growing evidence suggesting their utility.
Reliability and measurement
To contextualize the potential utility of dimensional alternatives, it is useful to consider evidence for the limited reliability of categorically-defined neurodevelopmental conditions. Most evaluations of reliability of these conditions have focused on ASD and ADHD, whereas data are lacking for other neurodevelopmental conditions (with a few exceptions321). Interrater reliability (i.e., the extent to which two raters agree) has generally been found to be low to barely adequate for both ASD322-325 and ADHD326-328, and even lower for specific ADHD subtypes329.
Interrater reliability estimates for ASD and ADHD diagnoses are also generally lower than for other psychiatric diagnoses323, 324, 330, 331. One important consideration is that, unlike diagnoses of most other psychiatric conditions, diagnoses of neurodevelopmental conditions are often made using parent and other informant (e.g., teacher) reports rather than relying solely on self-report, especially at younger ages. As cross-informant discrepancies must be resolved when making a diagnosis, despite often reflecting unique information that each reporter has access to rather than errors, this can lead to low interrater reliability332.
Interrater reliability is consistently higher for neurodevelopmental features and specific symptom dimensions. For example, interrater reliability for diagnostic features of ASD (e.g., reciprocal social interaction, communication, repetitive and restricted behavior) has been found to be higher than for the diagnosis323, 324, 331. ADHD symptom dimensions (inattention and hyperactivity-impulsivity dimensions) similarly show higher interrater reliability than the diagnosis329.
Moreover, estimates of test-retest reliability (a measure of temporal stability) also tend to be higher for dimensional conceptualizations of neurodevelopmental conditions relative to categorical ones. Whereas findings for categorical diagnoses of ASD324, 333 and ADHD334-336 have varied substantially, dimensional studies examining inattention, hyperactivity, and sluggish cognitive tempo features of ADHD333, 337, 338, as well as social, communication, sensory and motor features of ASD339-341, have consistently shown high stability. Overall, there is extensive evidence that spectra/dimensions of neurodevelopmental and other psychiatric features show superior temporal stability compared to diagnostic categories43, 62, 337, 342-344.
The relatively lower reliability found for neurodevelopmental categories compared to dimensions may be due in part to the high co-occurrence between neurodevelopmental diagnoses and their transdiagnostic features (e.g., similarities in symptoms). These issues pose significant challenges to differential diagnosis among the neurodevelopmental conditions345. For example, the interrater reliability for the DSM-IV autism disorder diagnosis – one of five DSM-IV pervasive developmental disorder (PDD) diagnoses – was generally adequate-to-good for the diagnosis of autism versus non-PDD conditions326, 345, but lower for the differential diagnosis of autism versus other PDD326, 345.
Moreover, it is difficult to partition true dimensional and transdiagnostic features into discrete diagnostic categories. For example, clinicians commonly report uncertainty when determining whether individuals with significant social difficulties meet criteria for ASD versus other neurodevelopmental conditions346, and the feature of elevated inattention that is key for ADHD is also commonly seen in children with other neurodevelopmental conditions, as well as other psychiatric conditions97, 347.
Notably, standard diagnostic measures for children and adolescents – e.g., the Diagnostic Interview for Children and Adolescents (DICA)348 – assess ADHD but rarely include other neurodevelopmental conditions, and most adult diagnostic interviews – e.g., the Structured Clinical Interview for DSM-5 (SCID-5)349 – do not include any neurodevelopmental conditions. As such, these conditions are rarely assessed alongside other psychiatric conditions (because doing so would require the addition of another diagnostic assessment and increase burden on researchers/clinicians and patients). This means that the differential diagnosis of neurodevelopmental conditions versus other psychiatric conditions is rarely done in research or clinical contexts, making it difficult to evaluate or differentiate transdiagnostic features (e.g., attention problems due to ADHD or to depression) and contributing to their artificial separation in research and clinical practices32.
Challenges in the reliable assessment of categorical neurodevelopmental diagnoses have important implications. For example, the DSM-5 introduced several changes in the new ASD diagnosis, now encompassing all five DSM-IV PDD diagnoses. This shift has resulted in more severe presentations in individuals receiving a DSM-5 ASD diagnosis compared to those with a DSM-IV diagnosis, but in fewer DSM-5 diagnoses in individuals who had previously met criteria for DSM-IV PDD diagnoses350, 351. At the same time, many individuals who do not meet criteria for a DSM-5 diagnosis nonetheless still show features of ASD350, 351 and other psychiatric conditions30. A shift toward transdiagnostic dimensional assessments that do not rely on strict diagnostic cut-offs would avoid these problems, because dimensional approaches allow for the assessment of key features of neurodevelopmental and other psychiatric conditions, as well as of symptom severity and functional impairment, likely leading to a better identification of treatment targets.
Consistent with recognition of the usefulness of a dimensional approach, there is a long history of dimensional measures for ADHD352-356, such as the Strengths and Weaknesses of ADHD Symptoms and Normal Behavior Scale (SWAN)353, the Adult ADHD Self-Report Scale (ASRS)355, and scales included in the ASEBA system21. There has also been a recent move toward dimensional measures for ASD41, 357, such as the Social Responsiveness Scale (SRS)358, the Autism Symptom Dimensions Questionnaire (ASDQ)359, and the Repetitive Behavior Scale-Revised (RBS-R)360.
These dimensional measures carry multiple advantages, as they are readily adopted in clinical settings (especially when conducting full diagnostic assessments is not feasible or preferred) and show improved interrater reliability and prediction of functioning and impairment relative to categorical ASD and ADHD diagnoses358-362. However, most of these assessment tools are still focused on features of individual conditions, rather than providing a transdiagnostic assessment of all neurodevelopmental conditions, as well as other psychiatric conditions.
Dimensional measures for neurodevelopmental conditions other than ASD and ADHD are also still uncommon, with a few exceptions363, 364. In addition, measurement invariance is rarely considered or explicitly evaluated, but it is important to establish when considering assessments across informants, age, sex/gender, and other sociodemographic and clinical characteristics. Notably, initial work with some standard dimensional measures of ASD indicates a lack of measurement invariance for birth sex that obscures sex-specific patterns of ASD symptoms among boys and girls365.
Overall, it is clear from decades of research that – as for dimensional conceptualizations of internalizing, externalizing and psychotic conditions8, 366 – dimensional measures of neurodevelopmental conditions show higher reliability than categorical indicators7, 41. The development of new transdiagnostic dimensional measures that span across features of all neurodevelopmental and psychiatric conditions and do not rely on strict diagnostic cut-offs will likely further improve reliability. In turn, better reliability of measures can result in more robust research efforts, greater utility in clinical settings, and improved clinical care.
Explanatory and prognostic utility
A critical aspect of the utility of a model or framework is its ability to explain and predict clinical phenomena, risk factors, and outcomes. The heterogeneity intrinsic to neurodevelopmental diagnostic categories has long been regarded as a significant barrier to explanatory and prognostic utility367-371. The transdiagnostic nature of risk factors, cognitive and socio-emotional profiles, and developmental course across neurodevelopmental conditions (as reviewed above) further points to the limited explanatory and prognostic value of categorical diagnoses.
Conversely, a growing body of evidence indicates that a transdiagnostic neurodevelopmental spectrum, or narrower dimensions included within this spectrum (e.g., inattention), can improve explanatory and prognostic utility over a categorical approach, in line with meta-analytic evidence showing greater validity of dimensional conceptualizations relative to categorical ones for a wide range of psychiatric conditions366.
In the Canadian 2006 Participation and Activity Limitation Survey (ages 5-14; weighted N=120,700), a factor capturing neurodevelopmental and related functional characteristics fully mediated the relationship between an ASD diagnosis and child and family health and well-being outcomes (e.g., involvement in school activities, family psychological well-being)372. The direct effects of the neurodevelopmental factor on these outcomes were roughly twice as large as the effects of ASD diagnosis, and these latter effects disappeared when the neurodevelopmental factor was added into the model372, indicating the superior explanatory utility of the dimensional approach.
Longitudinal evidence from three cohorts (total N=1,253) further showed that a model including a neurodevelopmental factor primarily capturing ADHD features, measured in early childhood, predicted pre-adolescent psychiatric psychopathology and psychosocial functioning about two times more strongly than meeting criteria for a DSM diagnosis373.
These findings align with replicated evidence that continuous dimensions of inattention and hyperactivity-impulsivity show greater predictive utility and temporal stability than DSM ADHD inattentive, hyperactive-impulsive, and combined type diagnoses329, 374-377, speaking to the utility of a dimensional approach and the limited validity of categorical diagnostic specifiers.
Several studies also indicate that neurodevelopmental factors show stronger associations with a range of important risk factors and outcomes – including global executive functioning, brain functioning, developmental delays, learning problems, psychosocial functioning, medication use, and service utilization – than general factors comprising other psychiatric conditions and clinical features25, 42, 190, 233, 262, 373, 379. A large Swedish population study (N=1,093,788) showed that a neurodevelopmental factor was associated with reduced fetal growth to a greater extent than internalizing, externalizing, psychosis, and general psychopathology factors45. These associations remained significant even in sibling analyses controlling for unmeasured familial confounding.
A transdiagnostic neurodevelopmental spectrum has also been found to show improved utility over specific neurodevelopmental features. For example, a large longitudinal study on a UK birth cohort (N=10,054) found that a broad childhood neurodevelopmental factor predicted adult mood problems more stably and to a larger extent than more narrow dimensions capturing motor and cognitive difficulties49.
Overall, these findings indicate that a transdiagnostic characterization of neurodevelopmental conditions can better explain and enhance prediction of important outcomes beyond categorical approaches, and provides incremental validity even over dimensional indicators of other psychiatric conditions and clinical features202.
Clinical utility
Clinical utility includes the extent to which shifting toward a transdiagnostic dimensional approach for neurodevelopmental conditions would reflect clinician acceptability and preference; facilitate practical implementation in clinical settings, patient conceptualization, communication among practitioners, patients and family members, clinical decision-making, and treatment selection/planning; and improve outcomes for individuals, families and clinicians379.
Several lines of evidence indicate that transdiagnostic dimensional approaches in general17-19, and to neurodevelopmental conditions more specifically7, 202, 320, 380, provide more clinically useful assessment and treatment targets than diagnostic categories.
Research on practitioner ratings has found that clinicians report a preference for and greater acceptability, feasibility and clinical utility of a transdiagnostic dimensional approach to diagnosis in both child and adult patients, including those with ADHD326. This is consistent with data showing that practitioners focus more on symptom severity than diagnostic categories in clinical decision-making381. Notably, child and adult patients (and parents of child patients) also reported that the transdiagnostic approach was likely to be more helpful to the clinician in understanding their problems and needs326.
Another piece of evidence directly pointing to the clinical utility of a dimensional approach to neurodevelopmental conditions is the widespread implementation of dimensional assessments in clinical settings382, particularly for ADHD353-355, 383, 384, but also more recently for ASD41, 357-360, 385 and intellectual disabilities363, 386. As a singular diagnosis does not provide clinicians with an accurate picture of the individual patient, dimensional assessments are routinely used in clinical care to yield a more complete conceptualization of an individual's strengths, weaknesses and needs beyond their categorical diagnosis7, 382, 387-390.
This is illustrated by a recent field trial on the utility of newly-developed behavioral indicators for assessing the severity of intellectual disabilities, included within the Clinical Descriptions and Diagnostic Requirements for ICD-11 neurodevelopmental disorders363. Findings showed positive practitioner ratings regarding ease of administration, as well as clinical utility for treatment selection, prognostication, and communication with other health care and educational professionals363.
Regarding support and treatment strategies, there is evidence that targeting the social difficulties common across many neurodevelopmental conditions by designing interventions around social skills rather than diagnoses may be more helpful and cost-effective202, 391. Dimensional assessments can also be useful for monitoring treatment efficacy and clinical improvements over time387, 389, 392. Broadening the transdiagnostic focus across both neurodevelopmental and psychiatric conditions is likely to promote the development of preventive strategies to avert the emergence of later-onset mental health challenges in individuals with neurodevelopmental conditions. This is in line with recent proposals for a stepped-care personalized health model for ASD tailored to autistic individuals’ and families’ needs, strengths and challenges390.
Finally, the clinical utility and acceptability of the proposed transdiagnostic dimensional approach are reflected in stakeholders’ clinical priorities. Advocacy organizations and individuals with neurodevelopmental conditions have highlighted the unmet support needs resulting from the use of traditional categorical approaches in clinical settings33, 34, 393. As a solution to these challenges, they have actively called for a shift toward clinical services supporting multiple neurodevelopmental conditions and including dimensional assessments for neurodevelopmental and co-occurring conditions313, 382.
Emerging evaluations of clinical services adopting such an approach in the UK have shown improvements in capacity for support and satisfaction from patients, families and practitioners, along with reductions in waiting lists, re-referrals to different assessments (e.g., for learning difficulties in a child initially assessed in an ADHD clinic), and economic cost383. These encouraging data point to the clinical utility of a transdiagnostic dimensional approach to neurodevelopmental conditions and support the extension of this approach to other counties394.
IMPLICATIONS
Integrating the proposed neurodevelopmental spectrum into transdiagnostic approaches to psychiatric conditions can have several important implications.
Research implications
From a research perspective, our proposal to situate the neurodevelopmental spectrum in transdiagnostic models of psychiatric conditions can provide a formal framework for characterizing the common developmental continuity and co-occurrence among neurodevelopmental conditions and between them and other psychiatric conditions. Progress in this area has been slow, as research based on categorical approaches has typically considered neurodevelopmental conditions separately from one another and from other psychiatric conditions. This is at odds with how these conditions manifest clinically, and has led researchers, advocacy organizations, and people with lived experience to call for more transdiagnostic work across neurodevelopmental conditions and psychiatric comorbidities7, 25, 32-35, 395. The notion of a neurodevelopmental spectrum and its explicit consideration alongside other transdiagnostic spectra/dimensions can directly respond to these issues by promoting a more holistic characterization of their frequent overlap across development.
Moreover, inclusion of the proposed neurodevelopmental spectrum into transdiagnostic models can have important implications for elucidating the etiological and developmental underpinnings of neurodevelopmental and other psychiatric conditions. Categorical approaches have encouraged etiological and developmental research focused on individual conditions, often not considering whether research participants also present with (or have a prior history of) other conditions. As a result, it has not been possible to clarify to what extent the risk factors and mechanisms identified for any individual condition are specific to that condition, shared across multiple conditions, or explained by unmeasured comorbidities9. Incorporating the neurodevelopmental spectrum into transdiagnostic models can allow researchers to pinpoint etiological and developmental processes that are specific to that spectrum (or its constituent subdimensions) and those shared with other transdiagnostic spectra/dimensions. Further, since earlier developmental expressions of neurodevelopmental features often precede more severe presentations and significant impairment145, the proposed transdiagnostic approach can generate new insights into developmental processes more generally, which are key to early identification and prevention.
In addition, by encouraging a broad assessment of the degree of functioning and challenges displayed by each individual, the dimensional approach intrinsic to the proposed transdiagnostic conceptualization can also help consolidate understanding that neurodevelopmental conditions are on a continuum with typical functioning and subthreshold presentations7, 26, just like their common psychiatric comorbidities12, 17-19. A dimensional approach characterizing the entire population-level distribution of multiple neurodevelopmental features will also encourage researchers to move away from the known limitations of case-control studies7, 11, 17. This is especially valuable for conditions with lower diagnostic prevalence rates (e.g., ASD), for which recruitment of eligible individuals into studies is challenging.
Overall, including the proposed neurodevelopmental spectrum in transdiagnostic frameworks can foster approaches to characterize co-occurring profiles, heterogeneity, mechanisms, and developmental processes, as well as promote significant refinement of theoretical and etiological models of neurodevelopmental and other psychiatric features. This can have important effects on stratification, biomarker discovery, and future clinical practices.
Clinical implications
From a clinical perspective, our proposal has implications for early identification, prevention, treatment planning, and transdiagnostic interventions. First, as neurodevelopmental conditions share many overlapping early features, focusing on transdiagnostic domains rather than single measures of separate diagnostic categories can improve early identification and optimize early intervention391. This has direct clinical implications, for example, in addressing issues of diagnostic overshadowing33, 396, such as when receiving a diagnosis of ASD leads to delayed diagnosis of other neurodevelopmental conditions (e.g., ADHD) or other psychiatric conditions (e.g., depression).
Second, a broader assessment of various neurodevelopmental features, alongside features of other psychiatric conditions, can yield a fuller evaluation of an individual's specific strengths, difficulties and needs than possible when focusing on categorical diagnoses. It can also allow for the assessment of gradations in functioning in multiple domains. This can both identify areas of strength, that may be emphasized, and allow for earlier identification of difficulties before they become severe enough to meet the level of a diagnosis. As a result, a transdiagnostic approach can directly address the priorities of individuals with neurodevelopmental conditions and their families, proving more clinically acceptable and less stigmatizing than categorical diagnostic approaches10, 32, 33.
Third, neurodevelopmental conditions increase the risk for other psychiatric conditions in adolescence and adulthood31, 49, 151, 153, 395, but this risk is non-specific across the neurodevelopmental spectrum49, 397. A transdiagnostic approach to assessing the neurodevelopmental spectrum, instead of focusing on individual diagnoses, offers greater explanatory power for predicting important outcomes. Characterizing risk pathways between a broad neurodevelopmental spectrum and subsequent psychiatric conditions can improve prevention and timely diagnostic assessment395.
Finally, the proposed transdiagnostic dimensional approach can increase access to needed services. Clinicians, users and their families, and advocates speak to the need for approaches and services that recognize mental health complexity33, 391, 398, 399, including service delivery based on severity, functioning and prognosis, rather than limiting access to only those who have received a specific diagnosis33, 400, 401. Under the current categorical approach, an individual displaying impairing features of several neurodevelopmental conditions, but not reaching diagnostic cut-offs for any specific diagnosis, can be denied care. Instead, taking a more universal approach to providing services focused on broad neurodevelopmental features can enable prompt recognition and support based on individual needs, helping to address barriers to care, including structural inequities related to immigration, race and ethnicity402-404. Additionally, such an approach may be destigmatizing, since it will encourage moving away from diagnostic labels towards a focus on individual challenges as well as strengths10, 405.
FUTURE DIRECTIONS
An important future step is to map the finer-grained structure of the neurodevelopmental spectrum by investigating its specific subdimensions (e.g., inattention, repetitive behaviors, reading difficulties). This work may build on previous studies on the structure of individual neurodevelopmental conditions. For example, the most replicated structure of ADHD includes separate inattention, hyperactivity and impulsivity factors199, 406, whereas the ASD literature has identified between three (communication, social interaction, and restrictive/repetitive behaviors)407, 408 and five (somewhat varying across studies)199, 409-412 factors.
Studies spanning subdimensions of neurodevelopmental and other transdiagnostic spectra/dimensions can shed light on whether certain neurodevelopmental features may partly overlap with other more established spectra/dimensions. For example, some studies conformant with the HiTOP model suggest that impulsive features of ADHD and aloofness features of ASD may be also partly accounted for, respectively, by disinhibited externalizing25 and detachment53 spectra.
Additionally, features currently included within other spectra/dimensions may be better captured by the new neurodevelopmental spectrum. For example, repetitive thinking and behaviors characterizing OCD (typically included in internalizing factors) may show stronger clustering with neurodevelopmental features25, in line with evidence that they are common also in ASD and Tourette's syndrome and not always associated with obsessions199.
There is also a critical need for prospective longitudinal studies of unselected epidemiological samples first assessed early in life and then repeatedly into childhood, adolescence and adulthood. Although such studies are resource and time intensive, they are the only way to capture the development, temporal ordering, and dynamic course of neurodevelopmental and other psychiatric conditions. Of particular importance for comprehensive etiological models of psychiatric conditions is a better understanding of the stability of the proposed neurodevelopmental spectrum, and the continuity or discontinuity of neurodevelopmental conditions with one another and with other psychiatric conditions captured by other broad spectra/dimensions. Investigations that track features and behaviors of neurodevelopmental and other psychiatric conditions across key developmental periods and the entire lifespan are also needed to examine equifinality and multifinality319.
Including neurodevelopmental features alongside other psychiatric features in transdiagnostic studies is also necessary to further evaluate the validity evidence for the neurodevelopmental spectrum, in line with validators commonly used in psychiatric nosology5, 17-19. The existing research reviewed in this paper identifies commonalities across neurodevelopmental conditions for psychiatric nosology validators. However, because this research rarely includes features of both neurodevelopmental and other psychiatric conditions, it remains unclear whether these validators are specific to the neurodevelopmental spectrum. Future studies should establish associations with validators specific to the neurodevelopmental spectrum or transdiagnostically associated with multiple spectra (particularly concerning environmental risk factors and temperament/personality profiles), as well as associations relevant to specific developmental periods.
Of note, this is also an issue for the validity of other, well-established internalizing, externalizing and psychosis spectra17-19, because that research likewise has rarely included neurodevelopmental conditions, meaning that unexamined co-occurrence with earlier-onset features of neurodevelopmental conditions may account for findings. Therefore, the inclusion of a neurodevelopmental spectrum in transdiagnostic psychiatric frameworks is necessary to evaluate the validity evidence for transdiagnostic spectra more generally.
Studies of this kind will require the development of new and expanded measures that comprehensively cover the range of features and behaviors captured in transdiagnostic frameworks of psychiatric conditions, including neurodevelopmental ones. Although strict cut-offs are antithetical to the transdiagnostic dimensional approach we describe here, incorporating clinically useful thresholds that identify individuals in need of additional supports can improve implementation, conceptualization, communication, treatment selection/planning, and outcomes for individuals, families and clinicians344.
Finally, an important future direction will be to engage multiple stakeholders – including people with lived experience, families, advocates, researchers and clinicians – in broader discussions (e.g., through participatory research approaches) on the acceptability of applying and implementing the proposed transdiagnostic approach to neurodevelopmental and other psychiatric conditions in clinical settings. Translating our proposed transdiagnostic approach into clinical care has the potential to transform how co-occurring mental health problems are detected and supported. Yet, integrating a neurodevelopmental spectrum in transdiagnostic psychiatric frameworks (e.g., HiTOP) may also suggest that features of ASD, ADHD and other neurodevelopmental conditions should be exclusively seen as forms of psychopathology. This issue is non-trivial, as many individuals with neurodevelopmental conditions do not recognize these conditions as pathological, but rather as forms of neurodiversity27-29 or aspects of their own identity (as evidenced by the preference for identity-first language expressed by certain groups)27.
At the same time, the neurodiversity framework encourages research and clinical efforts on issues important to people with neurodevelopmental conditions, with the potential to improve their lives27, 28, 313. As prompt recognition and access to support are top priorities of people with lived experience and advocacy groups worldwide32-35, the benefits arising from our proposed approach could outweigh the potential risks associated with considering a neurodevelopmental spectrum alongside other transdiagnostic psychopathology spectra/dimensions. Moreover, transdiagnostic dimensional approaches promote a view of each person as a whole, with individual challenges and strengths, and are less pathologizing/stigmatizing than categorical approaches10, which are still prevailing in clinical care.
CONCLUSIONS
The evidence discussed in this paper provides a compelling case for the inclusion of the neurodevelopmental spectrum into transdiagnostic frameworks of psychiatric conditions. Research and clinical practices have for too long focused on neurodevelopmental conditions in isolation, ignoring their high rates of co-occurrence with one another and other psychiatric conditions.
Our proposal promotes a shift towards a joint transdiagnostic and dimensional approach to neurodevelopmental and frequently co-occurring problems across development both in research and clinical settings. Future research and implementation work are needed, but our proposed approach can already be used to guide innovative studies and design transdiagnostic assessments and clinical protocols.
This approach can provide more accurate conceptualization, holistic assessment and individualized support for neurodevelopmental features alongside other frequently co-occurring conditions, thereby meeting the needs of each individual.
ACKNOWLEDGEMENTS
The authors thank M. Altschuler and C.G. McDonnell for their input in the early stages of this project, and L. Satchell, M. Bellgrove and J. Tiego for their feedback. They are also grateful to the neurodivergent people and neurodiversity advocates and organizations whose views have shaped this work. G. Michelini is supported by a Klingenstein Third Generation Foundation fellowship (no. 20212999); C.O. Carlisi by a Prudence Trust mid-career fellowship and a Wellcome Trust postdoctoral fellowship (no. 206459/Z/17/Z); R.F. Krueger by the US National Institutes of Health (grants nos. R01AG053217, R01AG077742, U19AG51426); J.J. Li by the E. Kennedy Shriver National Institute of Child Health and Human Development (no. P50HD105353).




