Fecal urgency and incontinence in inflammatory bowel disease perceived by physician and patient: Results from the Swiss fecal urgency survey
Nadia Wespi and Stephan Vavricka share co-first authorship.
Abstract
Introduction
Although increasingly appreciated, little is known about the prevalence of fecal urgency, fecal incontinence and differences between patients' and physicians' perception in inflammatory bowel disease (IBD).
Methods
We performed an online patient and physician survey to evaluate the assessment, prevalence and impact of fecal urgency and incontinence in IBD.
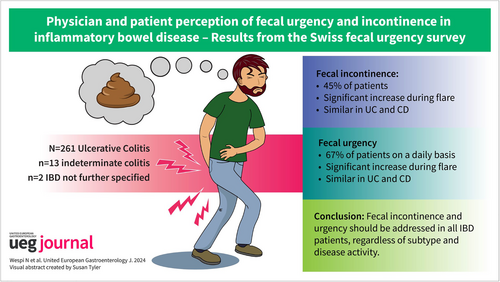
Results
A total of 593 patients (44.0% ulcerative colitis (UC), 53.5% Crohn's disease (CD), 2.2% indeterminate colitis, 2 not specified) completed the survey (65.8% females, mean age 47.1 years). Fecal urgency was often reported (UC: 98.5%, CD: 96.2%) and was prevalent even during remission (UC: 65.9%, CD: 68.5%). Fecal urgency considerably impacted daily activities (visual analog scale [VAS] 5, IQR 3–8). Yet, 22.8% of patients have never discussed fecal urgency with their physicians. Fecal incontinence was experienced by 44.7% of patients and 7.9% on a weekly basis. Diapers/pads were required at least once a month in 20.4% of patients. However, 29.7% of patients never talked with their physician about fecal incontinence. UC was an independent predictor for the presence of moderate-severe fecal urgency (OR 1.65, 95% CI 1.13–2.41) and fecal incontinence (OR 1.77, 95% CI 1.22–2.59). All physicians claimed to regularly inquire about fecal urgency and incontinence. However, the impact of these symptoms on daily activities was overestimated compared with the patient feedback (median VAS 8 vs. 5, p = 0.0113, and 9 vs. 5, p = 0.0187).
Conclusions
Fecal urgency and incontinence are burdensome symptoms in IBD, with a similar prevalence in UC and CD. A mismatch was found between the physician and patient perception. These symptoms should be addressed during outpatient visits.
Graphical Abstract
Key summary
What is already known?
-
Fecal urgency is increasingly recognized as a disturbing symptom in ulcerative colitis (UC) but is still neglected in Crohn's disease.
What are the significant and new findings?
-
We show that fecal urgency and incontinence are frequent (during flares, but also in disease remission) in both UC and Crohn's disease, with a significant impact on daily activities. There is a considerable mismatch between the physician and patient perception as to whether or not these symptoms are discussed during patient encounters.
-
Fecal urgency and incontinence should be addressed and treated in all inflammatory bowel disease patients, regardless of disease subtype and disease activity.
INTRODUCTION
Patients with ulcerative colitis (UC) and Crohn's disease (CD) mainly suffer from abdominal pain, diarrhea, and rectal bleeding.1 In recent years, other symptoms, particularly fecal urgency and incontinence, have been increasingly recognized and reported in both inflammatory bowel disease (IBD) subtypes. Bowel urgency is characterized by a sudden, immediate, and almost non-controllable need to defecate.2 Fecal incontinence is defined as the inability to control the passage of gas or stool through the anus, ranging from occasional soiling of underwear to a complete loss of bowel control.3 The pathophysiology of fecal urgency and incontinence remains elusive,4 but potentially chronic rectal inflammation results in fibrosis, which then decreases compliance of the rectal wall.5, 6
Bowel urgency and fecal incontinence both negatively impact daily activities and quality of life, but these symptoms are still and often considered a taboo topic, even during physician encounters. Patients might feel embarrassed, which potentially results in underreporting.7-11 In fact, as past studies have shown, bowel urgency remains an often-underestimated problem.12, 13 Only very recently, fecal urgency has come to attention in UC clinical trials as a potential and important patient-reported outcome that can be targeted by biological treatments,14 while in CD, it remains a neglected symptom. However, very little is known about the exact (patient-reported and real-world) prevalence of fecal urgency, the presence of fecal incontinence and differences between patients' and physicians' perceptions. Such a mismatch between patient and physician perception is a well-known problem from other aspects of IBD care.15
Given these uncertainties, we aimed to investigate patient-reported real-world prevalence of fecal urgency and incontinence among Swiss IBD patients, their potential impact on daily activities and quality of life, and patient satisfaction with physician encounters. Furthermore, we sought to explore—for the first time - a potential mismatch between patient and physician perspectives about the prevalence and impact of fecal urgency and incontinence.
METHODS
Study design
We performed an online patient and physician survey in the German speaking part of Switzerland to evaluate the assessment, prevalence and impact of fecal urgency and incontinence on overall disease burden. The patient survey was distributed among German-speaking IBD patients through the Swiss patient advocacy group and through IBD specialists. In the second step, a physician survey was distributed among the Swiss gastroenterologists with the highest IBD patient load. The study was exempted from ethical approval by the local ethics committee of the University of Zurich (BASEC No-2022-01336) given the completely anonymous data collection.
Patient recruitment, inclusion and exclusion criteria
An anonymous online survey was distributed among IBD patients with the help of the Swiss patient advocacy group Crohn Colitis Schweiz (CCS) and Swiss IBD specialists. CCS sent a survey link through their regular member information, while IBD specialists were encouraged to inform their patients and—if they were interested—to send them the respective survey link. All survey participants who completed the online survey were included. If the survey was not completed, participants were excluded from the analysis. For the physician survey, a link was sent to the gastroenterologists that were most mentioned as treating physicians by the surveyed IBD patients and all specialists who completed the survey were included for analysis.
Patient survey
A survey was generated using the commercially available online tool limesurvey (https://www.limesurvey.org/de). The survey was developed in a two-step approach: a first draft was set up by two IBD experts (NW and SV) after a literature review (with the main focus of the survey being frequency and impact of fecal urgency and incontinence). This first version was then discussed with the co-authors and refined according to their feedback. The online patient questionnaire consisted of a total of 40 questions, with 17 questions focusing on fecal urgency, 8 on fecal incontinence, 10 on general information and IBD symptoms and 5 on past and current therapies. All questions were in German. The survey was open from 15 January 2023 to 9 September 2023. The final version (in German) can be found in the online supplements (Supporting Information S2) with the key questions regarding fecal urgency and incontinence translated in English (Table S3).
Physician survey
In analogy to the patient survey, a physician survey was generated using limesurvey (https://www.limesurvey.org/de), with the initial draft by two experts being revised after feedback from the co-authors. The online physician questionnaire consisted of a total of 28 questions, with 12 questions focusing on fecal urgency, 5 on fecal incontinence, 10 on general information and IBD symptoms and 1 on past and current therapies. All questions were in German. The survey was active from September 12 2023 to November 16 2023. The final version (in German) can be found in the online supplements (Supporting Information S3).
Outcomes and definitions
The primary outcome of the study was the prevalence of IBD patients reporting fecal urgency and fecal incontinence. Secondary outcomes were the impact of fecal urgency and fecal incontinence on disease burden and quality of life, patient perception of physicians' interest in these symptoms, and their respective satisfaction with the physician encounter. For grading symptom severity, a visual analog scale (VAS) ranging from 0 (absence of symptoms) to 10 (most severe symptoms) was used. For assessment of contribution to disease burden, a VAS ranging from 0 (no contribution) to 100 (100% contribution) was used. The following definitions were used in our study: (1) fecal urgency was defined as a sudden, immediate, and almost non-controllable need to defecate2; and (2) fecal incontinence was defined as the inability to control the passage of gas, mucus, or stool through the anus.3 Moderate to severe fecal urgency and incontinence was defined as VAS >5 on a scale from 0 to 10 (0 indicating no symptoms, and 10 indicating most severe symptoms). Disease remission was defined clinically by the absence of flare symptoms (based on patient interpretation).
Statistical analyses
For statistical analyses, the statistical package program STATA (version 16, College Station) and GraphPad Prism software (version 8.3.0) were used. Categorical data are depicted as percentage of the group total. Metric data are presented as means with standard deviation and total range or median with interquartile range. Comparison between categorical data was performed by using Chi-square test or Fisher's exact test, if the sample size was less than 10. For comparisons between continuous variables, the two-sample t-test and Wilcoxon rank-sum test were used depending on whether data were normally distributed or not. For paired data, either the paired t-test or the Wilcoxon signed-rank test was used. For the purpose of this study, a p-value of <0.05 was considered statistically significant.
RESULTS
Patient and disease characteristics
Between January 15 and 9 September, 2023, a total of 738 patients participated in the online survey. Assuming a link to the survey being sent to 2600 members of the patient advocacy group, the response rate was 28.4%. After 145 patients were excluded for not having finished the survey, a total of 593 patients (65.8% females) were included for analysis (corresponding to a final response rate of 22.8%). Of those patients, 261 suffered from UC (44.0%), 317 from CD (53.5%), and 13 from indeterminate colitis (2.2%). Two patients were diagnosed with IBD without specifying their underlying subtype. The mean age of the adult patients was 47.1 years (SD 14.6 years, range 19–86), 15 patients (2.5%) were adolescents (14–18 years). Almost all of the patients (583, 98.3%) were Swiss residents, with the largest proportion living in the region of Zurich (176, 29.7%). Of the surveyed patients, 299 (50.4%) were biologic-experienced, while 80 (13.5%) were not on any IBD-specific treatment at all. A total of 179 (30.2%) of the patients had undergone intestinal (IBD-related) surgery in the past. Vaginal delivery (at least one) was reported in 140 females (35.9% of all women). For patient and disease characteristics, see Table 1.
| Characteristics | Total | UC | CD |
|---|---|---|---|
| N = 593 | N = 261 | N = 317 | |
| Patient and disease characteristics | |||
| Age in years of adult patients (mean, range) | 47.1 (19–86) | 45.4 (19–81) | 48.5 (19–86) |
| Adolescent patients (age 14–18) | 15 (2.5%) | 7 (2.7%) | 7 (2.2%) |
| Female sex | 390 (65.8%) | 170 (65.1%) | 208 (65.6%) |
| IBD subtype | |||
| Ulcerative colitis | 261 (44.0%) | 261 (100%) | – |
| Crohn's disease | 317 (53.5%) | – | 317 (100%) |
| Indeterminate colitis | 13 (2.2%) | – | – |
| Not specified | 2 (0.3%) | – | – |
| Treatments | |||
| Oral 5-ASA | 155 (26.1%) | 125 (47.9%) | 23 (7.3%) |
| Rectal 5-ASA | 66 (11.1%) | 63 (24.1%) | 1 (0.3%) |
| Oral topical steroids | 29 (4.9%) | 11 (4.2%) | 17 (5.4%) |
| Rectal steroids | 22 (3.7%) | 15 (5.7%) | 7 (2.2%) |
| Systemic steroids | 46 (7.8%) | 22 (8.4%) | 22 (6.9%) |
| Conventional immunosuppression | 66 (11.1%) | 30 (11.5%) | 35 (11.0%) |
| Biologics | 299 (50.4%) | 100 (38.3%) | 194 (61.2%) |
| JAK-inhibitors | 9 (1.5%) | 7 (2.7%) | 1 (0.3%) |
| S1P | 2 (0.3%) | 1 (0.4%) | 0 (0.0%) |
| No treatment | 80 (13.5%) | 23 (8.8%) | 54 (17.0%) |
| Previous IBD-related surgery | 179 (30.2%) | 28 (10.7%) | 148 (46.7%) |
| History of vaginal delivery (% of all females) | 140 (35.9%) | 62 (36.5%) | 73 (35.1%) |
| Fecal urgency and incontinence | |||
| Frequency of fecal urgency (without flare) | |||
| Less often than daily | 159 (26.8%) | 71 (27.2%) | 83 (26.2%) |
| At least daily | 397 (66.9%) | 172 (65.9%) | 217 (68.5%) |
| No fecal urgency | 37 (6.2%) | 18 (6.9%) | 17 (5.4%) |
| Frequency of fecal urgency (with flare) | |||
| Less often than daily | 23 (3.9%) | 4 (1.5%) | 19 (6.0%) |
| At least daily | 550 (92.7%) | 251 (96.2%) | 285 (89.9%) |
| No fecal urgency | 20 (3.4%) | 6 (2.3%) | 13 (4.1%) |
| Frequency of fecal incontinence (during the last 6 months) | |||
| Present, but less than once a week | 218 (36.8%) | 93 (35.6) | 120 (37.9%) |
| On a weekly basis | 47 (7.9%) | 26 (10.0%) | 19 (6.0%) |
| No fecal incontinence | 328 (55.3%) | 142 (54.4%) | 178 (56.2%) |
| Wearing pads or diapers | |||
| Less than once per month | 36 (6.1%) | 21 (8.0%) | 15 (4.7%) |
| On a monthly basis | 121 (20.4%) | 57 (21.8%) | 59 (18.6%) |
| Not required | 436 (73.5%) | 183 (70.1%) | 243 (76.7%) |
- Note: Percentage refers to the total number of patients in each column (second column n = 593, third column n = 261 and fourth column n = 317).
- Abbreviation: CD, Crohn's disease.
Fecal urgency
An increase in fecal urgency during a disease flare was experienced by 82.1% of patients, 15% suffered from fecal urgency regardless of disease activity, and only 2.9% never experienced this symptom. The number of morning stools and severity of fecal urgency (VAS 0–10) significantly increased during a flare (median number of stools 3 vs. 1, and median VAS 8 vs. 4, p < 0.0001). Fecal urgency at least on a daily basis (in a period without a flare) was seen in 66.9% of patients, while this proportion increased to 92.7% during a flare (p < 0.001). See Figure 1a. In a period without a flare, 48.7% patients did not tolerate fecal urgency more than 5 min, while this proportion increased to 85.2% during a flare (p < 0.001). Fecal urgency considerably impacted daily activities (VAS 5, IQR 3–8), and contributed to 60% of the self-estimated disease burden (IQR 40%–80%). However, 22.8% of patients had never talked about fecal urgency, but only 11.8% thought their physician underestimated the problem. Women did not report fecal urgency more often than males, but they were more severely affected (VAS 6 vs. 5, p = 0.0025).
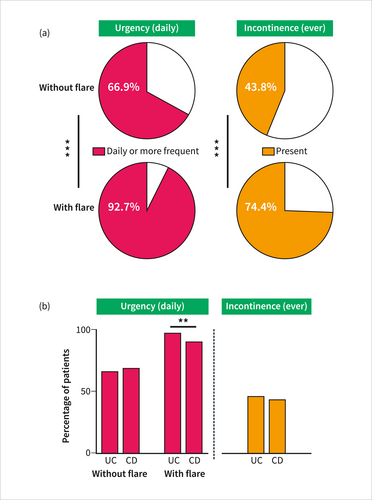
(a) Frequency of fecal urgency (in remission and during flare) and fecal incontinence (ever, in remission and during flare), in percentage of all patients; (b) Frequency of fecal urgency (in remission and during flare) and incontinence (ever in the last 6 months) stratified by IBD subtype (UC vs. CD), in percentage. **p < 0.01, ***p < 0.001. CD, Crohn's disease; IBD, inflammatory bowel disease; UC, ulcerative colitis.
UC and CD patients appeared to be similarly affected by fecal urgency. Almost all UC (98.5%) and CD (96.2%) patients experienced fecal urgency either during a flare or regardless of underlying disease activity. Fecal urgency at least on a daily basis was experienced by 65.9% of UC and 68.5% of CD patients (in a period without a flare). While this proportion increased during disease flares for both IBD subtypes, significantly more UC patients (96.2 vs. 89.9%, p = 0.004) suffered from fecal urgency during a flare. See Figure 1b. A similar proportion of patients did not tolerate fecal urgency more than 5 min (UC 45.2%, CD 52.4%) in a period without a flare, with a significant increase during a flare. However—again—during such a flare, significantly more UC patients experienced severe fecal urgency without tolerance of more than 5 min (88.9 vs. 81.7%, p = 0.016), compared to CD patients. The self-assessed severity of fecal urgency (VAS) during periods without a flare was higher in CD patients (VAS 4, IQR 2–6) than in UC patients (VAS 3, IQR 1–5, p < 0.001), while during flares, severity was higher in UC patients (VAS 9, IQR 8–10) compared to CD (VAS 8, IQR 7–9, p = 0.002). The impact on daily activity was considerable in both UC (VAS 6, IQR 3–8) and CD (VAS 5, IQR 3–8). See Figure 2a. Nevertheless, the contribution to disease burden was estimated to be higher in UC than CD (60 vs. 50%, p = 0.0275). A considerable proportion of both UC (19.9%) and CD patients (24.9%) had never talked to their physicians about fecal urgency, but only a small proportion of UC (13.4%) and CD (10.4%) patients thought that their physician underestimates the problem of fecal urgency, To disentangle the association of IBD subtype with severity of fecal urgency, we performed a multivariate logistic regression model with the following co-variates: history of vaginal delivery, sex, age, presence of severe disease (defined by treatment with biologics or a small-molecule), IBD subtype, history of previous intestinal surgery. Presence of moderate to severe fecal urgency defined by VAS >5 (on a scale from 0 to 10) was the dependent variable. In this model—after adjusting for the abovementioned covariates—UC was significantly associated with moderate to severe fecal urgency (OR 1.65, 95% CI 1.13–2.41, p = 0.010), as it was seen for previous intestinal surgery (OR 2.07, 95% CI 1.36–3.18, p < 0.001). For details, see Table S1.
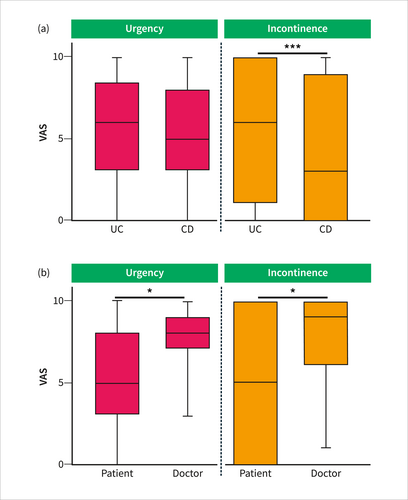
(a) Impact fecal urgency and fecal incontinence on daily activities, based on a VAS 0–10, stratified by IBD subtype; (b) Mismatch between patient and physician perception of impact (VAS 0–10) of fecal urgency and fecal incontinence. *p < 0.05, ***p < 0.001. IBD, inflammatory bowel disease; VAS, visual analog scale.
Fecal incontinence
Experience of fecal incontinence (ever in the last 6 months, with a frequency of either more than once a week, once a month to once a week or less often than once a month) was reported by 44.7% of patients (Figure 1a) and 7.9% on a weekly basis. When asked about details of incontinence (ever, also beyond 6 months), most patients reported uncontrolled passage of liquid stool (72.5%), while incontinence for gas was seen in only 14.5%. During a flare, fecal incontinence (either noticed or unnoticed) was significantly more frequent than during disease remission (74.4 vs. 43.8%, p < 0.001). Diapers/pads were required at least once per month by 20.4% of patients. Fecal incontinence considerably impacted daily activities (median VAS 5), with—however—a large variation (IQR 0–10). Still, 29.7% of patients never talked to their physician about fecal incontinence (7.9% would like to talk more). Of note, no difference with regard to the prevalence and severity of fecal incontinence was found between males and females.
Both UC and CD patients similarly experienced fecal incontinence (45.6% and 43.8%) and required diapers/pads on a monthly basis (21.8% and 18.6%). See Figure 1b. However, the impact of fecal incontinence on daily activities was significantly higher in UC (VAS 6, IQR 1–10) than CD (VAS 3, IQR 0–9, p = 0.0007). See Figure 2a. A considerable proportion of both UC and CD patients did not talk to their physicians about fecal incontinence (26.1% and 32.2%).
To disentangle the association of IBD subtype with severity of fecal incontinence, we performed a multivariate logistic regression model with the following co-variates: history of vaginal delivery, sex, age, presence of severe disease (defined by treatment with biologics or a small-molecule), IBD subtype, and history of previous intestinal surgery. The presence of moderate to severe fecal incontinence defined by VAS >5 (on a scale from 0 to 10) was the dependent variable. In this model—after adjusting for above mentioned co-variates—UC was significantly associated with moderate to severe fecal incontinence (OR 1.77, 95% CI 1.22–2.59, p = 0.003), as it was seen for history of vaginal delivery (OR 1.61, 95% CI 1.02–2.53, p = 0.04), history of previous intestinal surgery (OR 1.76, 95% CI 1.17–2.65, p = 0.007), and older age (OR 1.01, 95% CI 1.00–1.02, p = 0.04). For details, see Table S2.
Physician survey
Between September 12 and 16 November, 2023, 15 gastroenterologists completed the physician survey (the survey link was sent to 16 physicians, response rate 93.8%). These gastroenterologists have been practicing for a median of 14 years and most of them (80%) have been treating at least 100–500 IBD patients per year. All physicians (100%) claimed to regularly inquire about fecal urgency and incontinence during patient consultations. Fecal urgency and incontinence were both rated as IBD symptoms with a high impact, but this impact was overestimated compared to the patient feedback (median VAS 8 vs. 5, p = 0.0113, and 9 vs. 5, p = 0.0187). Similarly, the number of morning stools was overestimated during both remission (2 vs. 1, p = 0.0045) and flares (4 vs. 3, p = 0.0015). For details, see Figure 2b.
DISCUSSION
In this online patient and physician survey, we analyzed the prevalence and impact of fecal urgency and incontinence, and a potential mismatch between patient and physician perception. Our main findings are: (1) Fecal urgency and incontinence are frequent and represent two burdensome symptoms in IBD patients. (2) Prevalence of urgency and incontinence is comparable between UC and CD patients. (3) However, UC is an independent predictor for the presence of moderate to severe fecal urgency and fecal incontinence. And (4) a considerable mismatch was found between the physician and patient perception as to whether or not fecal urgency and incontinence are discussed during patient encounters.
Fecal urgency and incontinence are frequently reported by IBD patients and their impact on quality of life and contribution to disease burden is considerable. We found that 97% of IBD patients at least once (ever) experienced fecal urgency, while almost 50% suffered from various degrees of fecal incontinence. These numbers are even higher than previously reported, where prevalence of fecal urgency was estimated at between 60% and 83%,16, 17 and the pooled prevalence of fecal incontinence was 37%,8 although the need for diapers/pads and protection was considerably higher in the CONFIDE UC patient survey, which used a similar definition for fecal incontinence (45% of patients with diapers/pads at least once a week).18 High rates of fecal incontinence in our study could be attributed to the chosen definition with inclusion of uncontrolled passage of gas (not only stool), and the absence of a symptom duration as a prerequisite (such as a 3 months period in the ROME IV criteria).19 Prevalence of fecal urgency appears to be particularly high during disease flares, which goes in line with previous findings from Kulyk et al. and Wang et al. showing that presence of urgency is associated with disease activity.20, 21 Importantly and surprisingly, prevalence of both fecal urgency and fecal incontinence was comparable in UC and CD patients. Thus, although underappreciated,12 fecal urgency and incontinence are not only a problem in UC but also in IBD in general. Overrepresentation of colonic CD could have potentially confounded these results, but data on disease location are missing. In contrast to IBD, fecal urgency appears to be a negligible problem in otherwise healthy individuals.22 Additionally, both symptoms have a considerable impact on daily activities and considerably contribute to the self-estimated disease burden in CD and UC. This goes in line with previous findings showing that sudden need for bowel movement or incontinence impacts health-related quality of life by making the patients feel embarrassed, affecting relationships, or having an impact on work.7 Nevertheless—although frequent in both IBD subtypes—UC is associated with a more severe presentation of fecal urgency and incontinence, as shown by a multivariate regression model. Assessment of fecal urgency appears to be also important from a follow-up perspective as a recent study has demonstrated that patients showing improvement of fecal urgency achieve other outcome parameters more likely.23
IBD specialists acknowledge the importance of fecal urgency and fecal incontinence. However, they appear to overestimate the problem when compared with their patients. Indeed, this difference between patient and physician ratings was significant and also clinically meaningful. This somehow contradicts previous findings where Rubin and colleagues showed that physicians tend to underestimate fecal urgency, particularly in CD.12 Here, a possible selection bias has to be taken into account, as providers interviewed in our survey were from academic centers that manage highly complex IBD cases. In addition, recent approval of Mirikizumab by the Swiss Medical Agency (Swissmedic) might have sharpened gastroenterologists' perspective on fecal urgency and incontinence in the past, as both were clinical outcomes in the respective approval studies.14 Thus, our findings cannot be extrapolated to gastroenterologists in private practice with a smaller IBD patient volume or physicians from other disciplines (e.g. general practitioner).
Importantly, a considerable mismatch was seen when comparing patient and physician perceptions of patient encounters in outpatient clinics. Almost a quarter of patients have never discussed fecal urgency with their physician. Similarly, 30% of patients never talked about fecal incontinence, and 8% would like to talk more. In contrast, all interviewed gastroenterologists stated to regularly inquire about both symptoms at outpatient visits. Such a mismatch between patient and physician perceptions and views has been frequently reported in the medical literature in general, but also for the IBD field in particular. In IBD, this mismatch is especially seen when investigating psychological aspects.15 In our study, however, we reveal for the first time that while physicians think they inquire about symptoms, patients do not perceive it. The European federation of Crohn's and ulcerative colitis associations has recently shown that half of physicians in Europe do not inquire their IBD patients about their quality of life and nearly half of patients do not initiate such a conversation with their physicians.24 Possible explanations are fear of surgery, lack of trust, low self-esteem, and physicians considered too busy or having lack of interest.10, 25 Possible communication barriers are the (over)use of medical jargon, language barriers or underuse of direct questions. Taken together, our and previous findings highlight the need for improvement of communication skills in IBD care.
Our study has several limitations: Due to language restrictions, our results are limited to the German-speaking part of Switzerland. Moreover, due to the nature of the survey, it was not possible to account for confounding factors such as disease course, disease location and score-based disease severity. It could be speculated that patients with more severe symptoms were more likely to participate in the survey. Thus, our findings cannot be extrapolated 1:1 to the general IBD population. In addition, both surveys (patient and physician questionnaires) were newly developed for the purpose of this study and therefore do not represent standardized or validated instruments. This strategy was chosen to keep the surveys as simple as possible. However, the absence of validated instruments such as the urgency numerical rating scale or fecal incontinence quality of life could have impacted robustness and generalizability of our results.14, 26 The patient questionnaire did not ask for the presence of irritable bowel syndrome (IBS) as a comorbidity; thus, we cannot exclude that concomitant IBS contributed to the presence of fecal urgency or incontinence. In fact, 39% of IBD patients are known to suffer from IBS symptoms,27 although fecal incontinence might be less frequent in IBS than in IBD.28 The survey is—as it is known for surveys in general—subject to a so-called recall bias. Thus, the importance of fecal urgency and incontinence might have been overestimated. Although it was asked for repetitive episodes, it cannot be ruled out that some patients with a single episode of fecal incontinence stated to suffer from fecal incontinence with a frequency of less than once per month. However, on the other hand, the presence of fecal incontinence might also have been missed in some patients since we did not ask for coping strategies (such as staying at home in close proximity to a toilet). Finally, the physicians included in the physician survey were all highly experienced IBD experts; thus, our findings cannot be extrapolated to the general practicing gastroenterologist.
In conclusion, fecal urgency and incontinence are burdensome symptoms in IBD, with a similar prevalence in UC and CD. Treating physicians are aware of and might even overestimate the problem. However, a considerable mismatch was found between the physician and patient perception as to whether or not fecal urgency and incontinence are discussed during patient encounters. In order to align patient needs and physician perspective, open questions in a trustable atmosphere—particularly for taboo symptoms—appear to be key for both UC and CD. Patient-centered studies properly assessing their needs and potential gaps in clinical care are needed.
AUTHOR CONTRIBUTIONS
Study concept and design: Nadia Wespi, Stephan Vavricka and Thomas Greuter; acquisition of data: Nadia Wespi, Stephan Vavricka and Thomas Greuter; analysis data: Nadia Wespi, Stephan Vavricka and Thomas Greuter; interpretation of data: Nadia Wespi, Stephan Vavricka, Stephan Brand, Patrick Aepli, Emanuel Burri, Benjamin Misselwitz, Frank Seibold, Petr Hruz, Laurent Peyrin-Biroulet, Alain Schoepfer, Luc Biedermann, Christiane Sokollik, Gerhard Rogler and Thomas Greuter. drafting of manuscript: Nadia Wespi and Thomas Greuter; critical revision of the manuscript for important intellectual content: Stephan Vavricka, Stephan Brand, Patrick Aepli, Emanuel Burri, Benjamin Misselwitz, Frank Seibold, Petr Hruz, Laurent Peyrin-Biroulet, Alain Schoepfer, Luc Biedermann, Christiane Sokollik, Gerhard Rogler; supervision: Stephan Vavricka and Thomas Greuter.
ACKNOWLEDGMENTS
We would like to thank all participants for their valuable contributions and the patient organization CCS for their organizational support. This study was supported by a grant from the Swiss National Science Foundation to TG (grant no. P2ZHP3_168561). This work was further supported by a young investigator award from the Swiss Society of Gastroenterology to TG, a research grant from the Novartis Foundation for Medical-Biological Research to TG, and a research award from the Swiss IBDnet to TG.
CONFLICT OF INTEREST STATEMENT
SV has received consulting fees and unrestricted research grants from Abbott, Falk Pharma GmbH, Ferring Pharmaceuticals, Janssen, MSD, Pfizer Inc, Sanofi-Aventis, Takeda, Tillotts, UCB, and Vifor. SB declares the following conflicts of interests: SB received speaker's honoraria from Abbvie, Falk Foundation, Ferring, Janssen, MSD, Takeda, UCB, and Vifor and participated in advisory boards of Abbvie, BMS, Celgene, Janssen, MSD, Pfizer, Pierre Fabre, Roche, Takeda, and UCB. SB has received an educational grant from Takeda. PA has received consulting and speaker's fees from Boston Scientific, honoraria for advisory boards from Janssen and travel grants from Abbvie. EB has received consultant and/or speaker's fees from Abbvie, Allergan, Amgen, Buehlmann Laboratories, Boston Scientific, Bristol Myers Squibb, Dr. Falk Pharma, Ewopharma AG, Ferring, Janssen-Cilag, MSD, Norgine, Pfizer, Pierre Fabre, Sandoz, Takeda, Tillots, and Vifor. BM reports traveling fees from Takeda, Vifor, Gilead and MSD. BM received fees as a speaker from Takeda. BM has served at an advisory board for Gilead, Takeda and BMS. BM has received research grants from MSD and BMS unrelated to the submitted work. FS is medical adviser for Abbvie, BMS, Eli Lilly, Dr Falk, MSD, Janssen, Takeda. PH has received consulting fees from Abbvie, Bristol Myers Squibb, Falk Pharma GmbH, Janssen, iQone, Lilly, MSD, Pfizer Inc, Sanofi-Aventis, Takeda, and Vifor. LPB reports the following conflicts of interest: Consulting fees from Abbvie, Abivax, Adacyte, Alimentiv, Amgen, Applied Molecular Transport, Arena, Banook, Biogen, BMS, Celltrion, Connect Biopharm, Cytoki Pharma, Enthera, Ferring, Fresenius Kabi, Galapagos, Genentech, Gilead, Gossamer Bio, GSK, IAC Image Analysis, Index Pharmaceuticals, Inotrem, Janssen, Lilly, Medac, Mopac, Morphic, MSD, Nordic Pharma, Novartis, Oncodesign Precision Medicine, ONO Pharma, OSE Immunotherapeuthics, Pandion Therapeuthics, Par' Immune, Pfizer, Prometheus, Protagonist, Roche, Samsung, Sandoz, Sanofi, Satisfay, Takeda, Telavant, Theravance, Thermo Fischer, Tigenix, Tillots, Viatris, Vectivbio, Ventyx, Ysopia; Research grants from Celltrion, Fresenius Kabi, Medac, MSD, Takeda; Speaker's honoraria from. Abbvie, Amgen, Arena, Biogen, Celltrion, Ferring, Galapagos, Genentech, Gilead, Janssen, Lilly, Medac, MSD, Nordic Pharma, Pfizer, Sandoz, Takeda, Tillots, Viatris; and travel grants from Abbvie, Amgen, Celltrion, Connect Biopharm, Ferring, Galapagos, Genentech, Gilead, Gossamer Bio, Janssen, Lilly, Medac, Morphic, MSD, Pfizer, Sandoz, Takeda, Thermo Fischer, Tillots. AS has received consulting fees and unrestricted research grants from Abbvie, Dr Falk Pharma, Ferring Pharmaceuticals, Janssen, MSD, Pfizer, Sanofi-Aventis, Takeda, Tillotts, UCB, and Vifor. LB has received fees for consulting/advisory board from Abbvie, Amgen, Bristol Myers Squibb, MSD, Vifor, Dr. Falk Pharma, Esocap, Janssen, Lilly, Calypso, Ferring, Pfizer, Takeda, Janssen, Sanofi. GR has consulted to Abbvie, Arena, Augurix, BMS, Boehringer, Calypso, Celgene, FALK, Ferring, Fisher, Genentech, Gilead, Janssen, Lilly, MSD, Novartis, Pfizer, Phadia, Roche, UCB, Takeda, Tillots, Vifor, Vital Solutions and Zeller; GR has received speaker's honoraria from Abbvie, Astra Zeneca, BMS, Celgene, FALK, Janssen, MSD, Pfizer, Phadia, Takeda, Tillots, UCB, Vifor and Zeller; GR has received educational grants and research grants from Abbvie, Ardeypharm, Augurix, Calypso, FALK, Flamentera, MSD, Lilly, Novartis, Pfizer, Roche, Takeda, Tillots, UCB and Zeller. GR is cofounder and head of the scientific advisory board of PharmaBiome. TG has consulting contracts with Sanofi-Regeneron, Bristol-Myers Squibb, Takeda, Abbvie, Janssen, Lilly, Pfizer, and Dr. Falk Pharma GmbH, received travel grants from Dr. Falk Pharma GmbH and Vifor, speaker's fee from Norgine and Amgen, and an unrestricted research grant from Novartis. The other authors have no conflicts of interest to declare. No company representative was involved in the conception, writing, or financing of this study.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.