Intrahepatic splenosis mimicking hepatocellular carcinoma
Martina Rosi and Valentina Adotti contributed equally.
A 50 years-old male outpatient was evaluated for the detection of a hepatic nodule during workup for chronic ALT elevation. The patient had undergone splenectomy for abdominal trauma when he was 14 years old and had evidence of metabolic and alcoholic steatotic liver disease.1 MRI showed marked hepatic fatty infiltration and a mass in the 3rd segment. The nodule was hypointense in T1, isointense in T2, and hyperintense in T2-weighted imaging with fat suppression, and showed restriction in diffusion-weighted sequences. The aspect after the administration of gadoxetic acid is shown in Figure 1a–c.
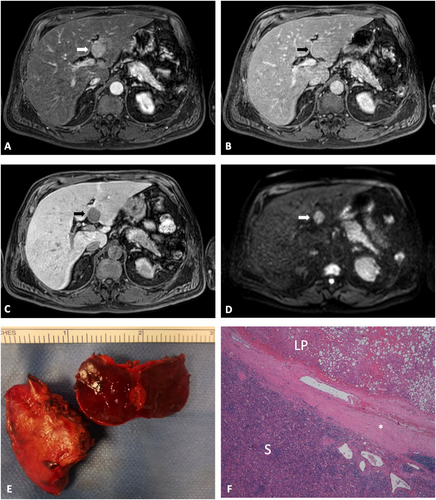
MRI of intrahepatic splenosis (arrow) showing arterial enhancement (a), isointensity in the portal phase (b), hypointensity in the hepatobiliary phase (c) and restriction in diffusion-weighted sequences (d). Macroscopic aspect of resected nodule (e). Histopathology (f) showing steatotic liver parenchyma (LP) separated by a fibrous capsula (*) from the highly vascularized lymphoid tissue with follicular areas (S). Original magnification 4x.
The MRI characteristics were highly suspicious for hepatocellular carcinoma,2 but imaging was not sufficient to make a diagnosis because features of cirrhosis were lacking.3 The patient underwent US-guided liver biopsy on two occasions, with similar reports (presence of necrotic cells and lymphocytes). In consideration of the high risk of malignancy, the patient underwent resection of the hepatic third segment. With the postoperative pathology report (Figure 1e–f), a diagnosis of intrahepatic splenosis was made. This case underscores the essential role of a liver biopsy for the definition of focal lesions in a non-cirrhotic liver.3 In case of inconclusive biopsy, resection is advised, as outlined in a recent review4.
ACKNOWLEDGMENTS
This study did not receive specific funding. We gratefully acknowledge the help of drs. Lavinia Pugliese and Luca Tirloni for providing pathological pictures.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare.
INFORMED CONSENT
Written informed consent has been obtained from the patient. This is held by the corresponding Author together with the Patient's medical record, and is available upon request.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.




