The roles of sex hormones in the pathophysiology of age-related sarcopenia and frailty
Abstract
Background
Sarcopenia is an age-related condition characterized by a progressive and systemic decline in skeletal muscle mass, quality, and strength. The incidence of sarcopenia contains sex-specific aspects, indicating the contribution of sex hormones to its pathophysiology. This review focuses on changing trends in sarcopenia, discusses alterations in definitions and diagnostic criteria, and emphasizes the association between sarcopenia and sex hormones.
Methods
A literature search was performed on PubMed for related articles published between 1997 and December 2023 using appropriate keywords.
Main Findings (Results)
Advances in research have emphasized the significance of muscle quality and strength over muscle mass, resulting in new diagnostic criteria for sarcopenia. Androgens demonstrated anabolic effects on skeletal muscles and played a significant role in the pathophysiology of sarcopenia. In clinical settings, androgen replacement therapy has exhibited certain positive outcomes for treating sarcopenia, despite concerns about potential side effects. Conversely, estrogen is involved in skeletal muscle maintenance, but the detailed mechanisms remain unclear. Moreover, results regarding the clinical application of estrogen replacement therapy for treating sarcopenia remained inconsistent.
Conclusion
The elucidation of molecular mechanisms that involve sex hormones is eagerly awaited for novel therapeutic interventions for sarcopenia.
1 INTRODUCTION
Maintaining the musculoskeletal system is crucial for older adults to lead independent lives. Sarcopenia and frailty are related concepts that frequently coexist in older adults. Sarcopenia is a progressive skeletal muscle disease characterized by low muscle strength, quantity, or quality, as well as diminished physical performance.1, 2 Sarcopenia progression causes reduced mobility, increased risk of falls and fractures, physical disability, and frailty.3 With the global aging population, the number of individuals with sarcopenia is expected to increase. Therefore, addressing the prevention and treatment of sarcopenia and frailty has become an urgent global concern.
The decline in serum androgen levels in males due to late-onset hypogonadism (LOH syndrome) is intricately related to frailty. Conversely, the onset of frailty in females is closely associated with a decrease in serum estrogen levels during menopause. Herein, we provide an overview of trends in sarcopenia, discuss changes in definitions and diagnostic criteria, and particularly focus on its association with sex hormones.
2 UPDATE ON THE DIAGNOSIS OF SARCOPENIA
2.1 Conventional definition and diagnostic algorithm (European Working Group on Sarcopenia in Older People [EWGSOP] and Asian Working Group for Sarcopenia [AWGS] 2014)
Skeletal muscle mass decreases and muscle strength and physical function decline with aging. In 1988, Irwin Rosenberg proposed the term “sarcopenia,” which comes from the conjunction of the Greek words “sarx” (flesh) + “penia” (loss), and defined it as “a syndrome characterized by progressive and generalized loss of skeletal muscle mass and strength with a risk of adverse outcomes such as physical disability, poor quality of life, and death.”1, 4 In 2016, sarcopenia was assigned an International Classification of Diseases, 10th Revision code (M62.84), internationally recognized as a muscle disease, and has now become an essential perspective in all medical and caregiving professionals.5
Diagnostic criteria for sarcopenia have evolved with advancements in research and understanding. In particular, the EWGSOP, the AWGS, and the International Working Group for Sarcopenia (IWGS) played a leading role in the discourse on diagnostic criteria and the consensus on sarcopenia.1-3, 6, 7 In 2010, EWGSOP indicated the criteria for age-related sarcopenia, which recommended the use of (i) low muscle mass + (ii) low muscle function (either low strength and/or low physical performance) for screening community-dwelling people aged ≥65 years.1 These criteria recommend subsequent measurement of muscle mass if an individual shows low grip strength and/or reduced gait speed. The individual is diagnosed with sarcopenia if the muscle mass is decreased. In 2014, the AWGS proposed diagnostic criteria and cut-off values for Asian populations aged ≥60 years, considering race-specific factors such as body size, diet, and physical activity.6 Furthermore, these criteria used grip strength, gait speed, and skeletal muscle mass for diagnosing sarcopenia, where a decrease in muscle mass was essential. The IWGS outlined a similar definition and provided a compilation of the causes categorized by age groups and prevalence of sarcopenia.3
2.2 Updated definition and the diagnostic algorithm (EWGSOP2 and AWGS2019)
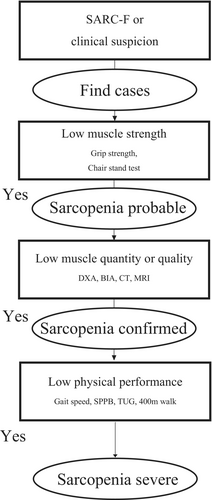
Studies have revealed that a decline in muscle mass does not always correlate with a decline in muscle strength or adverse outcomes. Hence, the understanding of reduced muscle strength, quality, and functional decline as more crucial factors than low muscle mass when assessing sarcopenia in older adults is increasing.8-11 In 2019, EWGSOP2 updated the definition of sarcopenia and developed new diagnostic criteria with clear cut-off values. The updated definition clarified sarcopenia as a muscle disease (muscle failure) rooted in adverse muscle changes that accrue over a lifetime. Sarcopenia is prevalent among older adults but can also occur earlier in life; therefore, it is now recognized to start even before 60 years of age. Additionally, EWGSOP2 emphasized low muscle strength as a key characteristic of sarcopenia, used the detection of low muscle quality or quantity to confirm the diagnosis of sarcopenia, and identified low physical performance as indicative of severe sarcopenia.2 Consequently, probable sarcopenia can now notably be diagnosed solely on the basis of a decrease in grip strength, with recommended intervention at that point. Based on these criteria, EWGSOP2 proposed a new case-finding, diagnosis, and severity algorithm (Figure 1). In 2020, AWGS2019 proposed a new consensus report that retained the previous definition of sarcopenia but revised the diagnostic algorithm, protocols, and certain criteria.6 Particularly, this algorithm recommended the use of methods, such as calf circumference and strength, assisting with walking, rising from a chair, climbing stairs, and falling (SARC-F) or SARC and calf circumference (SARC-CalF) criteria, as a tool for case identification, as skeletal muscle mass measurement is difficult in regional or primary care settings.12, 13 In medically well-equipped hospitals and research facilities, AWGS2019 continued to use the algorithm from AWGS2014, in which both skeletal muscle mass and strength were considered essential to diagnose sarcopenia. Table 1 shows a comparison of the latest definition/characteristics and cut-off values for sarcopenia in the EWGSOP2, AWGS2019, and IWGS criteria.2, 3, 7
| EWGSOP22 | AWGS20197 | IWGS3 | |
|---|---|---|---|
| Muscle mass | |||
| Skeletal mass index |
Men <7.0 kg/m2 Women <5.5 kg/m2 |
Men <7.0 kg/m2 Women <5.4 kg/m2 (by DXA) Men <7.0 kg/m2 Women <5.7 kg/m2 (by BIA) |
Men <7.23 kg/m2 Women <5.67 kg/m2 (by DXA) |
| Muscle strength | |||
| Grip force |
Men <27 kg Women <16 kg |
Men <28 kg Women <18 kg |
- |
| Chair stand test (for five rises) | >15 s | ≥12 s | - |
| Physical performance | - | ||
| Gait speed | ≤0.8 m/s | <1.0 m/s | <1.0 m/s |
| SPPB | ≤8-point score | ≤9-point score | - |
| TUG | ≥20 s | - | - |
| 400-m walk test | Noncompletion or ≥6 min for completion | - | - |
- Note: If not specified, the criteria are the same for both men and women.
- Abbreviations: BIA, bioimpedance analysis; DXA, dual-energy X-ray absorptiometry; SPPB, short physical performance battery; TUG, timed-up and go.
2.3 Epidemiology of sarcopenia
Skeletal muscle undergoes constant protein synthesis and breakdown, and the balance of this cycle is crucial for maintaining skeletal muscle mass. An imbalance in muscle metabolism occurs in older adults, and muscle mass decreases by 1%–2% annually after 50 years of age even in healthy individuals. Therefore, over the age span of 20–80 years, the loss of muscle mass results in an approximate 30%–40% reduction.14, 15 Muscle strength experiences a more rapid loss, as a longitudinal study indicates that at 75 years of age, strength diminishes at 2.5%–4% per year (3%–4% per year in males and 2.5%–3% per year in females).15 Consequently, muscle strength in older adults decreases by 20%–50% compared with that in younger individuals.16 Changes in muscle quality, such as fiber type composition, cross-sectional area, myonuclear content, and satellite cell content, may also contribute to these declines in muscle mass and strength.17 Overall, the prevalence of sarcopenia is high in older adults. Furthermore, the prevalence ranges from 1% to 30% in community-dwelling populations aged ≥50 years, although it varies according to the diagnostic criteria.16, 18 A recent meta-analysis reported that the global prevalence was estimated to be 10% (95% confidence interval [CI]: 2%–17%) in individuals aged ≥60 years, following the EWGSOP2 criteria.19 In a large-scale cohort study in Japan, Yoshimura et al. estimated the prevalence to be approximately 8.2%.20 However, unified diagnostic criteria have not been established so far, and a single diagnostic criterion for sarcopenia is required for further advancement of sarcopenia research.
2.4 Causes of sarcopenia
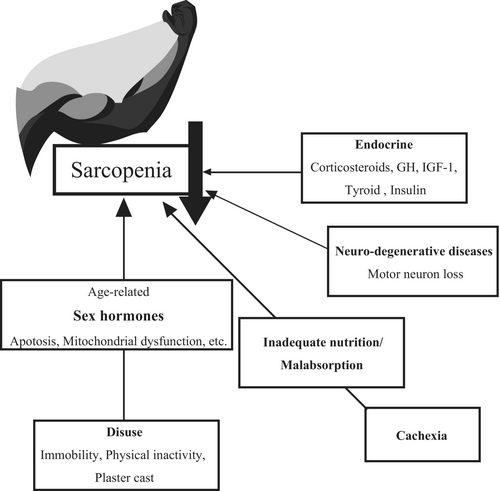
Sarcopenia has a complex, multifactorial etiology; therefore, its pathophysiology remains unclear. Sarcopenia is associated with aging, and its onset is determined by various factors, including disuse, malnutrition (low protein intake), cachexia, neurodegenerative diseases, endocrine imbalances, and age-related metabolic and functional decline (Figure 2).11, 21 Among these factors, changes in humoral factors, particularly sex steroid hormones, have gained significant attention. Hormones responsible for maintaining homeostasis, such as glucocorticoids and thyroid hormones, are generally preserved with aging. In contrast, sex hormones, such as testosterone and estrogen, decrease with age. Currently, approved medications for treating sarcopenia remain unavailable; however, medications related to androgens are highly anticipated among the treatments demonstrating promising clinical applications.22 Interestingly, the incidence of sarcopenia is reported to contain sex-specific aspects, with females having a 20% higher risk of developing sarcopenia than males, indicating the contribution of sex hormones.9
3 ANDROGEN, FRAILTY, AND SARCOPENIA
3.1 What is an androgen?
Androgens are essential male hormones involved in the development and maintenance of the male phenotype. They belong to the steroid hormone family and are mainly secreted from the testes, ovaries, and adrenal glands. Testosterone, the primary androgenic hormone, exerts its effects through both genomic and nongenomic pathways. The androgen receptor (AR), which is expressed in various tissues throughout the body, predominantly mediates the genomic pathway. Therefore, its target organs are diverse, including the skeletal muscles, bones, skin, central nervous system, prostate, and generative organs.
Testosterone exerts anabolic effects and increases both muscle size and strength.23, 24 Testosterone enters target cells and undergoes conversion to its biologically potent form, dihydrotestosterone (DHT), with the enzyme 5α-reductase. Subsequently, testosterone and DHT bind to AR in the cytoplasm. The activated AR then translocates into the nucleus and binds to specific DNA sequences, also known as androgen response elements, or is tethered to muscle-specific enhancers located in the promoter regions of target genes. Consequently, AR plays the role of a transcription factor and regulates the expression of proteins involved in glucose and protein metabolism.24-26
3.2 Androgens and aging
Testosterone regulates many domains of sexual function in males and females. The secretion of testosterone, along with its precursors dehydroepiandrosterone (DHEA) and DHEA sulfate (DHEA-S), decreases as males age. The androgenic hormone levels generally decrease by 40%–50% in older age compared with younger age, with free testosterone levels particularly decreasing by 60%.27 This age-related low testosterone state in males, also known as LOH syndrome, is strongly associated with sexual dysfunction, including low sexual desire, reduced nocturnal erections, and ejaculate volume.28, 29 Additionally, LOH syndrome is related to the loss of bone density and muscle mass, and the positive correlation between serum-free testosterone concentration and skeletal muscle mass/strength is widely recognized.27, 30-32 Consequently, low testosterone levels are associated with functional impairment, increased risk of falls, and decreased quality of life.33 Orwell et al. investigated the association between testosterone levels and fall risk over a 4-year follow-up period in males aged ≥65 years and revealed that males in the lowest quartile of testosterone demonstrated a 40% higher risk of falls than those in the highest quartile.34 Based on the United States National Health and Nutrition Examination Survey III, Eichholzer et al. reported that males with low free testosterone (<243 pmol/L) or high sex hormone-binding globulin serum levels (≥66 nmol/L) were associated with significantly increased odds of frailty (odds ratio [OR] = 2.97, 95% CI: 1.28–6.86; OR = 3.92; 95% CI: 1.29–11.89, respectively).35 Testosterone is known to reduce with age in both sexes, but most studies have focused on males, and the benefit of androgenic hormones in females remains largely unresolved.33
A meta-analysis by Correa et al. revealed that androgen replacement therapy (ART) is associated with increased muscle mass and strength in addition to physical performance in middle-aged/older males.36 However, ART is associated with potential side effects, such as prostatic hypertrophy and cardiovascular events.23 Therefore, safer treatment methods are required. Resistance training is considered a safer alternative because it has been reported to increase testosterone and DHEA levels without notable side effects.37, 38 We recently reported that exercise increases the expression of AR mRNA both in vivo and in vitro, resulting in the regulation of interleukin-6/signal transducer and activator of transcription 3 signaling, thereby further indicating the efficacy of exercise.39
3.3 Anabolic effects of androgens
Several studies have revealed that the target genes of androgens include important genes for skeletal muscle maintenance and fiber shift, such as myoblast determination protein 1, insulin growth factor-I, myostatin, and follistatin.24, 25, 40 Moreover, recent data indicate that androgens mediate nontranscriptional actions, including activation of phosphoinositide 3-kinase (PI3K)/Akt pathway, which plays a crucial role in the pathophysiology of sarcopenia.11, 41, 42 The PI3K/Akt pathway induces hypertrophy by stimulating protein synthesis and inhibiting protein degradation. PI3K/Akt activates the mammalian target of rapamycin, which in turn activates the downstream 70-kDa ribosomal protein S6 kinase and eukaryotic initiation factor 4E, resulting in protein synthesis. Concurrently, the pathway inhibits fork head box O (FoxO) nuclear translocation, thereby blocking the suppression of transcription of the atrophy-related genes atrogin-1 and muscle ring finger 1.43 Other mechanisms have been reported, including the impact on satellite cells through Notch signaling and the regulation of mitochondrial function cytokines and inflammation in skeletal muscles.44-47
3.4 Phenotypes in AR knockout (ARKO) mouse models
The analysis of ARKO mice has been instrumental in further determining the anabolic function of the androgen/AR axis in the muscle. MacLean et al. generated whole-body ARKO mice and revealed that ARKO males demonstrated decreased body mass and muscle mass, with reduced muscle strength by fast-twitch muscles, whereas females exhibited normal phenotypes.48 However, Sato et al. reported that whole-body ARKO mice demonstrated significant effects beyond skeletal muscle, such as atrophic testes or female-like external genitalia.49 Therefore, analysis of skeletal muscle-specific ARKO mice was required, and these mouse models were developed using the Cre-LoxP system. Ophoff et al. and Chambon et al. developed a muscle-specific AR knockout (mARKO) mouse model using Cre recombinase under the control of the muscle creatine kinase promoter (MCK) and the α-skeletal actin promoter (HSA), respectively.50, 51 Both mARKO male mice demonstrated limited changes in muscle mass; however, the MCK-Cre mARKO mice exhibited no changes in muscle strength or fatigue, whereas the HSA-Cre mARKO mice showed impairment in the myofibrillar organization of sarcomeres and decreased muscle strength. Conversely, MCK-Cre mARKO mice showed that AR signaling contributed to fiber type regulation.50 Altogether, AR appeared to directly influence muscle quality, whereas its role in maintaining muscle mass may be more indirect, acting through AR in extramuscular tissues. Recently, we developed fast-twitch-specific mARKO mice using Mlc1f-Cre and longitudinally analyzed males until old age.52 This mouse model demonstrated reduced muscle strength and fatigue resistance, along with a fiber type shift toward slow-twitch muscle. Noteworthy, impaired muscle mass was observed in these mARKO male mice after middle age, indicating a change in the role of AR over time. Furthermore, we highlighted the association between AR and polyamine biosynthesis, which mediates the anabolic effects of androgens and is significantly altered in aged mice.53-55 Therefore, they are being considered as a novel therapeutic mechanism for sarcopenia treatment. Another recent study using HSA-Cre mARKO mice revealed impaired glucose and fatty acid metabolism in the skeletal muscle.56 This metabolic switch was also associated with decreased polyamine biosynthesis and promoted amino acid catabolism and oxidative stress, mitochondrial dysfunction, and myofiber necrosis, indicating lower muscle quality consistent with previous studies.
Androgens are strongly presumed to regulate numerous transcription factors, metabolic enzymes, and structural proteins through AR, which play a pivotal role in the pathology of sarcopenia. However, the molecular mechanism is complex, with many aspects remaining unclear, thereby requiring further research for clarification.
4 ESTROGEN, FRAILTY, AND SARCOPENIA
4.1 What is estrogen? Estrogen and aging
Estrogens, including 17β-estradiol, are female steroid hormones that play a crucial role in developing and regulating the female reproductive system and secondary sex characteristics. Estrogen levels in women markedly decrease throughout menopause. The decline in serum estrogen concentration, along with the absence of feedback inhibition, increases the secretion of luteinizing hormone and follicle-stimulating hormone from the pituitary gland.
Similar to androgens, estrogens also contribute to the regulation of protein synthesis in skeletal muscles; however, the mechanisms underlying this remain largely unsolved. Skeletal muscles demonstrate specific estradiol receptors (ERs) at the fiber levels: ERα, ERβ, and G protein-coupled receptors. Therefore, the biological effects of estrogen are expressed by binding to ER and subsequent activation of genomic and nongenomic pathways. In particular, evidence indicates that estrogen interacts with mitochondrial function and glucose and protein metabolism via ERs.47, 57, 58
Traditionally, androgens have been considered crucial for muscle metabolism, whereas estrogen has been considered important for bone metabolism.59 However, in recent years, the association between sarcopenia and estrogen has gained attention.60 Moreover, testosterone is metabolized by aromatase and undergoes conversion to 17β-estradiol.61, 62 Therefore, noteworthy, this process explains some of the above-mentioned effects of testosterone.
4.2 Estrogen and muscle phenotypes in ERKO mouse models
Kitajima and Ono investigated ovariectomized (OVX) female mice and revealed that reduced estrogen levels caused muscle atrophy, muscle strength, and fiber type shift toward fast-twitch muscle. Moreover, satellite cell function was affected in OVX mice, indicating the importance of estrogens in maintaining muscle function.63 Recently developed muscle-specific ERKO mice clarified the subject for a more detailed analysis of estrogens in skeletal muscles. Collins et al. developed female mice with muscle-specific ERαKO and revealed that ERα mediated the primary mechanism through which estradiol exerts its effects on strength.64 Seko et al. developed muscle-specific ERβKO and satellite cell-specific ERβKO female mice. These mouse models demonstrated that ERβ deletion in muscles reduced muscle mass, while ERβ deletion in satellite cells impaired muscle regeneration due to decreased proliferation and increased apoptosis of satellite cells.65
Despite the promising outcomes observed in these animal experiments, Javed et al. revealed the results of their meta-analysis on postmenopausal women aged ≥50 years, stating that estrogen replacement therapy (ERT) did not significantly slow the loss of muscle mass in females.66 However, concurrent changes, such as shifts in dietary quantity and quality, reduced levels of physical activity, and the onset of depressive states, are prominently observed in this population; therefore, the influence of these multiple confounding factors should be considered.67 The effectiveness of ERT in male patients with sarcopenia has never been reported and is limited to males with congenital aromatase deficiency.68 Androgens are the primary sex steroids in males, and estrogens also play a crucial role in skeletal health. Additionally, the secretion of estradiol decreases as males age, and the serum estradiol concentration falls below the threshold level necessary for maintaining bone mass in some cases.69 The interaction between muscles and bones is widely known; therefore, the potential usefulness of ERT in male skeletal muscles may be recommended in the future.11 Further research is required to investigate the detailed mechanisms of estrogen in skeletal muscle maintenance and to evaluate the potential benefits of ERT in both male and female patients with sarcopenia.
5 CONCLUSION
Sarcopenia is an age-related condition characterized by a progressive and systemic decline in skeletal muscle mass, quality, and strength. Advances in research have highlighted the importance of muscle strength over muscle mass, resulting in new diagnostic criteria for sarcopenia. The relationship between sex hormones and muscle mass, strength, and physical function is closely related, although many aspects remain incompletely understood. Evidence establishing the association between androgens and sarcopenia/frailty has been emerging, but studies on the association between estrogen and sarcopenia remain insufficient. The elucidation of the molecular mechanisms involving sex hormones is eagerly awaited and is expected to lead to novel therapeutic interventions for sarcopenia.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.