Quality of life and functional status after pulmonary endarterectomy for chronic thromboembolic pulmonary hypertension: A Swedish single-center study
Drs Bredin and Sartipy contributed equally to this manuscript.
GUARANTOR: Ulrik Sartipy.
Abstract
Little is known about long-term quality of life (QOL) and functional status after pulmonary endarterectomy (PEA) for chronic thromboembolic pulmonary hypertension (CTEPH). We investigated QOL and functional status late after PEA. All patients who underwent PEA for CTEPH 1993–2020 at one Swedish center were included. Baseline characteristics and data from right heart catheterization, 6-min walk test, and Cambridge Pulmonary Hypertension Outcome Review (CAMPHOR) were obtained from patient charts and national registers. The RAND 36-Item Health Survey was sent by post, and Karnofsky Performance Status (KPS) was evaluated by telephone. A total of 110 patients were included. The survey was completed by 49/66 (74%) patients who were alive in 2020. In all domains except for bodily pain, QOL was slightly lower than that of an age-matched reference population. The KPS score was obtained from 42/49 (86%) patients; of these, 31 patients (74%) had a KPS score of ≥80% (able to carry on normal activity). All 42 patients were able to live at home and care for personal needs. The median postoperative CAMPHOR scores were: 4 for symptoms, 4 for activity, and 2.5 for QOL. We observed that QOL after PEA approached the expected QOL in a reference population and that CAMPHOR scores were comparable to those of a large UK cohort after PEA. Functional status improved when assessed late after PEA. Three-quarters of the study population were able to conduct normal activities at late follow-up. Our findings suggest that many patients enjoy satisfactory QOL and high functional status late after PEA.
Patients suffering from chronic thromboembolic pulmonary hypertension (CTEPH) are often severely symptomatic and experience dyspnea and fatigue due to right heart failure.1 This condition is caused by unresolved pulmonary emboli, intimal hypertrophy, and fibrosis in the pulmonary arteries leading to increased pulmonary artery pressure and pulmonary vascular resistance,2, 3 and ultimately leads to death. Guidelines recommend pulmonary endarterectomy (PEA) as a first-line treatment for all operable patients with CTEPH.1 Balloon pulmonary angioplasty (BPA) or medical therapy are alternative treatment options for patients who are ineligible for surgery or have recurrent or residual pulmonary hypertension (PH) after surgery.3, 4 In a previous study, we demonstrated that life expectancy after PEA was reduced compared with that in the general population, although the difference was small.5 Ten-year survival after PEA is 69%–75%,5-7 whereas patients with CTEPH without surgical treatment have a 3- to 5-year survival rate of 60%–70%.4, 8 In previous studies, the quality of life (QOL) in patients with CTEPH has been described as impaired compared with that in the general population.9-11 Furthermore, patients who have undergone PEA experience better QOL than non-operated patients with CTEPH.12, 13 Prospective studies on BPA and medical therapy further report improved QOL.14-16 Very few studies have investigated long-term QOL after PEA. Study settings have been challenging given the rarity of the disease, small study sample sizes, and long study periods.12, 13, 17, 18 Moreover, a wide variety of approaches to assess functional status have been used, including the 6-min walk test (6MWT), World Health Organization (WHO) functional class, and the New York Heart Association (NYHA) class. Various instruments have been used to evaluate QOL—the EQ-5D, the Short Form-36/RAND 36-Item Health Survey (RAND-36), the Cambridge Pulmonary Hypertension Outcome Review (CAMPHOR), and the Borg dyspnea score—making a comparison of studies difficult.9 In a previous study, we investigated life expectancy following PEA for CTEPH.5 Data on very long-term QOL and functional status after PEA for CTEPH are lacking in a contemporary patient population. Therefore, we performed a descriptive cross-sectional investigation including all patients who underwent PEA for CTEPH at one center in Sweden. This study aimed to assess and describe QOL and functional status after PEA for CTEPH.
METHODS
Study design
This study combined data from a cross-sectional investigation of QOL and functional status with patient-level data obtained from two Swedish national quality registers and patient medical charts. Approval for this study was obtained from the Swedish Ethical Review Authority (registration number 2020-03133).
Study population and data sources
All patients who underwent PEA for CTEPH between 1993 and 2020 at Karolinska University Hospital were included in the study. Baseline characteristics and operative details were obtained from patient medical charts and the Swedish Cardiac Surgery register,19 which is a part of SWEDEHEART.20 The RAND-36 questionnaire was sent by post to all living patients in our cohort. Those who did not reply received one postal reminder and finally a reminder by telephone. All patients who returned the RAND-36 form were subsequently contacted by telephone for evaluation of Karnofsky Performance Status (KPS).
Data on the 6MWT, WHO functional class, right heart catheterization (RHC), and CAMPHOR score were obtained from patient medical charts and the Swedish Pulmonary Arterial Hypertension registry (SPAHR), the Swedish national quality register for pulmonary arterial hypertension and CTEPH.8 This register was launched in 2008; all Swedish specialist centers for pulmonary arterial hypertension and CTEPH report into the SPAHR. Of the total 1,782 incident and prevalent patients registered in the SPAHR, approximately 25% are patients with CTEPH. The 2020 SPAHR annual report identifies the completeness of data for RHC, 6MWT, WHO functional class, and CAMPHOR score at the time of diagnosis in patients with CTEPH for each referring center in 2011 and 2016.8 For example, in 2016, almost all newly diagnosed patients with CTEPH had undergone RHC and echocardiography, whereas CAMPHOR scores for only 15%–60% of patients were registered.
RAND 36-item health survey
The RAND-36 is a freely available version of the Short Form-36 (SF-36), which is the most used patient-reported outcome measure internationally.21 The RAND-36 is currently used in several Swedish national quality registries. In the RAND-36, patients answer 36 questions in eight domains defined by physical and psychological components. The eight domains are general health, bodily pain, vitality, physical functioning, role physical, mental health, role emotional, and social functioning. Reference data that can be used for norm-based comparisons are available for many populations. In the current study, the data obtained from RAND-36 were compared with an age-matched Swedish population.22
Karnofsky performance status
KPS describes patient status in relation to normal activity and work on a scale from 0% to 100%. The 0% score is given if the patient is dead and 50% is assigned if the patient is unable to work and can live at home and care for most personal needs but requires considerable assistance and frequent medical care. A score of 100% describes a patient with a normal daily life with no signs of illness.23 Because we included only living patients in the study, KPS scores of 0% were not recorded. A KPS score was determined for each patient by telephone interview in 2021.
6MWT, WHO functional class, and RHC
6MWTs and WHO functional class are common measures of functional status in patients with CTEPH. The preoperative value and the last recorded value for 6MWT were obtained from patient charts and missing values were completed with data from the SPAHR.
Preoperative WHO functional class was obtained from patient charts. Hemodynamic measurements were obtained from patient charts and missing values were completed with data from the SPAHR. Measurements from the preoperative RHC and the last performed RHC were obtained.
Cambridge pulmonary hypertension outcome review
The CAMPHOR is a validated instrument for measuring QOL in patients with PH24 and includes questions about QOL, symptoms, and limitations in activity. The scores have a negative correlation to symptoms; that is, a lower score indicates fewer symptoms or limitations. The maximum scores (i.e., indicating the worst outcome) are 25 for symptoms, 30 for activity, and 25 for QOL. The CAMPHOR has been translated into Swedish and has been validated for use in Sweden.25 The CAMPHOR score has been registered in the SPAHR since 2010. In 2019, a total of 68% of patients in the registry—including patients with pulmonary arterial hypertension and CTEPH—had a CAMPHOR score documented.
Statistical methods
Baseline characteristics were described as frequencies and percentages for categorical variables and means and standard deviations for continuous variables. Pre- and postoperative measurements were compared using paired sample t-tests and reported as mean differences including 95% confidence intervals (CIs). Data management and statistical analyses were performed using Stata 17.0 (StataCorp LP) and R version 4.2.1 (R Foundation for Statistical Computing).
RESULTS
We included 110 patients who underwent PEA for CTEPH between 1993 and 2020 at the Karolinska University Hospital in Stockholm and survived beyond 30 days after surgery. In September 2020, 66 of these patients were living and were sent the RAND-36 questionnaire by post. At the end of the follow-up on March 2, 2022, 61 patients were alive. The RAND-36 questionnaire was completed by 49 patients; among these patients, 42 provided a KPS score via telephone interview.
Baseline characteristics
Baseline characteristics are shown in Table 1. The mean age at the time of surgery was 61.2 years and 65% of patients were male. Chronic obstructive pulmonary disease was preoperatively diagnosed in 22% of patients. At the time of surgery, 51% of patients were never-smokers, 45% were former smokers, and 5% were active smokers. Peripheral artery disease was present in 5.5% of patients and 2.7% of patients had diabetes. A majority (92%) of patients had a history of venous thromboembolism, although only 7.3% had known risk factors for venous thromboembolism. Coagulopathy had been preoperatively diagnosed in 22% of patients. The mean preoperative 6-min walk distance (6MWD) was 362 m, 89% of patients were in WHO functional class III–IV, 19% of patients received home oxygen therapy, and 15% of patients had been on phosphodiesterase inhibitors preoperatively. The preoperative mean pulmonary artery pressure (mPAP) was 46 mmHg and the cardiac index was 2.1 L/min/m2.
| Variable | Total population | Missing data (%) |
|---|---|---|
| n | 110 | |
| Age (years), mean (SD) | 61.2 (12.6) | 0.0 |
| Female sex | 39 (35.5) | 0.0 |
| Body mass index (kg/m2) | 0.0 | |
| <18.5 | 0 | |
| 18.5–24.9 | 48 (43.6) | |
| 25–29.9 | 43 (39.1) | |
| ≥30 | 19 (17.3) | |
| Smoking | 0.0 | |
| Never | 56 (50.9) | |
| Former | 49 (44.5) | |
| Smoker | 5 (4.5) | |
| COPD | 24 (21.8) | 0.0 |
| Diabetes | 3 (2.7) | 0.0 |
| Peripheral artery disease | 6 (5.5) | 0.0 |
| Coagulopathy | 24 (21.8) | 0.0 |
| Riskfactor for VTE | 8 (7.3) | 0.0 |
| History of VTE | 101 (91.8) | 0.0 |
| WHO class | 0.9 | |
| I–II | 12 (11.0) | |
| III | 80 (73.4) | |
| IV | 17 (15.6) | |
| Poor mobility | 4 (3.6) | 0.0 |
| 6 min walk distance (m), mean (SD) | 362.4 (144.6) | 61.8 |
| Home oxygen therapy | 21 (19.3) | 0.9 |
| PDEi treatment | 16 (15.1) | 3.6 |
| Mean PAP (mmHg), mean (SD) | 45.8 (9.8) | 0.0 |
| Cardiac index (L/min/m2), mean (SD) | 2.1 (0.5) | 10.0 |
| PCWP (mmHg), mean (SD) | 10.0 (3.2) | 24.5 |
| PVR (dynes•s•cm−5), mean (SD) | 743.1 (302.6) | 1.8 |
| Endarterectomy reported as complete | 94 (85.5) | 0.0 |
| Year of surgery | 0.0 | |
| 1993–2003 | 24 (21.8) | |
| 2004–2011 | 39 (35.5) | |
| 2012–2020 | 47 (42.7) |
- Note: Numbers are n (%) unless otherwise noted.
- Abbreviations: COPD, chronic obstructive pulmonary disease; PAP, pulmonary artery pressure; PCWP, pulmonary capillary wedge pressure; PDEi, phosphodiesterase inhibitors; PVR, pulmonary vascular resistance; SD, standard deviation.
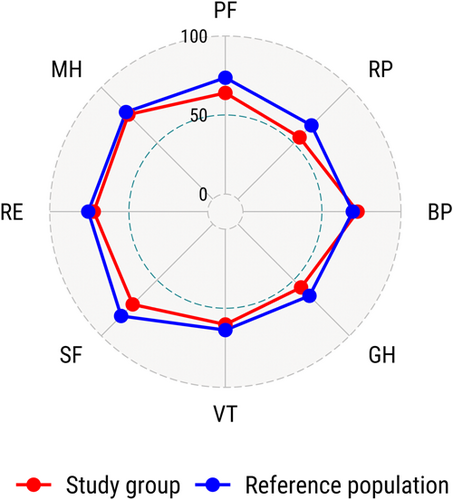
RAND-36
The RAND-36 was completed by 49 of 66 (74%) patients. The mean time from PEA to the evaluation of QOL by RAND-36 was 8.5 years (range: 1–24 years). The study population had slightly lower scores than the Swedish age-matched reference population in all domains except for bodily pain. The most affected domains were role physical and physical functioning (Figure 1). The RAND-36 scores from our study are compared with those in three other studies12, 17, 18 in Figure S1.
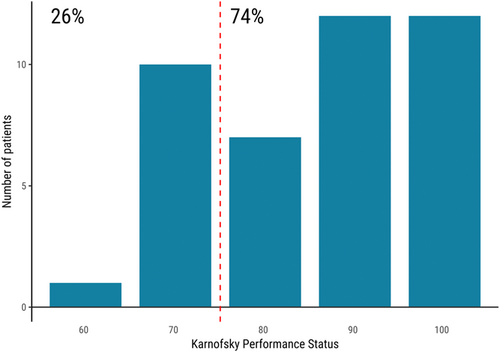
Karnofsky performance status
The KPS score was obtained from 42 of 49 (86%) patients. Of these patients, 12 (29%) had a KPS score of 100% and 31 (74%) had a KPS score of 80% or higher (i.e., were “able to carry on normal activity”). All 42 patients were able to live at home and care for most personal needs, although 11 (26%) patients were unable to carry out normal activities and work (Figure 2).
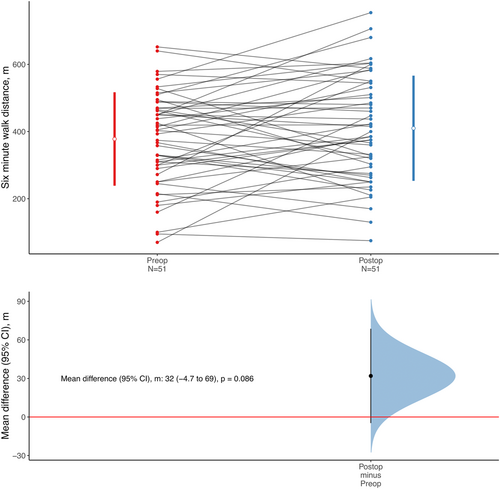
6-min walk test
The results for the 6MWT before and after PEA were available in 51 of 110 (64%) patients. The mean time from preoperative 6MWT to late measurement was 5.5 years (range: 0.2–19 years). The mean 6MWDs were 378 m before PEA and 410 m late after surgery. The mean difference was 32 m (95% CI: −4.7 to 69; p = 0.086; Figure 3).
Right heart catheterization
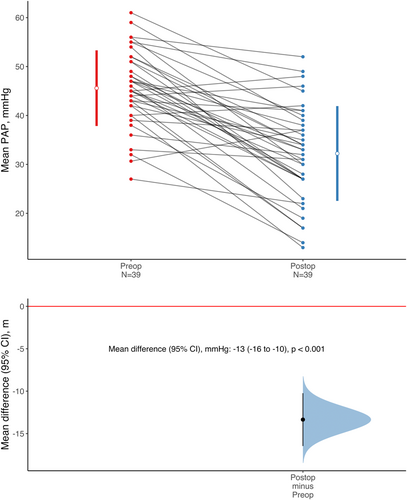
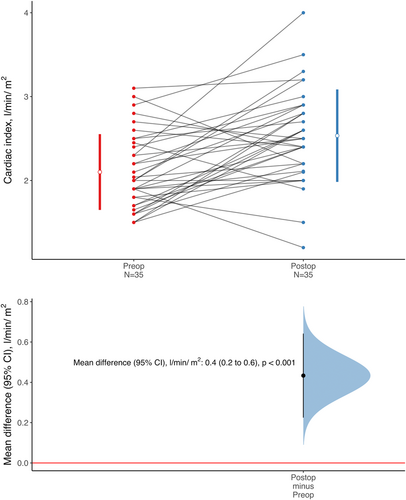
Pre- and postoperative evaluation of mPAP and cardiac index by RHC was available in 39 of 110 (35%) and 35 of 110 (32%) patients, respectively. The mean time from preoperative RHC to late measurements was 6.0 years (range: 0.9–17 years). The mean difference in mPAP was −13 mmHg (95% CI: −16 to −10; p < 0.001; Figure 4). The mean difference in cardiac index was 0.4 L/min/m2 (95% CI: 0.2–0.6; p < 0.001; Figure 5).
Cambridge pulmonary hypertension outcome review
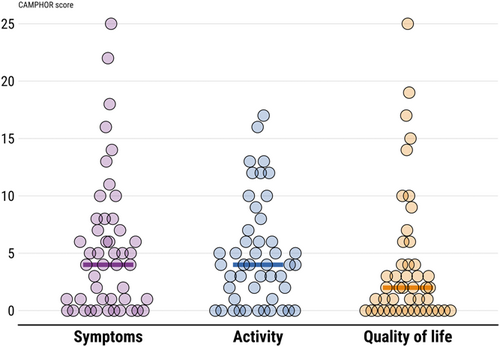
Data on CAMPHOR were available postoperatively in 47 of 110 (43%) patients and are presented in Figure 6. The mean time from PEA to the evaluation of QOL by CAMPHOR was 5.9 years (range: 0.4–20 years). Median post-PEA CAMPHOR scores across the three domains were 4 for symptoms, 4 for activity, and 2.5 for QOL.
Residual PH post-PEA and functional status and QOL
Health-related QOL (RAND-36, CAMPHOR scores) and functional status (KPS score, 6MWD) was evaluated in patients stratified by presence of residual PH defined as early postoperative mPAP ≥30 mmHg. These exploratory analyses showed a trend for worse functional status and QOL in patients with residual PH and are shown in Figures S2–S5.
DISCUSSION
We observed that QOL after PEA as measured with the validated instrument RAND-36 approached the expected QOL in an age-matched general population in Sweden. Moreover, CAMPHOR scores were low and comparable to those observed in a large United Kingdom (UK) cohort of patients with CTPEH following PEA. Functional status according to 6MWT improved slightly between the period before PEA and late after PEA and the KPS indicated that three-quarters of study participants were able to conduct normal activities at late follow-up without the need for specialized care. More data on health-related QOL following PEA for CTEPH is needed. A recent review of QOL in patients with CTEPH concluded that QOL in patients with CTEPH was lower than that in a healthy population, that PEA for CTEPH significantly improved QOL, and that more studies are needed to further validate appropriate QOL instruments in this patient population.9 The review further observed that CAMPHOR is the only QOL instrument that is validated specifically for PH and that comparisons of QOL data between studies are difficult because different instruments have been used. A summary of the previous literature on health-related QOL and functional status following PEA for CTEPH is shown in Table 2.
| Domain | Study, year of publication | Period of surgery | Comparator | Follow-up time | Findings |
|---|---|---|---|---|---|
| Quality of life | |||||
| SF-36 or RAND-36 | Archibald,12 1999 | 1970–1994 | Nonoperated patients, healthy population | Mean: 3.3 years, range: 1–16 years | Improvement |
| Tamada,18 2019 | 2014–2016 | Pre- vs. post-op, national average | 4 months | No difference, worse compared with average Japanese population | |
| Kamenskaya,17 2020 | 2011–2016 | Pre- vs. post-op | 3 years | Improvement | |
| CAMPHOR | Newnham,13 2020 | 2006–2017 | Pre- vs. post-op, nonoperated CTEPH | 1 year, 5 years | Improvement |
| Functional status | |||||
| Karnofsky Performance Status | – | ||||
| WHO or NYHA class | Archibald,12 1999 | 1970–1994 | Self-estimated pre- and post-op | Mean: 3.3 years, range: 1–16 years | Improvement |
| Tamada,18 2019 | 2014–2016 | Pre- vs. post-op | 4–8 months | No difference | |
| Newnham,13 2020 | 2006–2017 | Pre- vs. post-op | 1 year | Improvement | |
| 6-min walk test | Tamada,18 2019 | 2014–2016 | Pre- vs. post-op | 4–8 months | Improvement (not significant) |
| Newnham,13 2020 | 2006–2017 | Pre- vs. post-op | 1 year | Improvement |
- Abbreviations: BPA, balloon pulmonary angioplasty; NYHA, New York Heart Association; WHO, World health organization.
Health-related QOL
The San Diego group conducted the first study on QOL in patients after PEA for CTEPH in 1999.12 The group investigated a cohort of 514 survivors that were discharged after PEA between 1970 and 1994. Of 514 patients, 123 were lost to follow-up, 51 had died, and 14 and 3 were excluded because of language difficulties and lung transplantation, respectively. The study design was cross-sectional and 308 patients were included. Median time since PEA was 2.3 years (range: 1–16 years). The mean age at the time of the survey was 56.2 years (range: 19–89 years). The RAND-36 response rate was 97% (298/308). QOL after PEA was rated slightly below that of levels reported for healthy individuals in the United States. Postoperative QOL after PEA as measured with the RAND-36 was considerably better than for a group of pre-PEA patients. A study in Japan investigated QOL before and after PEA or BPA for CTEPH.18 The SF-36 was completed by 39 patients (n = 15 for PEA, n = 24 for BPA) before and after treatment. Significant differences in baseline characteristics were observed between the groups. Patients who underwent PEA had higher mPAP and pulmonary vascular resistance and lower exercise tolerance than patients treated with BPA. The mean follow-up times were 4.4 and 7.9 months for PEA and BPA, respectively. Mean mPAP declined from 43 to 25 mmHg following PEA whereas the cardiac index increased from 1.8 to 2.3 L/min/m2. The SF-36 scores were lower in both treatment groups compared with the national average. No significant difference was observed in QOL improvement between the BPA and PEA groups. In the PEA group, QOL improved significantly in the following domains: physical functioning, general health, vitality, and mental health. Kamenskaya et al. conducted a 3-year follow-up after PEA for CTEPH using the validated health-related QOL instrument SF-36.17 The response rate was 107/128 (84%), the mean age was 51 years, and 67% of the patients were men. Survival at 1 year was 91% and the 3-year survival was 90%. Hemodynamics improved: the mean mPAP dropped from 47 to 28 mmHg and the cardiac index improved from 1.9 to 2.9 L/min/m2 during follow-up. Health-related QOL further improved considerably, with increases in both physical (32–46) and mental (38–50) component summary scores. In all three studies, patients had a similar dramatic hemodynamic improvement after PEA.12, 17, 18 In two of the studies, the patient mean age at surgery was approximately 60 years,12, 18 whereas the mean age was lower (51 years) in the third study.17 Age likely affects experienced and reported QOL. In our study, we compared the QOL data in the study population with those from an age-matched general population in Sweden.22 We observed that the RAND-36 physical functioning and role physical domain scores were slightly lower in the study population compared with those in the age-matched general population in Sweden. However, scores in all other domains were very similar to those in the general reference population. Our findings were thus in line with those in the San Diego group's report.12 In contrast, health-related QOL measured with the SF-36 was low across all domains in the Japanese study.18 One reasonable explanation could be the differences in follow-up time after surgery. The follow-up time in the Japanese study was short (4 months) whereas the remaining studies included a longer mean follow-up time (approximately 3 years). Recovery from open heart surgery takes a fair amount of time; the patient usually recovers for 2–3 months from uncomplicated surgery and in complex cases, recovery can take up to 1 year.
The most comprehensive study of patient-reported outcomes following PEA was conducted in a UK cohort of patients who underwent surgery between 2006 and 2017.13 Hemodynamics improved: mean mPAP was reduced from 45 to 25 mmHg and cardiac index improved from 2.2 to 2.3 L/min/m2 at the 1-year follow-up. Patient-reported outcomes were assessed using CAMPHOR before and up to 5 years annually after PEA. At 1 year post-PEA, CAMPHOR scores were available in 784 (60%) patients and the number of patients with available data declined each year. A significant improvement in the CAMPHOR score was observed across all domains compared with findings in the preoperative survey. The median 5-year post-PEA CAMPHOR scores were 4 for activity, 2 for QOL, and 3 for symptoms. Patients with no residual PH—which is defined as post-PEA mPAP <30 mmHg—showed greater improvement in the CAMPHOR score than those with residual PH (mPAP ≥30 mmHg). A similar trend was observed in the present study, but these findings should be interpreted with caution due to the small sample size. Other studies have demonstrated an association between residual PH and long-term survival after PEA for CTEPH.26 Furthermore, CAMPHOR scores were higher in the post-PEA population than in propensity score-matched patients with CTEPH who did not undergo surgery. In our study, CAMPHOR scores were obtained 5.9 years (range: 0.4–20 years) after PEA and were very similar to those in the UK cohort.13 This may indicate that the improvement in patient-reported outcomes following PEA can be sustained beyond 5 years and that life-long improvement is possible in at least some patients. The elevated QOL results from this long-term follow-up might have been due to positive selection bias in the survivor group. Moreover, cultural differences in the perception of illness and health may have influenced answers in patient-reported outcomes.
Functional status
Functional status was evaluated by the San Diego group using the patient's self-estimated postoperative NYHA functional class. Two years after PEA, a majority of patients (93%) categorized themselves as NYHA class I–II.12 A clear improvement was also noted in the UK cohort: 88% of preoperative patients were in WHO functional class III–IV and 73% were in WHO functional class I–II 1 year postoperation.13 A distinctive aspect of our study compared to prior studies of functional status following PEA for CTEPH was the reporting of KPS. The KPS is a quick and simple method to evaluate functional status and performance relating to activities of daily life. A previous study showed a correlation between NYHA functional class and KPS.27 Interestingly, the study suggested that KPS provides better clinical discrimination between categories of functional status than the NYHA functional class. Although KPS is scarcely used in cardiovascular research, it is a robust measurement that can be intuitively interpreted and understood. Moreover, the KPS may better describe clinically meaningful deterioration—particularly at low levels of performance—than the NYHA functional class.27 In our study, we used KPS to assess functional status at late follow-up after PEA for CTEPH. Our results showed that all study participants were able to live at home and care for most personal needs and that 74% were able to conduct normal activities without the provision of specialized care. Notably, one-third of patients reported a 100% score (i.e., normal life, no complaints, and no evidence of disease) using KPS. Previous studies reported similar patterns of improvement in 6MWD after PEA for CTEPH.13, 18 In the UK cohort, the mean 6MWD pre-PEA was 309 m and increased to 366 m 1-year post-PEA.13 In the Japanese study, the mean 6MWD improved from 281 m preoperatively to 372 m postoperatively, although the improvement was not statistically significant.18 In both the United Kingdom and Japanese studies, the increases in 6MWD following PEA for CTEPH appear clinically relevant. The minimally important difference in 6MWD in patients with PAH is approximately 33 m.28 In our study, 6MWD improved by 32 m and was not statistically significant; however, this improvement could represent a clinically meaningful increase in functional capacity. Notably, according to prior research, improvement in 6MWD should be expected up to 2 years after PEA and appears to be sustained up to 5 years after surgery.29 Whether the improvement in 6MWD is sustained beyond 5 years or whether a natural decline occurs instead—perhaps because of greater age—is unclear.
Study limitations
This was a small single-center study and the study period spanned nearly three decades. Patient care has changed during this period; new treatment modalities such as medical therapy for PH and BPA have emerged. Data on whether patients had undergone BPA after surgery or whether PH medication had been used were not available. In this study, a large variation was observed in the follow-up times using all measurements. We lacked baseline (i.e., pre-PEA) RAND-36 and CAMPHOR data. RHC data late after PEA were only available in a subset of the study population. Although 74% of all living patients participated in the cross-sectional QOL evaluation by RAND-36, some patients did not respond even after reminders by post and telephone. Moreover, the study population was too small to evaluate possible sex differences.30 We can only speculate about the reasons for which patients declined to participate; whether these patients were too ill to answer or were feeling well and were therefore unwilling to take the time to participate is unknown. Finally, our study results may have been affected by the COVID-19 pandemic. Patients with CTEPH are considered at high risk for contracting COVID-19. Some patients had placed themselves in strict self-quarantine, especially before vaccines became available. The RAND-36 was sent out in 2020 before vaccines were available; some patients included notes in questionnaires reporting that they felt physically restrained because of self-quarantine during the COVID-19 pandemic.
In conclusion, we observed that QOL after PEA approached the expected QOL in a reference population and that CAMPHOR scores were comparable to those in a large UK cohort after PEA. Functional status improved slightly when assessed late after PEA, and three-quarters of the study population were able to conduct normal activities at late follow-up without the need for specialized care. Our findings suggest that many patients enjoy a satisfactory QOL and high functional status late after PEA. For a better understanding of patient-reported outcomes late after PEA, longitudinal studies using validated instruments are needed.
AUTHOR CONTRIBUTIONS
Janica Kallonen, Matthias Corbascio, and Ulrik Sartipy: conceived and designed the research. Janica Kallonen and Ulrik Sartipy: acquired the data, performed statistical analyzes, and drafted the manuscript. Janica Kallonen, Matthias Corbascio, Göran Rådegran, Fredrik Bredin, and Ulrik Sartipy: contributed to the interpretation of data, made critical revision of the manuscript for key intellectual content and have seen and approved the final version.
ACKNOWLEDGMENTS
The authors thank the SPAHR registry for providing data for this study. This work was supported by the Swedish Heart-Lung Foundation (grant number 20190533 to US), and Region Stockholm (ALF Project) (grant number RS2020-0731 to US).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHIC STATEMENT
Approval for this study was obtained from the Swedish Ethical Review Authority (registration number 2020-03133).
Open Research
DATA AVAILABILITY STATEMENT
The data underlying this article are available in the article and in its online Supporting Information Material.