Bmpr2 mutant mice are an inadequate model for studying iron deficiency in pulmonary hypertension
Soban Umar and Airie Kim are contributed equally to this work.
Abstract
As bone morphogenetic protein receptor type II (Bmpr2) mutations are the most common genetic cause of pulmonary arterial hypertension (PAH), and iron deficiency (ID) is associated with worse clinical outcomes in PAH patients, we proposed to use Bmpr2 ± mice to induce a model of ID in pulmonary vascular disease. Our study shows that these transgenic mice are not a good model for this clinical phenomenon.
Mutations in bone morphogenetic protein receptor type II (BMPR2), a member of the transforming growth factor-β family, are the most common genetic cause of pulmonary arterial hypertension (PAH). BMPR2 mutations are found in 82% of patients with a family history of PAH, and are associated with disease development at a younger age.1 Even in patients with nonfamilial PAH with no BMPR2 mutations, BMPR2 protein expression and function are significantly decreased as compared to healthy controls (Ctrl),2, 3 demonstrating its importance for the development of both familial and nonfamilial PAH.
Despite the apparent BMPR2 abnormalities in PAH patients, only 15%−30% of individuals with BMPR2 mutations will develop the disease phenotype, indicating that a second hit is often necessary for these individuals to develop PAH.1, 4 One potential second hit is iron deficiency (ID), which is being increasingly recognized as an important comorbidity in these patients. Both ID and ID anemia are very common in PH, with studies reporting a 30%−43% prevalence in Group 1 PH.5-8 More importantly, the presence of ID in Group 1 patients has been associated with worsening of the clinical outcomes of 6-minute walk distance (6MWD), exercise tolerance, hemodynamics, and mortality,5, 9, 10 regardless of whether the ID is accompanied by anemia. Multiple clinical studies have shown that intravenous iron supplementation results in improvements in exercise tolerance, qualify of life, 6MWD, and hypoxia-induced pulmonary vasoconstriction.11-13 Previously, most studies evaluating the effects of ID in pulmonary hypertension have focused on Group 1 PAH, but a recent important study has shown that ID in Group 3 PH is also associated with increased mean pulmonary artery pressures and worse survival.14 As ID has been shown to potentiate the pulmonary vasoconstriction response to hypoxia,9 Group 3 PH patients with hypoxia could indeed be developing increased pulmonary pressures in the setting of ID.
The mechanistic relationship between iron metabolism and pulmonary vascular disease is largely undescribed. One potential link between ID and PAH is the master iron-regulatory hormone hepcidin, a small peptide that is induced in response to either inflammation via interleukin-6 (IL-6) or increased iron by BMP6 via the BMPR2 pathway.15 Hepcidin is elevated in PAH patients despite an impaired BMP signaling pathway, and this elevation does not correlate with either IL-6 or CRP levels.9 To confirm this paradoxical increase in hepcidin levels, in vitro studies using BMPR2-deficient HepG2 cells and endothelial cells also showed increased BMP6-mediated downstream signaling16 and hepcidin expression.9 As hepcidin acts by inhibiting intestinal iron absorption and the efflux of intracellular iron to the circulation,17 this unexplained increase in hepcidin levels would lead to the decreased iron availability as seen in PAH patients. The downstream effects of iron-deficient pulmonary endothelial cells and smooth muscle cells remain unclear, though studies suggest that dysfunctional mitochondrial iron metabolism is important in the development of PAH.18 While the underlying mechanistic relationship between iron metabolism and PAH remains unclear, the clinical relevance has prompted changes in PAH management, including the 2015 European Society of Cardiology PAH guidelines that recommend screening for and potentially treating ID.19
We proposed to create a transgenic mouse model of ID in PAH that could be longitudinally assessed with noninvasive hemodynamic measurements. Despite the clinical relevance of ID in PAH, there have been no such mouse models generated to our knowledge. We generated Bmpr2 heterozygous (Het) and littermate Ctrl mice by crossing Bmpr2 floxed mice20 (kindly provided by Dr. Paul Yu from Harvard University) with cytomegalovirus (CMV)-Cre mice, and Het deletion of Bmpr2 was confirmed by qPCR (−ΔCT (Hprt-Bmpr2): Ctrl −3.49 ± 0.09 vs. Het −4.27 ± 0.36, Figure 1a). Male and female Bmpr2 Het and Ctrl mice were weaned onto regular chow (185ppm Fe) or a low-iron (4 ppm Fe diet) for 2 or 5 months. Mice on the low-iron diet had a significant decrease in liver iron stores after 2 and 5 months on the diet, confirming decreased iron stores, and there was no significant difference in hepatic iron stores between the Bmpr2 Het and Ctrl mice (Figure 1b). We also measured the hepatic expression of hepcidin via Hamp mRNA. As hepcidin expression is suppressed by ID, and dysfunctional BMPR2 signaling appears to lead to increased hepcidin expression, we expected hepcidin to be lower in both genotypes on iron-deficient diet but with an attenuated decrease in Bmpr2 mice. However, we found that while liver Hamp mRNA decreases overall in response to ID, partial loss of BMPR2 had no significant effect on hepcidin expression at any time point (Figure 1c).
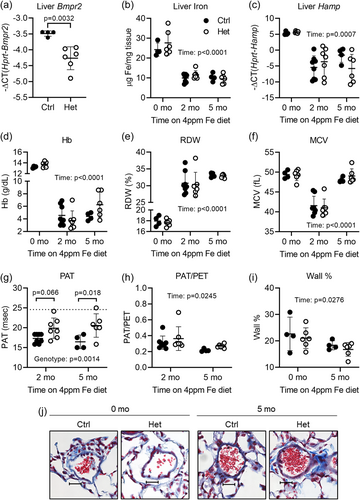
The complete blood counts also showed no significant effect of BMPR2 loss on the iron-deficient phenotype. As expected, mice on the low iron diet had decreased hemoglobin as compared to mice on regular diet, which is consistent with iron-deficiency anemia (Figure 1d). Also unsurprising was the increased red cell distribution width, likely largely secondary to concurrent microcytosis from ID and relative macrocytosis from a relative increase in reticulocyte percentage (Figure 1e). Mean corpuscular volume (MCV) was also decreased at the 2-month time point, as expected due to iron-deficiency anemia, but then recovered back to normal values by 5 months (Figure 1f). This normalization of MCV at the later time point could be secondary to a further increase in reticulocyte percentage with ongoing ID, although reticulocyte measurements would be necessary to confirm this. Thus, the hematological parameters showed no significant difference between Bmpr2 Het and Ctrl mice at any time point.
PAH severity was assessed via transthoracic echocardiography measurements of pulmonary acceleration time (PAT) and the ratio of PAT to pulmonary ejection time (PAT/PET).21 Prior reports in the literature have described the development of PH in murine models of ID,22 and our study also demonstrated increased PH severity in both Ctrl and mutant iron-deficient mice, as demonstrated by lower PATs than those of baseline wild-type mice (indicated with dotted line) (Figure 1g). Surprisingly, iron-deficient Bmpr2 Het mice had the same or mildly higher PATs than their littermate Ctrls at both the 2-month (Ctrl 17.29 ms vs. Het 19.88; difference −2.59, 95% CI [−5.34 to 0.15]) and 5-month time points (Ctrl 16.46 ms vs. Het 20.56; difference −4.10, 95% CI [−7.52 to −0.68]) (Figure 1g). When using PAT/PET ratios as a parameter of PH severity (Figure 1h), we found that Bmpr2 Het mice no longer had any indication of decreased pulmonary hypertension as compared to Ctrls, suggesting that any subtle difference reflected in the PAT measurements is likely physiologically insignificant. Between the two time points, PAT/PET ratios for both genotypes were significantly lower after 5 months of low-iron diet as compared to 2 months. This decrease at the later time point could be secondary to the longer duration of ID contributing to the PAH phenotype. Because we were aiming to create a mouse model with functionally significant phenotypic differences that could be evaluated longitudinally, we did not perform right heart catheterizations to search for any subtle differences that may not have been evident by echocardiogram. Masson trichrome staining of pulmonary arteries of baseline and 5-month 4 ppm Fe mice also showed no significant differences in wall thickness as measured by wall % (Figure 1i−j), although there was an overall decrease in wall thickness at the later time point. In short, the analyzed PH parameters showed no consistent differences in the Bmpr2 mutant mice regardless of ID.
Our expectation was that ID could provide the “second hit” for BMPR2-related PAH development and worsen PAH outcomes. Previous investigations have shown that Bmpr2 Het mice do not develop pulmonary hypertension spontaneously, but a second hit with an inflammatory stimulus can cause worse RVSPs as compared to Ctrls.4 However, our Bmpr2 Het mice had similar or subtly improved PAH parameters as measured by echocardiography compared to Ctrl mice when on low iron diet, which is counter to the correlation between ID and worse PAH parameters shown in clinical literature. We also did not see a difference in hepcidin expression in the transgenic mice despite the partial Bmpr2 deletion.
Our contrary results could have several potential causes. The loss of Bmpr2 could be compensated by an increase in other BMP type II receptors, such as ACTR2A,17 potentially causing a net overall increase in BMP signaling in the lungs. Another potential explanation is the mouse model itself. The mutation in the Bmpr2 allele in the mouse model used for these experiments is a loss of function, with exons 4 and 5 deleted.20 This could potentially produce a truncated Bmpr2 that binds to BMP ligands and downregulates other BMP signaling with unexpected downstream effects. Use of a mouse model of PAH also limits any phenotypic differences we would expect, as mouse models develop much milder PAH as compared to rat models. Finally, we used a model of extreme ID with depleted iron stores and severe anemia. The resulting significant hepcidin suppression and lack of any phenotypic difference could be secondary to this exaggerated ID that may be masking differences that would be visible with a milder ID. Further studies using a milder model of ID may be necessary to draw out more subtle differences. In conclusion, there have been multiple clinical associations between ID and different subtypes of PAH, but this Bmpr2 mutant mouse model is not a robust model for elucidating this relationship.
AUTHOR CONTRIBUTIONS
All authors contributed to experimental design, data analysis, and manuscript preparation; Vida Zhang, Soban Umar, and Airie Kim performed experiments.
ACKNOWLEDGMENT
This study was supported by NIH R01HL159507 (AK).
CONFLICTS OF INTEREST
E. N. and T. G. are scientific cofounders of Intrinsic LifeSciences and Silarus Therapeutics. T. G. is a consultant for ADARx, Akebia, Chiesi, Pharmacosmos, Ionis, Incyte, Gossamer Bio, Global Blood Therapeutics, American Regent, Disc Medicine, RallyBio and Rockwell Scientific. E. N. is a consultant for Protagonist, Vifor, RallyBio, Ionis, Shield Therapeutics, Disc Medicine, Novo Nordisk, Imara and Chiesi. T. G. and E. N. are inventors on patent applications related to hepcidin and erythroferrone. A. K. has consulted for Pharmacosmos. The remaining authors declare no conflict of interest.
ETHICS STATEMENT
All animal experiments in this study were approved by the Animal Research Committee at University of California, Los Angeles (UCLA).