Computational studies of H5N1 influenza virus resistance to oseltamivir
Abstract
Influenza A (H5N1) virus is one of the world's greatest pandemic threats. Neuraminidase (NA) inhibitors, oseltamivir and zanamivir, prevent the spread of influenza, but drug-resistant viruses have reduced their effectiveness. Resistance depends on the binding properties of NA-drug complexes. Key residue mutations within the active site of NA glycoproteins diminish binding, thereby resulting in drug resistance. We performed molecular simulations and calculations to characterize the mechanisms of H5N1 influenza virus resistance to oseltamivir and predict potential drug-resistant mutations. We examined two resistant NA mutations, H274Y and N294S, and one non-drug-resistant mutation, E119G. Six-nanosecond unrestrained molecular dynamic simulations with explicit solvent were performed using NA-oseltamivir complexes containing either NA wild-type H5N1 virus or a variant. MM_PBSA techniques were then used to rank the binding free energies of these complexes. Detailed analyses indicated that conformational change of E276 in the Pocket 1 region of NA is a key source of drug resistance in the H274Y mutant but not in the N294S mutant.
Introduction
As one of the main causes of acute respiratory infection in humans, influenza A virus can lead to annual epidemics and infrequent pandemics. In 1997, the H5N1 avian influenza A virus caused six deaths among 18 infected persons in Hong Kong.1 In addition, it has attracted considerable international attention, because H5N1 bird flu has been found in more than 60 countries throughout the world.2 Currently, influenza A virus subtype H5N1 is one of the largest pandemic threats. Two classes of antiviral drugs are available: the adamantanes, including amantadine and rimantadine, which target the M2 ion channel of the influenza A virus, and the neuraminidase (NA) inhibitors, which target the NA glycoproteins of influenza A and B viruses.
The NA inhibitors were designed to treat a key step in the influenza virus life cycle, i.e., when the NA enzyme releases new virions from the infected cell. By interfering with the release of new influenza virions from infected host cells, the NA inhibitors effectively prevent the spread of infection. Two FDA-approved drugs, oseltamivir (Tamiflu) and zanamivir (Relenza), have been used extensively to treat influenza and stockpiled by countries in preparation for an avian flu pandemic. Oseltamivir has a significant clinical advantage over zanamivir in that it is administered orally; zanamivir is administered via nasal inhalation. However, the effectiveness of both drugs will deteriorate with the emergence of new drug-resistant influenza variants.2
Several oseltamivir-resistant variants have been reported after oseltamivir treatment of influenza-infected patients,3, 4, 5, 6 and a possible mechanism for drug resistance has been proposed.7 In this working model, the drug resistance of influenza viruses depends strongly on the binding properties of the NA-drug complexes. Key residue mutations within the active site cause conformational changes or diminish the binding of drugs with NA proteins, resulting in drug resistance. When oseltamivir binds with NA, amino acids within the active site rearrange to accommodate the drug's hydrophobic side chain. Any mutations that affect this rearrangement may result in resistance to the drug.7 Indeed, several H5N1 mutations in NA have been reported, including H274Y and N294S.6, 8-10 The replication efficiencies and pathogenicities of these variants after oseltamivir treatment were extensively investigated, and it was shown that H274Y and N294S mutants confer resistance to oseltamivir and do not compromise the ability of A/Vietuam/1203/04(H5N1) and A/PR/8/39(H1N1) viruses to replicate in vitro.11 Furthermore, the high pathogenicity of the wild-type (WT) virus is preserved in the drug-resistant H5N1 variants.11 The recent emergence of oseltamivir-resistant viruses indicate that the drugs currently in use may not fully protect humans. Thus, a new generation of anti-influenza drugs is needed. However, to develop new antiviral reagents, we need a clearer understanding of the molecular mechanisms of oseltamivir resistance in the H5N1 virus.
To better understand the molecular mechanisms of drug resistance, we intended to quantify the resistance in terms of changes in the binding free energy of protein-ligand complexes. To achieve this goal, we used computational molecular modeling and simulation methods to characterize drug-protein binding and ranked the binding free energies based on binding-energy calculations. Although several computational approaches are available to achieve this goal, e.g., Free-energy Perturbation, Thermodynamic Integration, Linear Response, and Molecular Mechanics/Poisson-Boltzmann Surface Area (MM_PBSA),12 we chose MM_PBSA to estimate the binding free energies. The MM_PBSA method has been successfully applied to a variety of protein-ligand interactions;13-16 in particular, it has been used for several theoretical studies on NA inhibitors.17, 18
In this study, we focused on the complexes of oseltamivir carboxylate (active form of oseltamivir) that bind WT H5N1 and three variants, H274Y, N294S, and E119G. The emergence of the H274Y and N294S variants was previously observed in oseltamivir-treated patents with H5N1 virus infection.6 Influenza A (H3N2) virus with E119G NA mutations was isolated from humans treated with zanamivir.19 Because this variant was not resistant to oseltamivir, we used it as a control to test the reliability of MM_PBSA in distinguishing between drug-resistant and non-drug-resistant variants. We first conducted a 6-ns molecular dynamic (MD) simulation for each complex and then used MM_PBSA to rank the binding free energies of all complexes. We then computed the free energy decomposition of the contributions to binding to investigate the drug resistance of the H274Y and N294S variants. Our analysis of the structure clearly explained their resistance in terms of the conformational change of residue Glu276 in the Pocket 1 region of NA.
Results
MD simulations of the WT and mutant forms of H5N1 NA bound with oseltamivir
The coordinates of the WT NA of the H5N1-oseltamivir carboxylate complex were obtained from the Protein Data Bank structure (2HU4). The structure of NA is a β-propeller structure consisting of six blades. The active site that binds to oseltamivir carboxylate is in the loop region on the top of the propeller and contains a large number of polar (or charged) residues (see Fig. 1). The mutant viruses were prepared by making the following residue substitutions: E119G, H274Y, and N294S. The complexes were solved in the TIP3P water box, with each side 9 Å from the edge of the complex. The total number of atoms was about 27,700. After neutralizing the complexes, we performed the 6-ns MD simulations with the Amber8 software package. To analyze the stability of the MD simulation, we plotted the root-mean-square deviation (RMSD) values relative to the initial structures of the H5N1 backbone atoms during the 6-ns MD simulation against time (Supporting information Figure 1). All complexes reached convergence within the first 0.5 ns and remained stable during the first 3 ns. For the remaining 3 ns, all structures showed minor fluctuations. To approximate the range of fluctuations, we calculated two average RMSD values, one for the first 3-ns period and one for the second 3-ns period. The maximum difference was 0.46 Å for the WT complex, which was greater than those of E119G (0.43 Å), H274Y (0.13 Å), and N294S (0.40 Å) complexes. Overall, the structures of the H5N1 complexes were well preserved during the MD simulation.
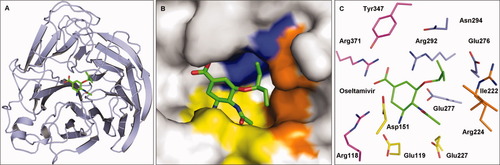
The propeller structure (A), the binding pockets (B), and key residues in the binding pockets (C) of the H5N1-oseltamivir carboxylate complex. Oseltamivir carboxylate (green) binds to residues of the influenza viruses at various locations, including the Pocket 1 (pale blue), Pocket 2 (orange), and Pocket 3 (yellow) regions. Nitrogen (blue) and oxygen (red) are also shown.
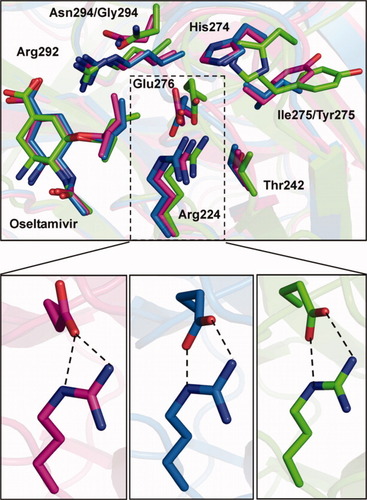
To further examine the effects of the each NA mutation, we plotted the RMSD of all atoms of the H274Y mutant in the complex with oseltamivir carboxylate relative to the initial structure within the 6-ns simulations (see Fig. 2). The initial structure was built based on the WT structure (2HU4). To inspect the conformational change, we chose three representative snapshots at the starting point, at relaxation, and at production. The structures were superimposed and fit onto the Cα atom in E276. The MD run started with the crystal structure of 2HU4 mutated by Y274 (Fig. 2, Structure 1), followed by an ∼4-ns structure relaxation. During relaxation, E276 first formed a bidentate salt bridge interaction with nearby R224, which distorted the carboxyl group of E276 to interact with R224 (Fig. 2, Structure 2). Then the E276 moved farther into binding site due to the bulkier Y274. This movement diminished the interaction between E276 and R224. As a result, the carboxyl group moved back to position similar to that of Structure 1 but much closer to the binding site (Fig. 2, Structure 3). After a 4-ns relaxation, the complex remained stabilized for the remaining 2 ns. While we were preparing the manuscript, crystal structures of drug-resistant H5N1-oseltamivir carboxylate mutants, including H274Y (3CL0) and N294S (3CL2), were reported.20 In terms of drug resistance, the key changes in the crystal structure of the H274Y mutant were on residue E276. The bulkier Y274 residue forces the carboxyl groups of the E276 to move farther toward the binding site. Our MD simulation predicted this conformational change correctly, and the structure of the H274Y at the end of the 6-ns simulation is essentially the same as the crystal structure 3CL0 [Fig. 3(A,B)].
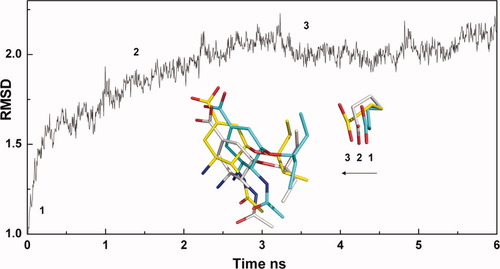
The root-mean-square deviation (RMSD) relative to the initial structure of all atoms in the mutant variants H274Y (black) during a 6-ns molecular dynamic (MD) simulation. Three representative snapshots at different stages including the (1) starting point (cyan), (2) relaxation (gray), and (3) production (yellow) are shown. The structures are superimposed on the Cα atom in Glu276.
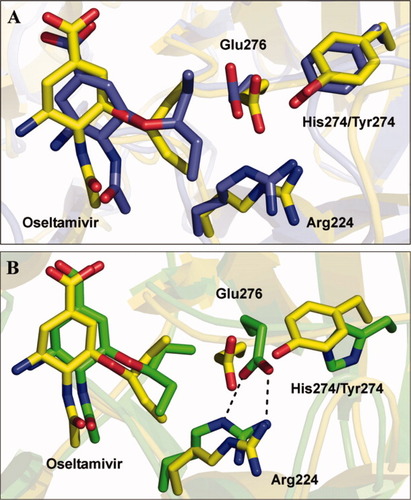
Superimposition of crystal structure and molecular dynamic (MD) structure of the H274Y mutant (A) and the superimposition of the MD structures of WT H5N1-oseltamivir carboxylate and the H274Y mutant (B). Carbons of the H274Y mutant in the crystal structures (slate) and those of the WT (green) and H274Y mutant (yellow) in the MD structures are shown, as are the nitrogen (blue) and oxygen (red).
The MD structure of the N294S mutant NA-oseltamivir carboxylate complex also predicted the change in the key structural features correctly but with one minor variation from the actual crystal structure. In a comparison of the crystal structures of the WT and the N294S mutant [Fig. 4(A)], the following two major structural changes were observed: (1) because of the loss of the asparagine side chain at position 294, the main-chain carbonyl of Y347 flipped out from its position in the WT to interact with R292; and (2) the hydroxyl group of the S294 residue formed a hydrogen bond with E276. In our MD simulations, the flip of the main-chain carbonyl of Y347 in the structure of N294S mutant [Fig. 4(B)] was in good agreement with that of the crystal structure. However, during our MD simulations, no hydrogen bond between S294 and E276 was observed. Instead, a stable bidentate salt bridge interaction between E276 and R224 was clearly observed during the MD simulations. Such difference was also observed in the MD simulation studies with the WT protein. Although N294 does not form a hydrogen bond with E276 in the crystal structure of WT protein, like the N294S mutant, E276 interacts with R224 through one oxygen site. However, during the MD simulations with the WT protein, the side chains of the two residues also formed a bidentate salt bridge.
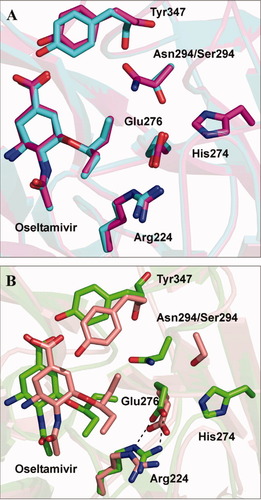
Superimposition of crystal structures (A) and molecular dynamic (MD) structures (B) of WT H5N1-oseltamivir carboxylate and the N294S mutant. Carbons of WT (magenta) and the N294S mutant (cyan) in the crystal structures are shown, as are the carbons of the WT (green) and the N294S mutant (orange) in the MD structures and the nitrogen (blue) and oxygen (red).
To examine the stability of the bidentate salt bridge in the WT and N294S mutant during the MD simulations, we performed multiple simulations (Supporting information Table I). First, we repeated simulation studies in triplicate with the WT (2HU4) and the N294S mutant (mutated from 2HU4). Second, we performed simulations with multiple starting points with slightly different positions of E276. These simulations began with different orientations and positions of E276 generated by adjusting the dihedral angle of carboxylate side chain of the residue. Third, we performed MD simulations using the newly published crystal structures of the N294S mutant (3CL2) as the starting point. Without exception, the bidentate salt bridge interaction remained stable after the systems reached equilibrium during all MD simulations.
| H5N1 | ΔEelec | ΔGPB | ΔGelec+PB |
|---|---|---|---|
| WT | −63.55 (0.62) | 68.98 (0.59) | 5.43 |
| N294S | −54.32 (0.75) | 67.75 (0.73) | 13.43 |
| H274Y | −60.99 (0.50) | 81.43 (0.47) | 20.44 |
| E119G | −120.44 (0.46) | 125.53 (0.41) | 5.09 |
- a All values are given in kcal/mol, with corresponding standard errors of the mean in parenthesis.Snapshots were taken every 5 ps for the enthalpy estimates and every 100 ps for the entropy estimates.
It has been widely reported that MD simulations can identify lower energy states by reorienting salt bridge-forming residues21, 22 or by changing the protein backbone conformation.23 Therefore, we propose that the bidentate salt bridge between R224 and E276, which was found in the MD simulation studies using the WT and the N294 mutant, presents a more stable state in solution. Consistent with this notion, we noticed that the conformation presented in our MD simulations can be observed in the crystal structure of the N(A)8-oseltamivir carboxylate complex.24 Because N8 and N1 belong to the group 1 of NAs and have similar active sites (see Fig. 5), it is very likely that the conformation of Glu276 in the N8 subtype also exists in the N1 subtype. Moreover, the bidentate salt bridge conformation was identified in another recent study,25 which used MD simulations to study the loop flexibility in the NA of H5N1. The simulation indicated remarkable topological changes and additional expansion of the inhibitor-binding pocket, as compared with crystal structure. A similar salt bridge interaction was indicated in a representative wide-open N1 structure.25
Binding free energies of NA-oseltamivir carboxylate complexes
The MM_PBSA method is typically used to determine binding free energies after the MD trajectory stabilizes.16 However, a stable RMSD does not always indicate that the binding free energies are stable. In particular, for an approach such as MM_PBSA that uses the converged energies to compute binding affinities and rank them, the stability of the energy is much more significant than that of the trajectory. Thus, to determine the period needed to accurately compute the MM_PBSA binding energies, a condition requiring stability in both the trajectory and energy has to be satisfied. In other words, adequate conformational sampling or a longer MD trajectory is necessary for high-quality MM_PBSA results.
To satisfy that condition, we calculated the MM_PBSA binding free energies for each snapshot (Supporting information Figure 2). Using the MM_PBSA method to determine the binding free energies of the complexes required that we determine the appropriate time period. To accurately analyze the energy contributions, we divided the binding free energy into several components, i.e., the gas-phase energy component (van der Waals and electrostatic contributions from solute), the polar solvation energy component (electrostatic contribution from solute-solvent interaction), and the nonpolar solvation energy component (cavity energy contribution) (Supporting information Figure 2). The binding free energies and other energy terms of the complexes fluctuated in small degrees during the first 4 ns. Furthermore, for the E119G mutant-oseltamivir carboxylate complex, the polar solvation energy was more favorable, and the gas-phase energy was more repulsive [Supporting information Figure 2(B)]. These features reflect the lack of negative charge on the glutamic acid residue. However, all energies of the WT and three mutants converged during the last 2 ns. Thus, we used only the last 2-ns portion of those trajectories in the MM_PBSA calculations.
 is the sum of the electrostatic contribution of solute (ΔEelec) and the polar solvation contribution of solute-solvent (ΔGPB); ΔEVDW is the van der Waals contribution; ΔTS is the entropy contribution; and
is the sum of the electrostatic contribution of solute (ΔEelec) and the polar solvation contribution of solute-solvent (ΔGPB); ΔEVDW is the van der Waals contribution; ΔTS is the entropy contribution; and  is the translational/rotational enthalpy contribution, which arises from six translational and rotational degrees of freedom. It is constant and equates to 6*1/2RT (−1.78 kcal/mol). Table I lists the electrostatic contributions from solute and solvent. Compared with other mutants, E119G has the more negative ΔEelec(−120.44 kcal/mol) and the more positive ΔGPB(125.53 kcal/mol). These differences result from the loss of a negatively charged glutamate residue. However, the overall
is the translational/rotational enthalpy contribution, which arises from six translational and rotational degrees of freedom. It is constant and equates to 6*1/2RT (−1.78 kcal/mol). Table I lists the electrostatic contributions from solute and solvent. Compared with other mutants, E119G has the more negative ΔEelec(−120.44 kcal/mol) and the more positive ΔGPB(125.53 kcal/mol). These differences result from the loss of a negatively charged glutamate residue. However, the overall  is similar to that of the WT system due to the cancellation of two terms. This finding indicates that the glutamate residue has less of an impact on
is similar to that of the WT system due to the cancellation of two terms. This finding indicates that the glutamate residue has less of an impact on  in the binding of H5N1 to oseltamivir carboxylate. N294S and H274Y have more positive values of
in the binding of H5N1 to oseltamivir carboxylate. N294S and H274Y have more positive values of  than does the WT complex. However, the variations in
than does the WT complex. However, the variations in  arise from different causes: N294S has a similar ΔGPB but a less negative ΔEelec, whereas H274Y has a similar ΔEelec but a more positive ΔGPB. These variations may be associated with the conformational changes of the two mutants in complexes.
arise from different causes: N294S has a similar ΔGPB but a less negative ΔEelec, whereas H274Y has a similar ΔEelec but a more positive ΔGPB. These variations may be associated with the conformational changes of the two mutants in complexes.The predicted binding free energies were −2.18 kcal/mol for the WT complex, −12.29 kcal/mol for the E119G variant, 6.57 kcal/mol for H274Y, and 1.35 kcal/mol for N294S (Table II). These values indicate that H274Y and N294S mutants diminish the binding of the drug with the H5N1 protein and result in drug resistance, whereas the E119G mutant most likely increases binding. Although the values of the estimated free energies are not accurate enough to compare with the experimental results, the relative ranking of binding free energies are in very good agreement with the experimental data.11 Indeed, Yen et al.11 reported that H274Y and N294S mutations conferred resistance to oseltamivir carboxylate and led to increases in 50% inhibitory concentrations of more than 250-fold and more than 20-fold, respectively.
| H5N1 | ΔEVDW | ΔGsur | ΔGelec+PB | ΔHbindb | ΔTS | ΔGbindc |
|---|---|---|---|---|---|---|
| WT | −25.82 (0.15) | −4.88 (0.01) | 5.43 | −25.27 (0.28) | −24.87(1.54)d | −2.18 (1.57) |
| N294S | −25.51 (0.16) | −4.88 (0.01) | 13.43 | −16.96 (0.41) | −20.09 (0.88) | 1.35 (0.97) |
| H274Y | −26.50 (0.14) | −4.70 (0.01) | 20.44 | −10.76 (0.32) | −19.11 (1.37) | 6.57 (1.41) |
| E119G | −30.60 (0.16) | −5.08 (0.01) | 5.09 | −30.59 (0.32) | −20.08 (1.49) | −12.29 (1.52) |
- a All values are given in kcal/mol, with corresponding standard errors of the mean in parenthesis. Snapshots were taken every 5 ps for the enthalpy estimates and every 100 ps for the entropy estimates.
- b The ΔHbind = ΔGelec+PB + ΔGsur + ΔEVDW.
- c The ΔGbind = ΔHbind + ΔTS + ΔHtrans/rot, and ΔHtrans/rot equates to 6*1/2RT (1.78 kcal/mol).
- d Two trajectories were excluded from the calculation due to large error. Without exclusion, the entropy value was −25.06 (2.29) kcal/mol.
Besides ranking the binding free energies correctly, another advantage of MM_PBSA is that it allows us to break down the total binding free energy into individual components, thereby enabling us to understand the complex binding process in detail. Positive
 values, such as those seen in the data from the H5N1 variants (Table II), indicate that the electrostatic energy is against the binding of oseltamivir carboxylate to the H5N1 protein, whereas the negative ΔEVDW values seen in all of the data indicate that the van der Waals interaction favors the formation of these complexes. As seen in Table II, the binding of the WT complex is electrostatically unfavorable, and ΔEVDWis the main driving force for the binding. This trend is consistent with previous theoretical studies.17
values, such as those seen in the data from the H5N1 variants (Table II), indicate that the electrostatic energy is against the binding of oseltamivir carboxylate to the H5N1 protein, whereas the negative ΔEVDW values seen in all of the data indicate that the van der Waals interaction favors the formation of these complexes. As seen in Table II, the binding of the WT complex is electrostatically unfavorable, and ΔEVDWis the main driving force for the binding. This trend is consistent with previous theoretical studies.17
In addition, individual energy components can be used to explain drug resistance, which is associated with free energy changes between H5N1 WT and variants, driven mainly by the balance of two energy components, ΔEVDW and
 . The differences between the binding free energy of the H274Y and N294S mutants and that of the WT are largely controlled by the electrostatic component (Table II), which resisted binding by 15.01 kcal/mol and 8.0 kcal/mol, respectively. The van der Waal interaction had a similar contribution to binding in the H274Y and N294S mutants. Thus, the total electrostatic energy component (
. The differences between the binding free energy of the H274Y and N294S mutants and that of the WT are largely controlled by the electrostatic component (Table II), which resisted binding by 15.01 kcal/mol and 8.0 kcal/mol, respectively. The van der Waal interaction had a similar contribution to binding in the H274Y and N294S mutants. Thus, the total electrostatic energy component ( ) was mainly responsible for the difference in binding free energies and might be the main cause of drug resistance. The E119G mutation changed the
) was mainly responsible for the difference in binding free energies and might be the main cause of drug resistance. The E119G mutation changed the  (−0.34 kcal/mol) and ΔEVDW (4.78 kcal/mol). In contrast with the findings in H274Y and N294S, those from the E119G indicated that ΔEVDW was the dominant contribution to the difference in binding free energies. Therefore, the binding free energy of the E119G mutant was lower than that of the WT complex.
(−0.34 kcal/mol) and ΔEVDW (4.78 kcal/mol). In contrast with the findings in H274Y and N294S, those from the E119G indicated that ΔEVDW was the dominant contribution to the difference in binding free energies. Therefore, the binding free energy of the E119G mutant was lower than that of the WT complex.
The entropy contribution arises from the loss of solute conformational degrees of freedom because of the positional and conformational restraints imposed by protein surface. Although the normal mode has some drawbacks, including the neglect of anharmonic motions and the use of a distance-dependent dielectric constant, it is still the most reliable method to estimate the entropy contribution. In our studies, we used all-atom NMODE module in Amber8 to calculate the entropy contribution (Table II). Because entropy calculation is computationally demanding, 21 trajectories were used for each complex. The standard error of the mean ranged from 0.88 to 1.54 kcal/mol, which is common for vibrational entropies computed by normal-mode analysis.26, 16 The only exception was the calculation of the WT protein, where the average value and standard error were derived from 19 trajectories; two trajectories that resulted in large errors were excluded. As seen in Table II, all three mutants had similar entropy values, which opposed ligand association by ∼20 kcal/mol. Compared with that of the mutants, the entropy of the WT was more unfavorable by ∼5 kcal/mol. For the mutants, this difference can be ascribed to the disruption of the salt bridge interaction between E276 and R224 in H274Y and the transformation from bulky to small side chain in N294S. For the E119G mutant, replacing the charged residue most likely destabilized the interaction between E119 and nearby charged residues resulted in entropy gain.
Discussion
The structures of H5N1 influenza virus NA bound to oseltamivir carboxylate gave a clear picture of how the NA protein interacts with its inhibitor.24 The NA active site contains three key binding pockets.27 Pocket 1 contains several polar and charged residues, including E276, E277, R292, and N294. In this pocket, E276 bonds with H274 and R224 to form a hydrogen bond network. R292 interacts with carboxyl group of oseltamivir carboxylate to form a salt bridge. These two interactions constitute a well formed and relatively rigid pocket to accommodate hydrophobic pentyl moiety. More interesting, the nature of Pocket 1 is purely hydrophobic, although it contains several charged residues. Previous studies have shown that the interaction between this pocket and pentyl moiety plays a key role in overall binding by establishing nonpolar-nonpolar interactions.28 Pocket 2 is a hydrophobic pocket that is surrounded by S246, I222, and R224 residues, which have strong hydrophobic interactions with the pentyl side chain of oseltamivir carboxylate. Pocket 3 is deeply buried when oseltamivir carboxylate binds with NA protein. Several negatively charged residues, including E119, E227, and D151, introduce additional electrostatic interactions with the amino group of oseltamivir carboxylate. Compared with Pocket 1, Pocket 3 contributes less to overall binding.27
For H5N1 variants H274Y and N294S, oseltamivir resistance takes place entirely in the Pocket 1 region. The mechanism of drug resistance of the H274Y mutant has been proposed in prior studies based on the crystal structures of H5N1 in complex with oseltamivir carboxylate24 and experimental studies, which found that the NA sensitivity to oseltamivir carboxylate strongly depends on the size of amino acid located at His274.29 According to the proposed mechanism, the resistance of H274Y might be a result of the reorientation of E276. This hypothesis is supported by the crystal structures of H274Y and N294S mutants with oseltamivir carboxylate. The replacement of H274 by the bulkier Y274 forces the carboxyl group of E276 to move closer (∼2 Å) to the binding site. This motion disrupts the accommodation of the pentyl side chain in Pocket 1 and decreases binding energies.
Our MD model of the H274Y mutant supports the mechanism of drug resistance described above. E276 undergoes a very similar rearrangement to that shown in the crystal structure of H274Y. However, we argue that ∼250-fold weaker binding of the mutant to oseltamivir carboxylate might result from a larger conformational change observed in the MD model, which involves changes in both orientation and distance of the carboxyl group of E276, rather than only change in distance of the carboxyl group of E276 as present in the crystal structure. Our energy analysis indicated that this conformational change that breaks the salt bridge between E276 and R224 in the WT could change the solvation energy ∼20 kcal/mol without affecting the ΔEelec and ΔEVDW. Therefore, the solvation energy change caused by the reorientation of E276 is probably the primary contributor to the drug resistance of the H274Y mutant.
For the N294S mutant, the salt bridge between E276 and R224 is maintained, and the E276 is not a key factor. Instead, there are at least two other structural features related to the weaker binding of the N294S-oseltamivir carboxylate complex. One is that the main-chain carbonyl of Y347 flips out to form a hydrogen bond with R292, and the other is that the S294 residue in the N294S mutant locates farther from the binding site than does N294 in the WT complex. The combination of these two effects reduces ΔEelec ∼11 kcal/mol without affecting ΔEVDW or ΔGPB.
As expected, the E119 residue plays a minor role in the binding of oseltamivir carboxylate to NA, because it is located within the Pocket 3 region. This effect can be attributed to a small amino group in this NA inhibitor, compared with the positively charged guanidine group in zanamivir, which contributes the most to the drug's overall binding. The minor impact of the E119 residue on the binding is also supported by our MM_PBSA calculations, which showed electrostatic energy contributions (ΔGelec+PB) similar to those seen in the E119G mutation (5.09 kcal/mol) and WT (5.43 kcal/mol). Unlike those in the H274Y and N294S mutants, the van der Waals interaction of the E119G mutant arising from the glycine was the major contributor to the difference between the binding free energies of the WT and the E119G variant. This resulted in a binding free energy lower than that of the WT complex. Thus, no drug resistance was detected.
Materials and Methods
The MD software package Amber830 was used to carry out a 6-ns MD simulation for each complex. All calculations were conducted with a 420-cpu IBM Linux cluster at the Hartwell Center for Bioinformatics and Biotechnology at St. Jude Children's Research Hospital. The Pharm99 force field31 and AM1-BCC charges32 generated from the antechamber module were assigned to protein and oseltamivir carboxylate, respectively. The starting structure of ligand-protein complex was prepared based on the crystal structure of H5N1 with oseltamivir carboxylate (PDB ID: 2HU4). The crystal structure of 2HU4 is a tetramer, and only one subunit was extracted from it to build the NA protein, which consisted of 385 amino acids. SYBYL software (Tripos, St. Louis, MO) was used to generate the H274Y, N294S, and E119G mutants. After replacements, the mutated residues were minimized, while other residues were kept fixed. Further minimization was then carried out to relax the whole complex systems.
To prepare MD calculations, we first neutralized the complexes of the WT and the mutants with oseltamivir carboxylate by adding Na+ counter-ions. TIP3P waters were then added to fill a truncated octahedral box with each side 0.9 nm from the edge of the complex. For each complex, the MD simulation included the following four steps: (1) the whole system was adjusted by a 1000-step steepest-descent minimization followed by a 9000-step conjugated-gradient minimization; (2) systems were heated from 100 to 300 K with 5 kcal/mol harmonic restraints via a 50-ps NVT MD simulation; (3) the restraints were gradually reduced to zero via a 50-ps NPT MD; (4) a 6-ns NPT MD simulation was conducted, and the production trajectories were saved every 5 ps. Once the MD runs were complete, we used the ptraj module in Amber8 to extract the trajectories for further analysis.
Acknowledgements
The authors thank Drs. Elena A. Govorkova and Hui-Ling Yen for insightful discussions and suggestions, Dr. Angela J. McArthur for editing the manuscript, the Hartwell Center for Bioinformatics and Biotechnology for computational time, and Scott Malone and Mi Zhou for technical support for Amber 8 analysis.




