Effect of nurse-led and physician-led multidisciplinary team palliative care on quality of life, negative emotions, and pain for cancer patients: A meta-analysis
Yunrong Li and Tiantian Wang should be considered joint first author.
Abstract
To systematically evaluate the effect of nurse-led and physician-led multidisciplinary team (MDT) palliative care models on quality of life, negative emotions, and pain for cancer patients. A comprehensive literature search of randomized controlled trials (RCTs) published in nine databases was conducted. Data analysis was performed using RevMan5.3. The findings were summarized using a random effects model of mean differences with 95% confidence intervals. The search strategy identified 15 articles involving 1850 cancer patients. MDT hospice care improved quality of life among cancer patients (SMD = 1.77, 95% CI [1.08, 2.46], Z = 5.02, p < .001), with nurse-led care (SMD = 3.04, 95% CI [2.29, 3.79], Z = 7.95, p < .001) providing better effects than physician-led care (SMD = 0.5, 95% CI [0.33, 0.67], Z = 5.76, p < .001). Furthermore, MDT hospice care significantly alleviated depression (SMD = –1.31, 95% CI [−1.49, −1.12], Z = 14.18, p < .001) and anxiety (SMD = –1.11, 95%CI [−1.29, −0.92], Z = 11.69, p < .001) and reduced patients' pain (SMD = –0.92, 95% CI [−1.13, −0.7], Z = 8.37, p < .001). Nurse-led care provided better effects for relieving anxiety and depression, while physician-led care provided better effects for relieving pain. The findings of the meta-analysis indicate that MDT palliative care can improve the quality of life for cancer patients and alleviate their depression, anxiety and their pain. Nurse-led care was superior in terms of quality of life, depression, and anxiety indicators, while physician-led care had a more significant effect on pain relief.
1 INTRODUCTION
The overall incidence of cancer in China is high, with estimates that 4.82 million people were newly diagnosed with cancer and 2.37 million people died of cancer in 2022.1 Despite great progress in cancer treatment in recent years, it remains difficult to extend the lives of cancer patients. Thus, there is a great demand for hospice care for cancer patients in China.2 The purpose of hospice care is to provide psychological, spiritual, and social support through a multidisciplinary team (MDT) to control pain and other uncomfortable symptoms and help end-stage patients experience a “superior death.”3 The hospice team generally adopts an MDT service model4 that includes staff from different disciplines such as specialist doctors, specialist nurses, nutritionists, psychological counselors, religious volunteers, and so on. Team members perform their respective duties and cooperate to provide care for end-stage cancer patients and their families to meet their complex physical, mental, and social needs. Previous studies have shown that, compared with traditional single-disciplinary hospice care, MDT hospice care provides better results,5, 6 such as improving patients' quality of life and easing negative emotions.7, 8 At present, MDT hospice care teams lack a fixed personnel structure, but the responsible physician and specialist nurse are key members9 of the team. According to the leaders and personnel composition of the team, MDT hospice care can be divided into two categories: physician-led and nurse-led hospice care. Although there are many clinical studies on the role of MDT hospice care for end-stage cancer patients, no meta-analyses or systematic reviews of the effect of MDT hospice care on end-stage cancer patients have been conducted and there are few reports comparing the two types of hospice care. To address these research gaps, we conducted a meta-analysis to evaluate the following questions: (1) What are the advantages of MDT hospice compared with conventional care? (2) What is the effect of nurse-led and physician-led MDT hospice care on cancer patients? We hope the findings will provide an evidence base for future studies on this topic.
2 METHODS
2.1 Search strategy
For this meta-analysis, the following databases were searched from establishment until December 1, 2023: PubMed, Medline, Web of Science, CINAHL, Cochrane Library, CNKI, Wanfang, VIP, and Sinomed. To ensure the inclusion of all available and relevant preliminary studies, the databases were searched using a combination of Medical Subject Heading (MeSH) terms and free text words.
2.2 Inclusion and exclusion criteria
For the purpose of this meta-analysis, the inclusion criteria were as follows: (1) Study design: randomized controlled trial (RCT); (2) Participants: patients with pathological or cytological diagnosis of malignant tumor, regardless of type, who were receiving multidisciplinary hospice care. (3) Intervention: The experimental group received multidisciplinary hospice care while the control group received routine or holistic nursing care. The hospice care team included professionals from different disciplines, such as responsible doctors, specialist nurses, dietitians, psychological counselors, and religious volunteers. The responsibilities of the team members included palliative care, basic nursing, psychological counseling, nutrition program formulation and spiritual care. According to the structure of the team, the experimental group could be categorized as nurse-led or physician-led; and (4) Outcomes: patients' quality of life, depression, anxiety, and social support were evaluated. Exclusion criteria were: (1) the data were incomplete or could not be extracted; (2) conference papers and repeated publications; and (3) the full text were not available.
2.3 Study selection and data extraction
The titles and abstracts were individually screened by two reviewers according to the inclusion and exclusion criteria. For abstracts that met the inclusion criteria, the complete papers were obtained. The reviewers then screened the full paper using the inclusion criteria. Papers that did not meet the inclusion criteria were excluded. Where there was disagreement between the two reviewers, a third reviewer was consulted to make a decision. Data extraction was performed independently by the two researchers to obtain the following aspects: study-related information, research subjects, sample size, intervention measures, control measures, intervention duration, outcomes, measurement instruments, and so forth.
2.4 Assessment of study quality
The quality of the included studies was graded according to the Cochrane Evaluation Manual 5.1.0.10 The evaluation considers the following seven aspects of each study: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. If these criteria are fully met then the study quality is graded A, which reflects the lowest risk of bias. If 1–3 aspects are assessed as unclear or at high risk, the risk of bias is considered moderate and the study quality rating is B. If >3 aspects are assessed as unclear or high risk, the risk of bias is considered high, the study quality rating is C, and the study is excluded. The assessment of study quality was performed by two independent researchers. Any disagreements were solved through discussion or consultation with a third researcher.
2.5 Statistical analysis
Meta-analysis was performed using Review Manager (RevMan 5.4.1). The mean difference (MD) was used as a continuous variable. If the measurement tools used in the studies were different, the standardized mean difference (SMD) was used as the effective index; if measurement tools were the same, the weighted mean difference (WMD) was used. Due to various measurement tools used in the included RCTs, the SMD and 95% confidence interval (Cl) were calculated as continuous variables. The Cochrane Q-test was used to assess statistical heterogeneity and was calculated as an indicator of heterogeneity in percentages. If >1 and/or <50%, there was no statistical heterogeneity between separate studies, and a fixed-effects model was used. Alternatively, if ≤1 and/or ≥50%, there was statistical heterogeneity between independent studies, and a random-effects model was used. Additional subgroups and sensitivity analyses were performed for factors that may cause heterogeneity.
3 RESULTS
3.1 Selection and inclusion of studies
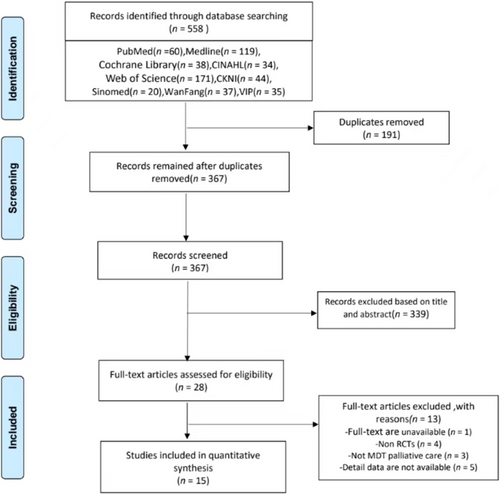
Of the 558 studies retrieved from the databases, 191 duplicates were identified and removed. Upon screening the titles and abstracts, another 339 studies were removed. The full texts were retrieved for the remaining 28 studies. Of these, 13 were removed due to various reasons (see Figure 1), resulting in 15 articles included in the meta-analysis.
3.2 Characteristics of the included studies
The 15 included studies11-25 were published between 2016 and 2022. These studies involved a total of 1850 cancer patients, including 925 in the experimental group and 912 in the control group. The basic characteristics of the included studies are shown in Table 1.
| Included study | MDT hospice pattern | Year of publication | Sample size (ex.) | Outcome metric | Measurement tools Path2 (Nursing work environment → Empathy → Caring behavior) | |
|---|---|---|---|---|---|---|
| Experimental group | Control group | |||||
| He Xing et al. | Nurse-led | 2017 | 40 | 40 | ①②④ | GQOLI-74, HAMD, NRSPath2 (Nursing work environment → Empathy → Caring behavior) |
| Ho Ke | Nurse-led | 2019 | 40 | 40 | ①②③ | Homemade Quality of Life Scale, SAS, SDSPath2 (Nursing work environment → Empathy → Caring behavior) Path2 (Nursing work environment → Empathy → Caring behavior) |
| Liu Yong et al. | Nurse-led | 2020 | 31 | 31 | ①③④ | QLQ-C30, HAMA, NRS |
| Liu Liang | Nurse-led | 2022 | 40 | 40 | ①②③ | GQOLI-74, SAS, SDS |
| Lu Hongmei et al. | Physician-led | 2022 | 341 | 341 | ①⑤ | QLQ-C30, comprehend the Social Support Scale |
| Zhang Li et al. | Nurse-led | 2022 | 50 | 50 | ① | QLQ-C30 |
| Li Jinna et al. | Physician-led | 2021 | 46 | 35 | ①④ | KPS, NRS |
| Shin Ji-ji et al. | Physician-led | 2020 | 55 | 55 | ①②③ | GQOLI-74, SAS, SDS |
| Sheep Wave et al. | Nurse-led | 2018 | 41 | 41 | ① | MQOL |
| Xie Jinqin | Nurse-led | 2018 | 50 | 50 | ①②③⑤ | SF-36, SAS, SDS, SSRS |
| Mengting Chen et al. | Physician-led | 2021 | 23 | 22 | ①②③④ | FACT-L, HADS, NRS |
| Joe Takatsuki | Physician-led | 2017 | 48 | 48 | ①②③ | SF-36, HADS |
| Wang Juan et al. | Physician-led | 2020 | 49 | 48 | ②③⑤ | ESAS, Patient Family Social Support Scale |
| Kim et al. | Physician-led | 2018 | 30 | 30 | ①④ | QLQ-C30, VAS |
| Malmstrom et al. | Physician-led | 2016 | 41 | 41 | ①④ | QLQ-C30, VAS |
- Note: ① Quality of life; ② depression; ③ anxiety; ④ pain; and ⑤ social support.
- Abbreviations: ESAS, Edmonton Symptom Assessment System; FACT-L, Functional Assessment of Cancer Therapy-Lung; GQOLI-74, Generic Quality of Life Inventory; HADS, Hospital Anxiety and Depression Scale; HAMA, Hamilton Anxiety Scale; HAMD, Hamilton Depression Scale; KPS, Karnofsky performance status; MQOL, McGill Quality of Life Questionnaire; NRS, Numerical Rating Scale; QLQ-C30, Quality of Life Questionnaire-Core 30; SAS, Self-rating Depression Scale; SDS, Self-report Depression Scale; SF-36, the MOS item short form health survey; SSRS, Social Support Rating Scale; VAS, Visual Analogue Scale.
3.3 Quality evaluation
All included studies were evaluated according to the Cochrane quality evaluation criteria.10 The results are shown in Table 2.
| RCTs | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other bias | Quality rating |
|---|---|---|---|---|---|---|---|---|
| He Xing et al. | High | Unclear | High | High | Low | Low | Low | B |
| He Ke et al. | Low | Unclear | High | High | Low | Low | High | B |
| Liu Yong et al. | Low | Unclear | High | High | Low | High | Unclear | B |
| Liu Liang | Low | Low | High | High | High | Low | Low | B |
| Lu Hongmei et al. | Low | Unclear | High | High | Low | Low | Low | B |
| Zhang Li et al. | Low | Unclear | High | High | Low | Low | Low | B |
| Li Jinna et al. | High | Unclear | High | High | Low | Low | Low | B |
| Shin Ji-ji et al. | Unclear | Unclear | High | High | Low | Low | Low | B |
| Sheep wave et al. | High | Unclear | High | High | Low | Low | Low | B |
| Xie Jinqin | Low | Low | High | High | Low | Low | Low | B |
| Chen Mengting et al. | Low | Unclear | High | High | Low | Low | Low | B |
| Joe Takatsuki | High | Unclear | High | High | Low | Low | Low | B |
| Wang Juan et al. | Low | Unclear | High | High | Low | Low | Low | B |
| Kim et al. | Low | Unclear | High | High | Low | Low | Low | B |
| Malmstrom et al. | Low | Unclear | High | High | Low | Low | Low | B |
3.4 Meta-analysis of outcomes
3.4.1 Effect of MDT hospice care on quality of life
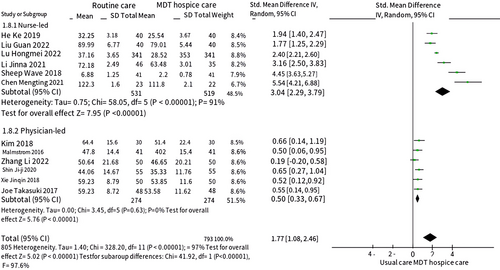
Twelve12, 14-22, 24, 25 of the 15 included studies compared the effect of MDT hospice care on quality of life for cancer patients, of which six were nurse-led and six were physician-led. Heterogeneity analysis revealed high heterogeneity among the six nurse-led studies12, 14, 15, 17, 19, 21 () but low heterogeneity among the six physician-led studies16, 18, 20, 22, 24, 25 (). The sensitivity analysis showed no obvious source of heterogeneity among nurse-led studies.Therefore, the random-effect model was used for both groups. The results showed that MDT hospice care improved quality of life for cancer patients more effectively than standard care () (Figure 2). The estimated effect size of nurse-led hospice care was greater than that of physician-led hospice care, indicating that a better effect of nurse-led MDT hospice care.
3.4.2 Effect of MDT hospice care on depression
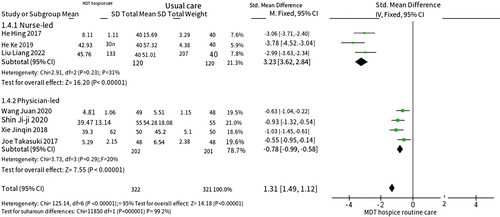
Seven studies11, 12, 14, 18, 20, 22, 23 evaluated the effect of MDT hospice care on depression among cancer patients, of which three were nurse-led and four were physician-led. As heterogeneity was low among the nurse-led11, 12, 14 () and physician-led studies18, 20, 22, 23 (), the fixed-effect model was used for the analysisThe results of the meta-analysis showed that physician-led MDT hospice care alleviated depression in cancer patients (). Nurse-led MDT hospice care also had a significant effect on alleviating depression in cancer patients (). The results showed a significant difference in the intervention effect between the MDT hospice care and standard care (), as shown in Figure 3, that is, MDT hospice care alleviated depression in cancer patients. The combined effect size of nurse-led MDT hospice care was further away from the ineffective line in the middle and had a larger estimated effect size than physician-led MDT hospice care, indicating that it had a better effect at alleviating depression in cancer patients.
3.4.3 Effect of MDT hospice care on anxiety
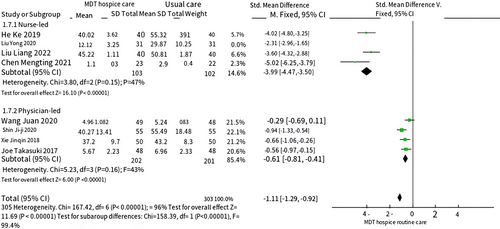
Eight studies12-14, 18, 20-23 compared the effects of MDT hospice care on anxiety among cancer patients, of which four were nurse-led and four were physician-led. The heterogeneity among the four nurse-led studies12-14, 21 was high (). However, there was no significant heterogeneity among the studies after removing the sources13 of heterogeneity identified by the sensitivity analysis (). As heterogeneity among the four physician-led studies18, 20, 22, 23 was low (), the fixed-effect model was used for the analysis. The meta-analysis results showed that physician-led MDT hospice care alleviated anxiety in cancer patients (). Nurse-led MDT hospice care also relieved anxiety in cancer patients The final combined effect size was statistically significant, that is, MDT hospice care significantly alleviated anxiety among cancer patients. The estimated effect size for nurse-led care was larger, indicating that its effect is greater than that of physician-led care (), as shown in Figure 4.
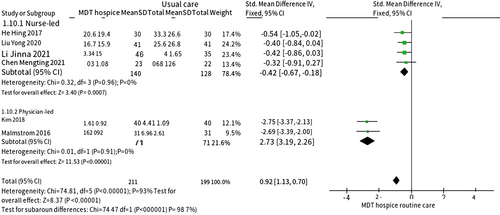
3.4.4 Effects of MDT hospice care on pain
Six studies11, 13, 17, 21, 24, 25 evaluated the effects of MDT hospice care on pain in cancer patients, of which four were nurse-led11, 13, 17, 21 () and two were physician-led24, 25 (). As both subgroups of studies had low heterogeneity, the fixed-effect model was used for the analysis. The meta-analysis results showed that physician-led MDT hospice care significantly relieved the pain of cancer patients (). Nurse-led MDT hospice care also relieved the pain of cancer patients (). The combined results were statistically significant (). While MDT hospice care can significantly relieve the pain of cancer patients, physician-led MDT hospice care had a greater estimated effect size, indicating that it provides greater control and relief of pain (Figure 5).
4 DISCUSSION
4.1 Methodological quality evaluation of included studies
All 15 studies included in this analysis were stochastic controlled experiments that met the inclusion and exclusion criteria. Among them, eight studies reported the generation method for the stochastic sequences and only one paper mentioned the stochastic grouping without giving a specific description of the grouping method. Only two studies described the implementation of distribution hiding. Due to the particularity of the intervention measures, not all studies could blind the patients and interveners. One study had incomplete data. There was a possibility of selective reporting bias in one study. One study had a certain subjective bias due to the use of self-made rating scales, which may affect the reliability of the conclusion. All studies were rated B for methodological quality and the overall literature quality was fair.
4.2 Effects of MDT hospice care in cancer patients
The results of this meta-analysis show that both nurse-led and physician-led MDT hospice care can effectively improve the quality of life for cancer patients, reduce negative emotions such as depression and anxiety, and relieve pain compared with conventional care. This result is consistent with that of a study by Rodin et al. Cancer patients not only suffer from physical pain, they also commonly face a large psychological burden and pressure. Research26 shows that 56%–57% of cancer patients have different degrees of psychological disorders, which can affect their quality of life. Compared with conventional care, MDT hospice care includes four unique aspects: death education, symptom care, life care, and psychological care. The multidisciplinary care team formulates a personalized plan according to each patient's condition, and provides them with comprehensive care and humanistic care services such as treatment and psychological counseling, to prevent or alleviate physical and psychological pain. This approach uses the complementary advantages of different disciplines to provide all-round care for the physical and mental well-being of cancer patients. As a result of the work of members of the multidisciplinary team, quality of life for cancer patients can been greatly improved and they are able to move through the final stages of life more calmly and peacefully.
4.3 Comparison of the effects between nurse-led and physician-led MDT hospice care
As shown by Figures 2-4, the effects of nurse-led and physician-led MDT hospice care differ in various metrics. Nurse-led MDT hospice care can better improve quality of life and alleviate depression and anxiety, while physician-led MDT hospice care has greater advantages for relieving physiological pain. The following sections discuss the possible reasons.
4.3.1 Roles and responsibilities
In a multidisciplinary hospice care team led by nurses, nurses are the main coordinators and act as a link to receive disease-related information from doctors and then pass it on to other members of the team. At the same time, nurses cooperate with other team members to assess a patient's psychological state, provide emotional support, and improve the quality of hospice care through communication. This makes patients feel more care.27 With physician-led hospice care, physicians are usually responsible for leading and guiding the hospice care team, formulating treatment plans, evaluating patients' conditions, and providing medical guidance and symptom management. However, physicians sometimes fail to address patients' humanistic needs and have less communication with patients, which may result in physicians ignoring patients' quality of life and emotional changes.28
4.3.2 Skills and training
Nurses and physicians differ in terms of their skills and training. The main components of hospice training for nurses include an overview of the hospice, pain management, symptom management, spiritual care, psychological care, communication, and grief care.29 Nurses can fully apply these skills in clinical practice to provide hospice care and understand patients' needs accurately in a timely manner, enabling them to consult with other members of the MDT hospice team to develop personalized plans so that patients' needs are met as fully as possible. In contrast, physician-led teams lack systematic training in hospice and related practical experience. Thus, they do not know how to provide psychological assistance to cancer patients, which is an important factor30 affecting the quality of hospice care.
4.3.3 Decision sharing
The imbalance of abilities and professional knowledge between physicians and patients hinders the implementation of shared decision-making. Many patients underestimate their ability to understand information, and doctors ignore patients' ability31 to obtain information. Therefore, in physician-led hospice care, it is difficult for patients to participate in medical decision-making. Thus, physicians play a more important role in making treatment plans and decisions. In nurse-led hospice care, nurses give priority to the patients' feelings, empower patients to participate in nursing decisions, and account for patients' personal decision-making preferences. Such shared decision-making can enhance nurse–patient communication and eliminate anxiety.32
4.3.4 Cancer pain management
At present, cancer pain education in China is relatively limited. Due to nurses' lack of understanding of cancer pain management and individual differences, patients' requirements33 cannot be met by relying solely on specialists. Physician-led hospice care is more effective at relieving pain for cancer patients, as it enables doctors to formulate individualized and standardized analgesic programs.
5 CONCLUSIONS
The findings of this meta-analysis suggest that MDT hospice care is superior to conventional care in improving quality of life, alleviating depression and anxiety, and relieving pain among cancer patients. However, differences in the composition of multidisciplinary teams can greatly affect hospice outcomes. In the subgroup analysis, the results showed that nurse-led MDT hospice care was more effective in some metrics than physician-led hospice care, although there was no significant effect in pain control. Due to the traditional Chinese values and concepts about “filial piety,” many patients and their families are reluctant to choose hospice care. Families are more willing to choose physician-led MDT hospice care over nurse-led MDT hospice care when they accept hospice care, because the public had stereotypes and bias on the role of nurses. Therefore, there is urgent need to promote nurse-led MDT hospice care. First, medical institutions, medical colleges, and academic organizations could regularly organize hospice-related activities, seminars, and knowledge popularization activities to improve public understanding and recognition of nurse-led hospice care. Second, the palliative care team needs to establish a long-term and sustainable relationship with each department to provide patients with a safer, more effective medical experience. Finally, relevant departments can develop policies and guidelines to support and promote nurse-led MDT hospice care, including improved supervision, training, financial support, and clarification of the roles and responsibilities of nurses in MDT hospice care.
In conclusion, it should be emphasized that nurses and physicians are indispensable members of MDT hospice care teams, whether they are nurse-led or physician-led. Good teamwork is essential for meeting the needs of patients and caregiver. MDT hospice care can help patients complete their last journey in life with dignity.
AUTHOR CONTRIBUTIONS
Yunrong Li: Conceptualization, formal analysis, writing original draft. Tiantian Wang: Conceptualization, formal analysis, writing original draft. Yi Zhang: Conceptualization, methodology, literature search, data extraction and interpretation. Yun Zhao: Conceptualization, formal analysis, writing review & editing. All authors were granted complete access to all the data in the study, with the corresponding author bearing the final responsibility for the decision to submit for publication. The corresponding author affirms that all listed authors fulfill the authorship criteria and that no others meeting the criteria have been omitted.
ACKNOWLEDGMENTS
This research was supported by the Elderly Health Research Program of Jiangsu Commission of Health (Grant/Award Number: LK2021012).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
The Ethics Committee of the Jiangsu Cancer Hospital approved this study.




