Primary central nervous system lymphoblastic B cell lymphoma located at cerebellum in a child: A case report and literature review
ABSTRACT
Introduction
Primary central nervous system lymphoma (PCNSL) is extremely rare in pediatric population. We reported a case of PCNSL in a 3-year-old girl and reviewed the literature in the past three decades.
Case presentation
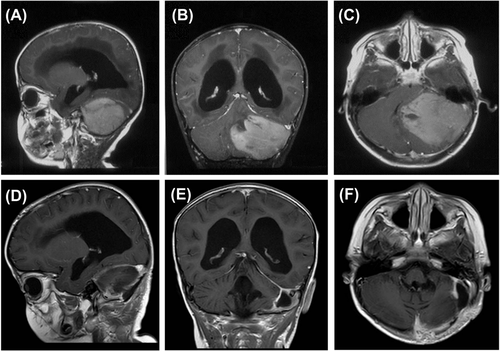
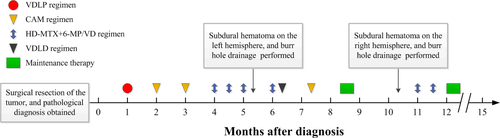
A 3-year-old girl presented with gait disturbance. A contrast-enhanced magnetic resonance image of the brain showed a solitary bulky mass in the left cerebellar hemisphere, hydrocephalus and cerebellar tonsillar hernia. Surgical resection was performed and the patient was diagnosed with primary central nervous system lymphoblastic B cell lymphoma. Then the patient received regular chemotherapy, including 6 cycles of chemotherapy containing high-dose methotrexate (HD-MTX). The patient remains alive 15 months after the diagnosis with no evidence of active disease, but suffered twice chronic subdural hematoma, which was treated by burr hole drainage.
Conclusion
Lymphoblastic B cell lymphoma is a rare histologic subtype of pediatric PCNSL. Chemotherapy containing HD-MTX remains the most effective treatment. The patient should avoid head impact after surgical resection of the tumor to prevent chronic subdural hematoma.
1 INTRODUCTION
Primary central nervous system lymphoma (PCNSL) is an aggressive form of non-Hodgkin’s lymphoma (NHL) that is confined to brain, leptomeninges, eyes, or spinal cord. PCNSL can affect all age groups with a median age in the sixth decade.1 However, PCNSL is an extremely rare tumor in the pediatric population, with case reports and case series describing approximately 200 cases over the past three decades.2-6 Histologically, the most common subtype of PCNSL is diffuse large B-cell lymphoma (DLBCL). Lymphoblastic lymphoma is an extremely uncommon histologic subtype of PCNSL both in adults and children. Here, we presented a case of primary central nervous system (PCNS) lymphoblastic B cell lymphoma located at cerebellum in a child, who underwent surgical resection and chemotherapy treatment but suffered twice chronic subdural hematoma (SDH). To our knowledge, this is the first pediatric PCNSL case of this histologic subtype occurring in cerebellum region, and the first report of repeated chronic SDH associated with PCNSL. We describe our treatment procedure and the outcome achieved.
2 CASE REPORT
A previously healthy 3-year-old girl presented with slowly progressive gait disturbance for one month and was admitted to the local hospital. A contrast-enhanced magnetic resonance image (MRI) of the brain showed a solitary bulky mass (6.6 cm × 6.6 cm × 5.3 cm) in the left cerebellar hemisphere with intense contrast enhancement, hydrocephalus and cerebellar tonsillar hernia (Figure 1A–C). The patient immediately underwent gross total excision of the tumor and extraventricular drainage. Microscopically, tumor cells were middle in size and infiltrated the cerebellar parenchyma with a scattered or perivascular growth pattern. Immunohistochemical staining indicated lymphoblastic B cell lymphoma.
Then, the patient was referred to our hospital. Pathology center review showed that the tumor cells were immunopositive for CD 19, CD79a, PAX 5 (B-Cell markers) and TDT (immaturity marker) while negative for CD3, CD4, CD5 (T-Cell marker). Fluorescence in situ hybridization did not reveal C-MYC translocation, and the screening of Philadelphia-like genes was negative. The spine MRI, cerebrospinal fluid flow cytometry and ophthalmologic examination were normal. The bone marrow biopsy and a whole-body PET/CT scan failed to demonstrate neoplasia elsewhere. Immunoglobulin levels and absolute number of T lymphocyte were normal. The tests of human immunodeficiency virus, Epstein-Barr virus and hepatitis B virus were negative. Accordingly, a diagnosis of PCNS-lymphoblastic B cell lymphoma in an immunocompetent child was established.
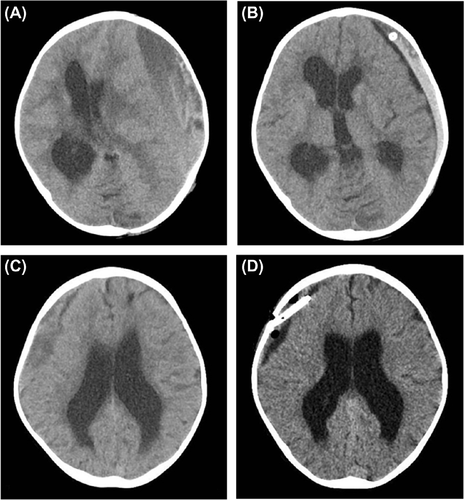
Six weeks after operation, the intracranial lesion recovered well (Figure 1D–F) without neurological symptoms, and the patient received systemic chemotherapy by Berlin-Frankfurt-Munster (BFM) 95 revised protocol (the regimens are shown in Figure 2). However, after 6 cycles of chemotherapy, the patient was referred to the emergency room due to acute altered bradycardia and poor mental response. Computed tomography (CT) scan of the head revealed a large left chronic SDH with midline shift and herniation and no skull fracture was detected (Figure 3A). Burr hole drainage was performed immediately and a subcutaneous drain was placed. After 24 hours, CT scan showed that the volume of hematoma decreased significantly (Figure 3B). The subcutaneous drain was taken out 3 days later. After three weeks of the burr hole drainage, the patient recovered completely and continued three cycles of chemotherapy and entered maintenance therapy. Unfortunately, chronic SDH of the right hemisphere was found by the routine head CT examination (Figure 3C), but the patient remained asymptomatic. Burr hole drainage was performed again, and CT scan showed the volume of hematoma decreased obviously after 24 hours of the surgery (Figure 3D). No malignant cell was found by the cytological examination of drainage fluid. The postoperative course was uneventful, and the patient continued another 2 cycles of high-dose methotrexate (HD-MTX) chemotherapy and entered maintenance therapy. In addition, the patient received 14 cycles of intrathecal chemotherapy, including methotrexate, cytarabine and dexamethasone. After follow-up of 15 months, the patient is still under maintenance therapy with no evidence of relapse of the lymphoma. Moreover, the patient grows well with normal gait.
3 DISCUSSION
Compared with adults, pediatric cancers are rare; each year, they affect 50 to 200 children per million worldwide.7 Brain tumor and NHL represent the second and the third most common malignancy among pediatric population, respectively. However, PCNSL is an extremely rare tumor in children. In a 40-year analysis (from 1973 to 2013), SEER (Surveillance, Epidemiology, and End Results) database found 103 (1.5%) PCNSL patients younger than 19 years of age among 6 765 PCNSL patients of all ages.1 From 19 027 PCNSL patients reported to CBTRUS (Central Brain Tumor Registry of the United States) in 14-year period (from 2000 to 2013), only 189 (1%) pediatric cases younger than 19 years of age was identified.1 In Asian countries, among 596 PCNSL cases enrolled in Brain Tumor Registry of Japan from 1969 to 1990, nine pediatric cases (1.5%) were documented.8
A multicenter study of BFM group, in the 3740 pediatric patients with NHL, only 17 patients (0.45%) were identified as PCNSL.3 Children’s Oncology Group reported that Burkitt lymphoma, DLBCL, lymphoblastic lymphoma, and anaplastic large cell lymphoma represented the most NHL (93%) in pediatric patients, and the remainder of 7% was considered as the rare pediatric NHLs; moreover, PCNSL accounted for 3.5% of the rare pediatric NHLs.9 Based on these data, pediatric PCNSL tends to account for 1%–1.5% of all PCNSLs and 0.4% of all pediatric NHLs.
In adults, the majority (> 90%) of PCNSL have histology of DLBCL. However, the incidence of this subtype in children is much lower, ranging from 30% to 70%. The largest series of 75 pediatric PCNSL patients by a multicenter study showed that the most common subtype was DLBCL (49.3%), followed by anaplastic large T-cell lymphoma (22.7%), Burkitt lymphoma (12%), B-NHL not otherwise specified (6.7%), B-cell precursor lymphoblastic lymphoma (5.3%) and other subtypes (4%).10 After review of the literature in the past three decades, we identified only 6 cases of PCNS-lymphoblastic B cell lymphoma reported in childhood (Table 1).10-12 Clinical information was available in 5 patients, all of whom were immunocompetent with a median age of 9.75 years (range, 8.11–18.00 years). All patients were alive at the time that the cases were reported with a median follow-up of 3.39 years (range, 0.19–9.00 years). In terms of tumor location, two patients had tumors located in leptomeninges; three patients had tumors involved the brain parenchyma (one in occipital lobe, and the exact sites were not mentioned in the other two cases). To our knowledge, the patient we presented is the first pediatric case of this histologic subtype located at cerebellum region.
| Study |
Age (years) |
Sex | Tumor site | Immune status | Treatment | Outcome |
Follow-up (years) |
|---|---|---|---|---|---|---|---|
| Attarbaschi et al10 | 11.41 | F | Brain parenchyma† | Immunocompetent | MTX-based Chemo + RT | Alive | 5.62 |
| 8.11 | M | Leptomeninges | Immunocompetent | MTX-based Chemo | Alive | 0.19 | |
| 9.75 | M | Brain parenchyma† | Immunocompetent | MTX-based Chemo + RT | Alive | 9.00 | |
| 18.00 | F | Leptomeninges | Immunocompetent | MTX-based Chemo + RT | Alive | 3.39 | |
| Abla et al11 | NM | NM | NM | NM | NM | NM | NM |
| Shiozawa et al12 | 9.00 | M | Occipital lobe | Immunocompetent | MTX+Ara-C-based Chemo + RT | Alive | 1.83 |
- F, female; M, male; MTX, methotrexate; Chemo, chemotherapy; RT, radiation treatment; NM, not mentioned; Ara-C, cytarabine. †The exact site not mentioned.
MRI with gadolinium contrast is the most sensitive radiographic method for the diagnosis of PCNSL, which is characterized by homogeneous contrast enhancement with well-defined borders. Stereotactic needle biopsy is recommended when PCNSL is suspected by MRI. Surgical resection is not part of the standard treatment for PCNSL because of the multifocal nature of this tumor and high complication rates after surgery. But surgical resection can be performed for symptomatic relief of severe mass effect. Given the serious neurotoxicity and the short duration of remission, whole brain radiotherapy is considered as the consolidation therapy after induction remission or the salvage treatment for relapsed/refractory patients. Hence, the current standard diagnosis and treatment for newly diagnosed PCNSL involves stereotactic brain biopsy for pathological diagnosis followed by systemic HD-MTX-based chemotherapy.
In adults, HD-MTX-based chemotherapy has become the standard treatment for PCNSL patients. However, the optimal treatment for PCNSL in children has not been established. In a few case series studies of pediatric PCNSL, a wide variety of treatment modalities have been used, including surgical resection, radiation, chemotherapy or the combination of these regimens. In the largest series study of pediatric PCNSL (n = 75), 58 patients (77%) were treated with NHL-subtype protocols, and 17 patients (23%) received miscellaneous therapies; the chemotherapeutic cycles included HD-MTX in 68 patients (91%), and there was an independently significant relationship between chemotherapy containing HD-MTX and longer event-free survival (EFS); the 5-year EFS and overall survival (OS) of the entire cohort were 74% and 85%, respectively.10 Similar outcomes were obtained in a smaller series (n = 29) by International Primary CNS Lymphoma Collaborative Group (IPCG), which showed that the 3-year OS was 82% and higher dose of MTX was significantly associated with higher response rate.11 The BFM group reported 17 pediatric PCNSLs treated with BFM protocols, which included HD-MTX, high-dose cytarabine, and triple intrathecal chemotherapy; with a median follow-up of 7.5 years, and the 3-year OS in the entire cohort was 63%.3 From these results, we found that the prognosis of pediatric PCNSL appears to be much better than that in adults, which reported a 5-year survival rate of 30%.13 In addition, HD-MTX-based chemotherapy should be recommended in pediatric PCNSL.
In our case, because of initial cerebral hernia, surgical resection was performed to reduce intracranial pressure and obtain pathologic diagnosis. Then the patient received regular chemotherapy, including 6 cycles of chemotherapy containing HD-MTX. Regular contrast-enhanced MRI of brain and cerebrospinal fluid examination showed no evidence of relapse. However, the patient suffered twice chronic SDH during the treatment. As we know, SDH often occurs in children younger than 2 years of age and elderly alcoholics, and the most common reason is the traumatic injury. In the present case, the patient unintentionally experienced slight head impact while playing games. Besides, the patient initially presented with hydrocephalus; after hydrocephalus absorption, the intracranial pressure decreased rapidly and intracranial space increased obviously. In this circumstance, even under a slight external force, the brain parenchyma continued to move due to inertial force, which caused the pulling and rupture of subdural blood vessels. Notably, Jankowski et al14 reported a 13-year-old boy with PCNSL received chemotherapy treatment more than one year but suffered a right sided basal ganglia hemorrhage following a concussion while playing football; unfortunately, 6 months post-injury he presented with asymptomatic lymphoma recurrence. Thus, the avoidance of any degree of head impact in this population is recommended, and the possibility of short-term relapse after intracranial hemorrhage should be alerted.
Lymphoblastic B cell lymphoma is a rare histologic subtype of pediatric PCNSL, with only 6 cases reported over the past three decades. We reported an immunocompetent pediatric PCNS-lymphoblastic B cell lymphoma located at cerebellum region. The patient underwent surgical resection of the total tumor followed by regular system chemotherapy and intrathecal chemotherapy, without brain radiation. During the treatment, the patient suffered twice chronic SDH, which were treated by burr hole drainage. A multicenter collaboration should be performed to understand the clinical features and prognosis of this rare disease.
CONSENT FOR PUBLICATION
Informed consent was obtained from the patient’s guardians.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.