Outcomes of surgery for epiblepharon accompanied with lower eyelid retraction secondary to buphthalmos in children
ABSTRACT
Importance
In cases of epiblepharon with lower eyelid retraction secondary to glaucoma, correcting epiblepharon alone is ineffective. Combined surgery should be performed to obtain satisfactory outcomes.
Objective
To investigate outcomes after surgery to correct epiblepharon with lower eyelid retraction secondary to buphthalmos in children.
Methods
A retrospective analysis of six eyes in four patients was performed included lower lid retractor recession combined with marginal rotation with tarsal fixation. The margin reflex distance-2, lagophthalmus, resolution of clinical symptoms, and complications were assessed during 6 to 12 months of follow-up.
Results
In all cases, epiblepharon and lagophthalmus were corrected, symptoms of photophobia and epiphora were relieved, and the corneal epithelium was repaired. The margin reflex distance-2 decreased and remained normal during the follow-up period, but slightly regressed within 6 months postoperatively.
Interpretation
Epiblepharon caused by buphthalmos in children is often associated with lower eyelid retraction. Lower lid retractor recession combined with marginal rotation with tarsal fixation fundamentally solves the problems of high eyelid tension, lower eyelid retraction, and epiblepharon and reduces the recurrence rate.
1 INTRODUCTION
Epiblepharon is a common disease in pediatric ophthalmology. In rare cases, epiblepharon can be accompanied by lower eyelid retraction characterized by an inferiorly displaced lower eyelid and exposed sclera between the lower corneal limbus and the eyelid margin. Lower eyelid retraction is typically caused by thyroid eye disease, glaucoma, vertical rectus muscle recession or facial nerve paralysis. Exposure of the ocular surface and eyelash friction can cause symptoms of irritation, photophobia, epiphora, conjunctival congestion, and even vision-threatening corneal decompensation.1, 2
Surgical treatment is indicated for epiblepharon with symptoms that not relieved by medical treatment, including topical lubrication and corneal epithelial repair. The choice of surgical technique is based on the shape of the epiblepharon and the degree of symptoms.2-4 In cases caused by glaucomatous eyeball dilation, the effects of eyelash friction and glaucoma lead to more severe corneal damage and more significant ocular irritation. Dilation of the cornea may make the presence of lower eyelid retraction evident, resulting in a diagnosis as of simple epiblepharon that is treated with routine epiblepharon correction. However, we find that correcting epiblepharon alone is ineffective in these patients and the condition often recurs.
Previous studies have reported outcomes of surgery for lower eyelid retraction or epiblepharon,2, 4 however, few studies have on the efficacy of surgery in cases secondary to buphthalmos in children. Therefore, this study was conducted to evaluate the effect of a surgical procedure in children with epiblepharon and concurrent lower eyelid retraction secondary to buphthalmos.
2 METHODS
2.1 Ethical approval
The study was approved by the Beijing Children’s Hospital Ethics Committee (2020-Z-171) and conducted in accordance with the Declaration of Helsinki. Informed consent was exempted.
2.2 Patients
We retrospectively reviewed the medical records of four consecutive patients who were diagnosed with epiblepharon with concurrent lower eyelid retraction secondary to buphthalmos from December 2017 to December 2018 in the Department of Ophthalmology, Beijing Children’s Hospital.
Patients with buphthalmos, epiblepharon, and lower eyelid retraction and with stable intraocular pressure and axial length for more than 6 months, were included in the study. Patients with epiblepharon and lower eyelid retraction but without a history of glaucoma, and those with unstable intraocular pressure or axial length during the prior 6 months were excluded from the study. All patients underwent a complete eye examination, including visual acuity, intraocular pressure, slit lamp examination, corneal diameter and axial length measurement, and fundus examination. To compare preoperative and postoperative conditions, facial photographs of the patients were taken, and the pre- and postoperative margin reflex distance-2 (MRD2) and amount of lagophthalmus were recorded. Resolution of clinical symptoms was also assessed, as were complications. All measurements were performed by three independent observers, and the average of the obtained values was used for analysis.
2.3 Surgical technique
All surgeries were performed by the same ophthalmologist (W.Q.). Under general anesthesia, patients were assessed for epiblepharon and lagophthalmus with lower eyelid retraction (Figure 1A–1C). A subciliary incision was made on the lower lid 1 to 2 mm below the lash line. The anterior lamella was dissected to the lower border of the tarsus, exposing the lower lid retractors. The lower lid retractors were then disinserted and 10 to 15 mm was excised until the lower eyelid margin rose to a position 1 to 2 mm below the pupil center (Figure 1D–1F). The retractor was then fixed to the inferior conjunctiva fornix. Epiblepharonwas corrected by fixing the upper edge of the incision to the tarsus with 6/0-Vicryl suture. The skin was closed in a continuous pattern with 7-0 silk thread (Figure 1G–1I). A Frost suture was used to prevent tissue adhesion. At the end of surgery, the position and contour of the eyelid margin were satisfactory (Figure 1J–1K). Tobramycin and dexamethasone eye ointments were applied in the conjunctival sac, and a bandage dressing was placed for 48 to 72 hours.

3 RESULTS
A total of four patients (six eyelids) who met the eligibility criteria were finally enrolled, including 3 boys and 1 girl. The mean age of the participants was 3.5 years (range: 1.3–4.5 years). The postoperative follow-up duration was 8.3 months (range: 6–12 months). Two of the patients (cases 1 and 4) had undergone routine epiblepharon correction two or three times previously; the condition had recurred in each case within 3 months postoperatively.
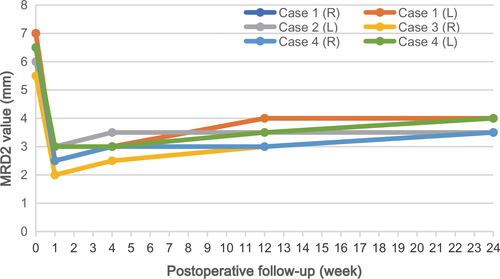
The mean preoperative corneal diameter and axial length were 13.9 mm (13.1–15.1 mm) and 27.1 mm (23.3–29.9 mm), respectively (Table 1). All eyes showed improvement in lower eyelid elevation and decreased MRD2 at the last visit (Figure 2). MRD2 decreased from a mean of 6.4 mm (5.5–7.0 mm) preoperatively to 3.8 mm (3.5–4.0 mm) at the last visit. However, MRD2 increased gradually over time and remained in a stable state of approximately 4.0 mm after 6 months postoperatively (Figure 3). The mean lagophthalmos decreased from 3.5 mm (2.0–4.0 mm) preoperatively to 0.3 mm (0–1.0 mm) postoperatively. There was no significant recurrence of lower eyelid retraction or epiblepharon during the follow-up period.
| Case | Sex | Age (years) | Primary disease | Side | Follow-up (months) | History of epiblepharon surgery | CED | CD (mm) | AXL (mm) | MRD2 (mm) | Lagophthalmus (mm) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Embedding | Skin excision | Pre-operative | Final | Pre-operative | Final | |||||||||
| 1 | M | 4.5 | CG | Right | 12 | 2 | 1 | ++++ | 15.0 | 29.9 | 7.0 | 4.0 | 4.0 | 0 |
| Left | 12 | 2 | 1 | ++++ | 15.0 | 28.9 | 7.0 | 4.0 | 4.0 | 0 | ||||
| 2 | M | 4.2 | CG | Left | 8 | 0 | 0 | ++++ | 14.0 | 26.9 | 6.0 | 4.0 | 3.0 | 0 |
| 3 | F | 1.3 | SWS | Right | 6 | 0 | 0 | +++ | 13.0 | 23.3 | 5.5 | 3.5 | 2.0 | 0 |
| 4 | M | 3.8 | CG | Right | 6 | 1 | 1 | ++++ | 13.5 | 26.9 | 6.5 | 3.5 | 4.0 | 1.0 |
| Left | 6 | 1 | 1 | ++++ | 13.0 | 26.6 | 6.5 | 4.0 | 4.0 | 1.0 | ||||
- AXL, axial length; CD, corneal diameter; CED, corneal epithelial defect; MRD2, margin reflex distance-2; CG, congenital glaucoma; SWS, Sturge Weber syndrome

All six eyes of the four patients showed improvement or resolution of the following clinical symptoms: ocular burning/itching, dryness, photophobia, epiphora, pain, and unsatisfactory eyelid appearance. No patient had obvious lagophthalmus, epiblepharon or corneal epithelial defects postoperatively. No complications, including infection, inflammation, incision dehiscence and ectropion, were observed during the follow-up period, except for bleeding or hematoma in the early postoperative period, which occurred in two eyes, and improved after pressure bandaging.
4 DISCUSSION
Epiblepharon is a common disease in children that can be caused by lower eyelid retraction in rare cases. Lower eyelid retraction is relatively rare in children compared with adults, with an incidence of approximately 0.4/100 000. Olayanju et al1 reported that childhood eyelid retraction occurred in 1 out of every 72 463 individuals younger than 19 years of age in Olmsted County, MN, USA, and that lower eyelid retraction accounted for 29% of all cases. Etiologies of pediatric lower eyelid retraction include thyroid eye disease, primary congenital eyelid laxity, congenital glaucoma, high myopia and other rare causes.2-6 This study describes four pediatric patients (six eyes) with lower eyelid retraction who exhibited buphthalmos, including one eye with secondary glaucoma caused by Sturge-Weber syndrome.
The position of the lower eyelid is maintained by the lower eyelid retractor, tension of the lower eyelid, location of the canthal ligament, degree of eyeball protrusion and adequacy of the conjunctivae. The lower eyelid retractor is of the capsulopalpebral fascia and inferior tarsal muscle. This structure, along with the orbital septum, plays an important role in maintaining the eyelid margin in its normal position by drawing the lower eyelid backward and downward, causing the lower eyelid to closely contact the eyeball surface and maintaining the proper tension of the lower eyelid. In cases of infantile glaucoma, long-term elevated intraocular pressure leads to gradual expansion of the eyeball, resulting in degeneration and shortening of the posterior lamella of the lower eyelid.4, 7, 8 In this study, the average axial length was 27.1 mm and the mean corneal diameter was 13.9 mm; these are significantly larger than normal values in children. Continuous downward traction of the lower eyelid retractor, tension of the eyelid skin and long-term prominent compression of the eyeball result in epiblepharon.
MRD2 is an important index to evaluate the degree of lower eyelid retraction.2, 9 The degree of retraction is categorized as mild if the lower eyelid asymmetry is less than 2.0 mm and if the MRD2 is less than 6.5 mm for both lower eyelids. If values exceed limits, the degree of retraction is categorized as severe.2 In this study, the mean preoperative MRD2 was 6.4 mm, with all cases categorized as moderate to severe. In glaucomatous patients, dilation of the cornea influences scleral exposure, which thus cannot be used as an indicator of lower eyelid retraction. Lagophthalmus can also be used as an indicator of lower eyelid retraction, makes the description of degree of the eyelid retraction more objective and direct.
Epiblepharon can be corrected by embedding or skin excision. However, in cases caused by glaucoma, this treatment can not only relieve lower eyelid retraction but can also increase the tension of the lower eyelid skin and muscle. Repeated operations can cause scar contracture, which further aggravates the degree of retraction.5, 10 In this study, two patients (four eyes) underwent a total of 10 epiblepharon corrections, with recurrence after each procedure. Considering the etiology and pathological changes, we chose a combined operation to achieve correction of lower eyelid retraction and epiblepharon to release tension of the lower eyelid, move the lower eyelid edge forward, correct the lower eyelid retraction, and then externally rotate the palpebral margin.
The selection of surgical techniques to correct lower eyelid retraction is based on the causes and degrees of retraction. Lower eyelid retractor recession alone or combined with a lateral tarsal strip procedure (for lateral canthal tightening) is often effective in mild-to-moderate lower eyelid retraction.8, 11 In severe cases, spacer grafts are often used to push the lower eyelid margin upwards and to prevent it from dropping.12-15 Spacer materials include autografts such as hard-palate mucosa and ear cartilage; allografts including preserved dermis (AlloDerm®, Surederm®) and sclera; and synthetic grafts including polytetrafluoroethylene (Gore-Tex) and porous polyethylene (Medpor).16-20 Considering the ethical problems and probable graft rejection in children, we adopted the technique of lower eyelid retractor recession without grafting even in severe cases.
There are several points to be aware of during the operation, including the depth of general anesthesia, which can affect the position of the eyelid and eyeball. The lower eyelid retractor should be completely separated, and fixed in the deep part of the conjunctival fornix to prevent long-term muscle reduction. The “superfluous” skin of the lower eyelid results from retraction; therefore, skin excision should be avoided. After resetting of the lower eyelid, tarsus inner fixation should be performed to correct the direction of the palpebral margin. A Frost suture is needed to prevent early retraction of the lower eyelid resulting from inflammation, gravity, or muscle reduction. The eyelid position should be overcorrected by 2 to 3 mm at the end of the operation, in consideration of the regression phenomenon. Postoperative intraocular pressure should be controlled to avoid recurrence of lower eyelid retraction. In this study, the overcorrection of eyelid position decreased gradually and remained stable 6 months postoperatively, as shown in Figure 2; this effect was also indicated by the change in MRD2 (Table 1 and Figure 3). The cosmetic effect was satisfactory, and MRD2 remained within the normal range (approximately 4 mm) until the last visit, with good eyelid closure, no recurrence of epiblepharon, repair of the corneal epithelium, and improvement or disappearance of irritation symptoms.
This study introduced a combined surgery of lower eyelid retractor recession and marginal rotation with tarsal fixation, which fundamentally solves the problems of high eyelid tension, lower eyelid retraction, and epiblepharon caused by eyeball enlargement, with low surgical recurrence and complications. However, study had several limitations, including low number of cases and short observation times. Thus, further studies with a larger sample size and longer follow-up period are needed to determine the long-term outcomes of the operation more objectively.
CONFLICT OF INTEREST
None.