Leveraging real-time data to drive quality improvement in a pediatric health system
Abstract
We are inundated by data; healthcare is no different. The electronic medical record, the numerous patient care monitors, and the thousands of medications to be reconciled with specific dosing parameters are a few examples of the omnipresent and intimidating nature of data in healthcare. Across the world, healthcare without data does not exist. The data represent many forms but are quickly moving towards electronic formats. As ubiquitous as data are the near universal finding that such data are lagging. There is an urgent need for real-time data in improving processes and ultimately outcomes in healthcare. If data lag by four to eight weeks, if not longer, then true change cannot occur and harm continues in that interval. This review article discusses the urgent need for real-time data and demonstrates examples of how Children's National Medical Center in Washington, DC uses real-time data to drive outcomes.
Introduction
Children's National Medical Center is a tertiary care, free-standing pediatric healthcare system in Washington, DC, United States of America. Our hospital has served the region and the country for nearly 150 years. This time period spans the era of modern medicine and as such, there have been tremendous changes and advancements in healthcare and healthcare delivery during these times particularly in the past couple of decades. One of the areas with the most rapid and voluminous change has been in the sheer amount of data that exists in healthcare.1 Terminology that is in vogue at present is “big data”, which speaks to the inundation of almost every industry with an unprecedented amount of data. These data can be life-saving and allow for novel analytical approaches. It is important to delineate that big data does not necessarily mean a large volume, rather it is best thought of to be a full data set where the sample size (N) is all of the data points.1
Just as data have evolved, quality improvement has also blossomed in the last quarter century. The science of quality improvement is now embedded into American healthcare culture. Hospitals and health systems track and report publically on their outcomes; indeed, this is occurring across the world as well. Improvement scientists rely on data and use data to drive problem identification and resolution. Traditionally, data for improvement science (quality improvement) has been lagging data. In other words, for process improvement in healthcare, the data that is used is at best a few weeks old. Of course, this is where we have evolved to and need to accelerate evolving past this threshold. There still exist major national and international healthcare collaboratives in which the data lags by six months or more. When participating in quality improvement collaboratives to improve a metric (for example, length of stay), the data used for benchmarking can be six to nine months old.
A 2016 estimate suggested that the amount of digital data is set to exceed 1 zettabyte, which is 30 million times the data in all books that have ever been written.2 Healthcare accounts for more than 30 percent of this data.3 McKinsey Corporation estimates that healthcare data has potential of saving the United States more than $300 billion with optimized, data-driven decision making and clinical pathways.4 Despite plethora of data, healthcare organizations struggle to make data-driven real-time decisions. The United States’ healthcare data systems have been transforming in the last twenty years, and it is in-part due to the increased usage of electronic health records (EHR).5 The Institute of Medicine Committee on Quality of Healthcare in America stressed the importance of information technology in transforming American healthcare into a “safe, patient-centered, and effective enterprise.6” According to the Institute, there are several core criteria for functionalities of EHR system: 1) EHR should improve patient safety; 2) efficiency; 3) support effective patient care delivery; 4) addresses management of chronic conditions, and 5) should be feasible to implement. Ferranti and colleagues argue that it is essential to have a “more thoughtful and systematic approach” to Health Information Technology services research. Robust usage of EHR requires “timely, relevant and actionable information” for all users.5 Several studies have been published on the topic of EHR-triggers utilized in reducing harm outcomes, such as nephrotoxic kidney injury7 sepsis.8 EHR has also been utilized to leverage an automated system for real-time medication administration error.9 On the contrary, real-time measures of nationally-reported harm are lagging indicators.
The National Healthcare Safety Network (NHSN) is an agency within the Centers for Disease Control and Prevention, and it is the most widely used system for tracking hospital acquired infections. NHSN enables facilities to keep track of various process measures, such as vaccine status and rates infection control practice adherence, such as hand-hygiene compliance. Facilities utilize NHSN data to identify infection trends and benchmark these data to state and federal level. With over 17 000 medical facilities NHSN facilitates a nationwide effort to reduce hospital acquired infections. NHSN data, albeit powerful, are lagging indicators sometimes months later. For example, the Central Line-Associated Bloodstream Infection event data for Quarter 1, which covers January–March, is due to NHSN by August 15. This means events in January could not be analyzed and trended for close to five months.
Solutions for Patient Safety (SPS) is a network of more than 130 Children's Hospitals to reduce hospital acquired and other harm conditions. In addition to NHSN-reported hospital acquired infections, SPS tracks outcomes in pressure injuries, venous thromboembolism, unplanned extubations, peripheral intravenous infiltration and extravasations, Adverse Drug Events, fall-injuries, and employee and staff safety. SPS data deadline is two calendar months after the event month. This means events in January are not reported and trended until March. SPS also tracks process measures such as compliance to evidence-based care bundles that are known to reduce hospital acquired conditions. For this data submission, tracking and managing process data in hospital-level are left to organizations. However, organizations often struggle to manage these datasets and rely primarily on reported lagging data. Bundle compliances are leading indicators, and hospitals miss crucial opportunities for improvement if they have delayed reactions to performance measures, resulting in improvement work with extremely long cycle times.
The National Surgical Quality Improvement Program (NSQIP) is one of the most successful platforms to demonstrate improvement on a macro level from individual hospital data. This platform from the American College of Surgeons uses a sophisticated sampling methodology to have hospitals enter hundreds of variables on index cases. There is no more impactful platform for surgical care that has demonstrated success in improving care, as NSQIP programs saw a 47% reduction in 30-day postoperative mortality and a 42% reduction in 30-day postoperative morbidity.10 NSQIP provides hospital-level comparative data, but lags by approximately six months.10
Hospital acquired conditions
At Children's National, we have adopted a version of the harm index, which was initially published by Nationwide Children's Hospital in Columbus, OH.11 The harm indexis an aggregate representation of the incidence of specific hospital conditions, and displays the actual incidence of events in an easy to interpret format. For example if there were five unplanned extubations in the month of May, this would be represented as “5” on the harm index. In many other presentations, this value of 5 is divided by the number of ventilator days or other such denominators to obtain a rate. Nationwide Children's and others have demonstrated significant reduction in harm for hospital acquired conditions with a visualization tool such as a harm index.11
In 2013–2014, Children's National health system made a programmatic commitment and approach to quality and safety with the re-alignment of previous disparate quality and safety functions under a consolidated leadership structure of a Chief Quality and Safety Officer. Shortly after this time, the organization adopted our version of the preventable harm index and branded this internally as our “Zero Harm Index”. The Zero Harm Index is shown several times a week to different audiences in our organization from the front-line to executive leadership and even to our Board.
There is dynamic tension from having the data perfectly correct and having it real-time.1 We made the strategic decision that real-time data was more important than always having the data 100% accurate. What this means is that we are willing to put a caveat with the Zero Harm Index that it may change. Building on the example of the unplanned extubations, in our example there were 5 listed in the month of May 2018. We reserve the right, and the organization understands that we may change this to 4 or 6 a few weeks later once the month has closed out and we have completed our data attribution and verification. The alternative to messy data is to wait two months until all the data has been reconciled and then report this out on the Zero Harm Index; however, this data is not actionable by that time.
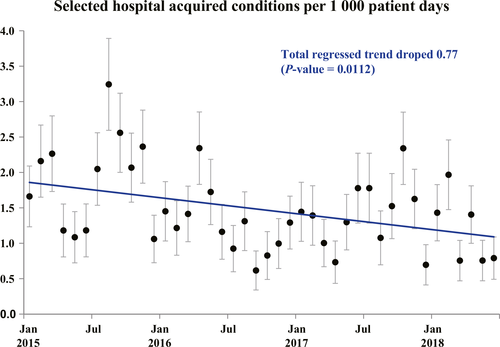
As demonstrated by Figure 1, we have seen a significant decrease in the actual number of events over the past several years. To demonstrate direct casualty from implementation of real-time monitoring of our hospital acquired conditions (HAC) and this decrease is impossible. However, the tactical approach to be cognizant and aware of all issues continuously most certainly allows our leadership team to be agile and respond. In addition to leadership being continuously aware of all potential issues, we also ensured that the front-line are immediately and continuously aware of issues, especially hospital acquired conditions.12 In building the real-time approach towards hospital acquired conditions, we utilized existing software (SharePoint) that is accessible to all levels of staff in the organization. Using this platform allowed us to centralize our data collection and visualization. The expectation is that the hospital provides the platform via SharePoint, but the clinical leaders are expected to enter the data in real-time. For example, if a clinical team identifies a venous thrombo-embolus, then the expectation is that they access the SharePoint site and enter the clinical data. The downstream implication of entering data real-time is that we can drill down to the micro-unit level and track and trend data.
The implicit understanding herein is that if data lags by months, then none of the aforementioned strategies are effective nor can even be implemented. As the Chief Quality and Safety Officer, the senior author has effectively utilized this real-time data to immediately impact changes. The Zero Harm Index is embedded on his laptop and the data is viewed on a near continuous basis allowing for early and immediate identification of potential issues.
Infection control and prevention
We have taken the philosophy of near real-time data beyond hospital acquired conditions; we have employed this strategically with infection control and infection prevention. Early and immediate identification and escalation of infection control requires real-time data and response. A new tactic that we have embarked upon is diagnostic stewardship. It is based on the premise that to improve our hospital acquired conditions related to infection control, we have to be immediate and agile in our responses. When our infection control practitioners see a possible infection related hospital acquired condition (such as a central-line associated bloodstream infection, catheter associated urinary tract infection, surgical site infection, etc.), they immediately bring the respective nursing and physician teams to work through the diagnosis. With data on infections, we have realized that if we wait a few weeks for perfectly clean attribution, then we lose the opportunity to see trends and prevent further potential contamination. This process of diagnostic stewardship is quite complex and beyond the scope of this re vi ew arti cle but it involves several micro-units partnering together to ensure the proper tests are ordered on patients in a timely fashion; this cannot be achieved with lagging data as the window of opportunity for these tests is lost. For example, if a patient has a suspected infection, prior to starting presumptive antibiotic therapy, the patient needs to have the proper panel of cultures ordered, obtained, and sent. This requires coordination amongst the nursing, clinical, infection control, quality, microbiology, and chief medical officer's teams. If this is not done in real-time with quasi real-time data then the diagnostic stewardship opportunity is lost. Inherent in this approach is a tacit understanding that the data will be messy (i.e. not perfect); this was noted above in the section on hospital acquired conditions as well.1 At Children's National we have become comfortable with not perfect data; indeed, this is a tenet of big data–that the data maybe messy.1 How we tease out the signal from the noise in the messy data is the concept of diagnostic stewardship.
Accreditation
The public across the world expects and demands that hospitals serve patients with the highest level of rigor. Accreditation and regulatory agencies, such as departments of health, governmental agencies, payers, etc., serve an indispensable role in this function. Accreditation and regulatory surveys occur on a periodic, however often unscheduled, pattern. Many organizations are not fully prepared for these visits and are reactive. At Children's National, we are proactive and real-time in our preparation and response to accreditation and regulatory issues. A brief example is that we embed a tracer methodology13 in our work so that we have our regulatory and accreditation teams round in all areas and then report this back real-time using the tools of the regulatory agencies back to the clinical teams. This real-time data allows us to impact and affect change that ultimately drives patient outcomes and reduces harm.
It is the holy grail of quality improvement in healthcare to drive towards high reliability.12 They exist five tenets of high reliability as outlined by Weick and Sutcliffe12; incorporation of tactics to move towards real-time data will broadly improve our efforts to move towards a healthcare system that can anticipate issues and quickly contain them as they occur.12 As with all quality improvement, this is a journey and Children's National continues on the path towards understanding the implications of real-time data and how to best leverage such data to drive safety and quality improvements.
CONFLICT OF INTEREST
The authors have no conflict of interests relevant to this article.