Natural course of low risk neuroblastoma†
Conflict of interest: Nothing to declare.
Abstract
Background
Neuroblastoma is characterized by heterogeneity of histology, biology, and clinical behavior. Most epidemiology studies are based on Western and Japanese populations; there are very few studies on neuroblastoma from Southeast Asia.
Procedure
Cases of Thai children with neuroblastoma were retrospectively reviewed to determine if the epidemiology of the disease differs from Western populations. Sixty-two cases were assembled from two pathology centers in Bangkok. Histologic prognostic category and MYCN copy number were determined.
Results
The median age at diagnosis was 2.9 years. Only 11% of cases presented at less than 1 year of age and 12% cases had low stage disease (1, 2, and 4S). The majority of tumors had unfavorable histology (48/62); this was at least partly due to the higher age at diagnosis for most patients. MYCN amplification was detected in 18/52 (35%) tumors, all in stage 3 or 4 tumors. We assigned patients to high, intermediate and low risk categories using the Children's Oncology Group risk stratification criteria. In contrast to Western studies, the majority of cases (50/59 or 85%) in our series had high risk disease.
Conclusions
Since there is no evidence to date that the biology of neuroblastoma varies by geographic region, the paucity of low risk cases in our study may reflect spontaneous resolution/differentiation of tumors that are not clinically detected. Moreover, a delay in diagnosis of intermediate risk cases could result in higher tumor burden at the time of diagnosis, increasing the proportion of high risk cases observed. Pediatr Blood Cancer 2012; 58: 690–694. © 2011 Wiley Periodicals, Inc.
INTRODUCTION
Neuroblastoma, the most common extracranial solid tumor of childhood 1, 2, is a malignancy of neural crest cells of the autonomic nervous system that most commonly is located in the adrenal medulla or along the sympathetic ganglion chain. This tumor occurs most frequently in children less than 5 years of age, with a median age at presentation of 17 months 3, affects approximately 1 in 7,000 children 4 and accounts for 15% of cancer-related deaths in childhood 2, 5.
Neuroblastoma is characterized by heterogeneity of histology and biology that is reflected in its variable clinical behavior 2, 6. Most epidemiology reports for neuroblastoma have been based on Western and Japanese populations, and these studies report a 25% incidence of low stage disease (stages 1 and 2) with a more favorable outcome, while the other 75% have high stage disease (stages 3 and 4) 1, 4 with a poor overall survival (OS) despite intensive therapy. Features associated with a poor outcome include: age greater than 18 months 3, skeletal metastasis and bone marrow involvement 4, unfavorable histopathology 7, amplification of the MYCN oncogene 8-10, diploid DNA content and specific segmental chromosomal aberrations such as 1p and 11q loss of heterozygosity 2, 11. Greater than 10 copies of the MYCN gene is an independent poor prognostic indicator, and is associated with advanced tumor stage, rapid tumor progression, and poor outcome. Approximately 20% of neuroblastoma tumors have amplification of the MYCN gene but this is more common (approximately 40%) in high stage tumors (stage 3 and 4) and uncommon (5–10%) in low stage tumors (stage 1, 2, or 4S) 2, 8, 10, 12, 13.
There are very few studies on neuroblastoma from Southeast Asia and almost no published biology data on these patients. The largest series from Malaysia included 78 patients ranging from 0.1 to 11 years old (median 3 years old) with a 2-year disease-free survival of 39%, and spanned 15 years 14. The majority of cases had stage 3 (22%) and stage 4 (66%) disease. In Thailand, a retrospective registry-based study reported 36 cases over a 3-year period (1995–1997), with most cases occurring between 1 and 4 years of age, with 3 cases greater than 5 years of age but only 2/36 cases in children less than 1 year 15. While the authors suggested that underreporting of cases may be a problem, neuroblastoma was still the fourth most common malignancy in Thai children. Details of staging and outcome were not included. A series of 18 cases from Singapore reported that half the patients were under 2 years of age 16. All patients were treated with radical surgery and some with adjunctive chemotherapy. With 4 years of follow-up provided, the authors reported a 50% survival and commented that these tended to be the cases with lower stage disease. No information on tumor histology or biology was provided in any of these series. The only report from Southeast Asia in which biological data were available was a series from Singapore that included 14 cases over a 5-year period 17. Five (36%) had favorable histology with normal MYCN copy number and all were alive except for one death from chemotherapy. The other nine (64%) had unfavorable histology, five of which were MYCN-amplified and the majority had a poor outcome.
The goal of our study was to describe the pattern of clinical and biological risk factors in a retrospective series of neuroblastoma cases in Thai children. In order to compare to other international studies, we categorized patients according to the COG risk stratification criteria. We identified very few cases with low risk tumors suggesting the biology, patterns of disease and/or clinical assessment of neuroblastoma might differ in this region of the world, compared to Western series.
MATERIALS AND METHODS
Cases diagnosed as neuroblastoma between 2000 and 2007 were retrieved from the pathology databases at The Institute of Pathology at Rajavithi Compound and King Chulalongkorn Memorial Hospital, Bangkok, Thailand. Studies were carried out with the ethical approval of both institutional review boards. A total of 67 patients were identified, all with histologic confirmation of their tumor. Formalin-fixed paraffin-embedded material was available on the tumors from 62 patients. For 2 of these 62 cases, the only biopsy performed was a bone marrow biopsy. Charts were reviewed to determine age at presentation, sex, and stage and, when available, outcome. Routine investigations for staging included: CT/MRI of primary tumor, serum levels of neuron-specific enolase, 24-hour urine for VMA, bone marrow aspirate (without or without a biopsy) and a bone scan except for patients with biopsy-proven metastatic disease in the bone marrow, liver, or skin. MIBG scan was not generally available. Staging was assessed according to the International Neuroblastoma Staging System 18. Histology on all tumors was classified according to the International Neuroblastoma Pathology Committee system 7, 19) by the institutional pathologists (SS and SS) and independently by a pediatric pathologist (PT). MYCN status was determined using chromogenic in situ hybridization (CISH) on paraffin embedded samples as described previously 20. CISH has been shown to be as reliable as fluorescent in situ hybridization detection of MYCN amplification and more accurate than Southern blotting or polymerase chain reaction 20-23. CISH has the advantage that sections from archival material can be evaluated by routine light microscopy, facilitating distinction between tumor and normal cells. Two hundred non-overlapping tumor nuclei were evaluated in each tumor specimen. Tumors were then classified as non-amplified or amplified (>10 copies) according to current standard guidelines 8-10. Risk group assignment was determined according to the system used by the Children's Oncology Group 2 which assigns patients as low, intermediate, or high risk based on combinations of stage, age, MYCN copy status, histology, and DNA ploidy at time of diagnosis. Since stage is only one parameter used in this system, high stage is not always equivalent to high risk. We were unable to assess ploidy retrospectively, and ploidy was only required to distinguish between low and intermediate risk in stage 4S patients with non-amplified favorable histology tumors. Therefore, we combined these two categories into one designated as “low/intermediate” risk for this rare subgroup that involved four patients (Table I). For the majority of patients (55) in the study, the lack of ploidy data did not affect our ability to assign patients to high, intermediate or low risk categories. The OS was analyzed by Kaplan–Meier plot using SPSS program version 17.0.
| INSS stage | Age | MYCN status | Shimada histology | Risk group | # of cases |
|---|---|---|---|---|---|
| 1 | 0–21y | Any | Any | Low | 0 |
| 2A/2B | <1.5y | Any | Any | Low | 2 |
| 1.5–21y | Nonamplified | Any | Low | 0 | |
| 1.5–21y | Amplified | Favorable | Low | 0 | |
| 1.5–21y | Amplified | Unfavorable | High | 0 | |
| 3 | <1.5y | Nonamplified | Any | Intermediate | 0 |
| <1.5y | Amplified | Any | High | 1 | |
| 1.5–21y | Nonamplified | Favorable | Intermediate | 0 | |
| 1.5–21y | Nonamplified | Unfavorable | High | 9 | |
| 1.5–21y | Amplified | Any | High | 4 | |
| 4 | <1.5y | Nonamplified | Any | Intermediate | 3 |
| <1.5y | Amplified | Any | High | 5 | |
| 1.5–21y | Any | Any | High | 31 | |
| 4S | <365d | Nonamplified | Favorable | Low/intermediatea | 4 |
| <365d | Nonamplified | Unfavorable | Intermediate | 0 | |
| <365d | Amplified | Any | High | 0 |
- a DNA ploidy is required to distinguish “low” and “intermediate” risk in this subgroup. Since ploidy was not available, the risk was designated as “low/intermediate.”
RESULTS
The cohort consisted of 23 female and 39 male patients with neuroblastoma. The ages of diagnosis ranged from 6 months to 11 years, with a mean of 3.4 years and median of 2.9 years. Interestingly, only 7/62 (11%) cases presented at under 1 year of age. Sites of the biopsy specimen at diagnosis included the adrenal gland (n = 22), retroperitoneum (n = 15), lymph node (n = 11), bone marrow (n = 4), liver (n = 3), other (mediastinum, thoracic extradural space paraspinal, abdomen, submandibular and soft tissue not otherwise specified (n = 7). We had adequate information to assess INSS stage on 60/62 patients. There were 2 patients with stage 2 disease, 14 patients with stage 3 disease, 39 with stage 4 disease, and 5 patients with stage 4S disease. Thus, 12% (7/60) of cases had low stage neuroblastoma (1, 2, and 4S). In contrast, in Western populations stages 1, 2, and 4S together comprise 25% of all cases 1, 4. Three patients were diagnosed by bone marrow aspirate only and included one with stage 4S and two with stage 4 disease. Two patients, also with stage 4 disease, had tissue biopsy confirmation but no paraffin blocks available. These five patients were not included in the study due to inadequate tissue. The majority (48/62) had unfavorable histology, at least in part due to the higher age at diagnosis for most patients, since age is one of the key determinants of histology prognosis in the International Neuroblastoma Pathology Committee system 7, 19. MYCN amplification was detected by CISH in 18/52 (35%) tumors for which hybridization was successful. All MYCN-amplified tumors were in patients with high-stage disease (5 stage 3 and 13 stage 4).
We were able to retrospectively determine the COG risk category in 55 cases. For the five stage 4S patients, four were assigned to low/intermediate because DNA ploidy was not available to distinguish low from intermediate risk categories. The fifth case lacked both information on ploidy and MYCN status and risk category could therefore not be assigned. An additional two cases could not be assigned due to lack of clinical staging information. Overall, based on COG risk groups 50/59 cases (85%) were determined to meet high risk criteria. The expected value for high risk based on Western populations is 50% 2.
Over 50% (33/62) of patients were lost to follow up and thus long term survival data are incomplete. Of the nine cases in the low and intermediate risk categories (including the 4S cases), six were alive with follow-up periods ranging from 8 to 106 months. Two cases, both stage 4 intermediate risk, had died at 5 and 13 months, respectively, and one case had no follow-up data. The one case of stage 4S that could not be assigned a risk group was alive at 64 months. Of the 50 patients with high risk tumors, 26 were alive with follow-up periods of 3–86 months (median 23 months), 16 had died of their disease and 8 had no follow-up data. Overall survival as related to stage, histology, and MYCN status is shown in Figure 1. Children with stage 3 neuroblastoma had an OS of 66 ± 16% while children with stage 4 disease had an OS of 31 ± 12%. The differences in OS by stage did not reach statistical significance (P = 0.27 by log rank test). Children with favorable histology had significantly better OS (77 ± 15%) compared with those with unfavorable histology (43 ± 11%) (P = 0.035 by log rank test). Most children with MYCN-amplified tumor died within 4 years of diagnosis, with only 1/18 surviving (OS of 16 ± 14%). In contrast, children whose tumors were not MYCN-amplified had significantly better OS (65 ± 12%) (P = 0.025 by log rank test).
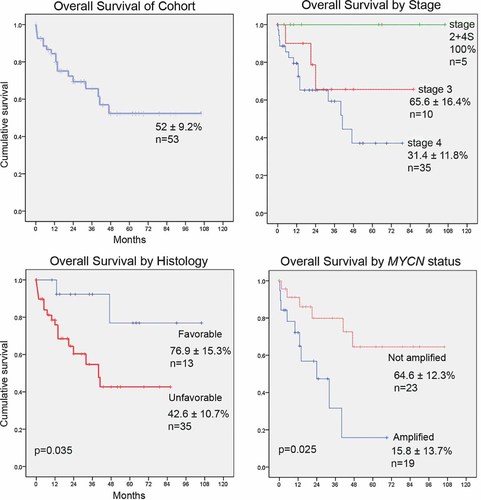
Kaplan–Meier survival plots according to stage, histology and MYCN status. Below each curve are estimate ± standard error of the mean; n = number of analyzable patients in each group; P-value indicates comparison between the two groups by log-rank test. When comparing histology, children with favorable histology NB had significantly better overall survival compared with those with unfavorable histology NB (P = 0.035 by log rank test). When comparing MYCN status, children whose tumors were not MYCN-amplified had a significantly better OS compared to those with MYCN-amplified tumors (P = 0.025 by log rank test). The differences in OS by stage did not reach statistical significance (P = 0.27 by log rank test).
There were also four cases with ganglioneuroma identified during the same study period. These included three females and one male and the ages ranged from 6 to 12 years with an average of 8.8 years. All were alive at least 12 months after diagnosis. None of the four tumors was MYCN-amplified.
DISCUSSION
Neuroblastoma is a clinically and biologically heterogeneous tumor with distinct subtypes. Risk stratification schemes based on clinical and biological risk factors have been devised to identify groups of patients with markedly different outcomes, allowing treatment intensity to be adjusted accordingly 2. Although progression from low risk to high risk disease occurs in some cases, in the majority, it is likely that high risk and low risk disease are inherently different 4. The present risk stratification system has been based on several decades of experience in patients with neuroblastoma in Western countries, with input from Japanese population studies. Few studies 14-17 have examined the incidence of neuroblastoma outside of North America, Europe, Japan, and Australia and thus, it is currently unclear whether clinical and biological factors used in neuroblastoma risk stratification are applicable to all countries. In applying the COG risk stratification system to a retrospective study of neuroblastoma at two oncology centers in Thailand, we found that the proportion of high risk cases (85%) was higher than the 50% value reported in Western studies 2. Similarly, a small study from Malaysia found 88% of cases had stage 3 or 4 disease, and it is likely that the majority of these patients would meet COG high risk criteria 14. In contrast, epidemiology studies from Japan report a proportion of high stage disease that is similar to those in North American and European studies 24, 25. Moreover, a recent COG study separating neuroblastoma patients in North America by race showed no significant differences in survival or the incidence of high risk disease between Asian and Caucasian patients; however, the number of Asian patients in the study was small 26.
Our study was conducted in 2 of the 25 tertiary care referral centers in Bangkok, Thailand. Since all centers in Thailand use the same protocols and patients referrals are based on proximity to the treating center, it is unlikely that there was bias towards referral of high risk cases to our two centers. One possibility as to why we identified so few patients with low risk disease may be due to delay in diagnosis. However, since the biology of low risk and high risk tumors is likely different from inception 27, low risk tumors transforming over time into high risk cases is unlikely. Patients with intermediate risk tumors might be expected to progress without treatment and, if diagnosis were delayed, they might present at a more advanced stage. Since the designation of risk category is age-dependent, older age at presentation might result in a tumor being reclassified from intermediate to high risk. Patient with high risk disease constituted the majority of our series; and the average age in our study was generally higher than that seen in Western healthcare institutions, with almost no patients under 1 year of age.
We speculate that the decreased percentage of low risk cases observed in our cohort is due to spontaneous differentiation or regression of tumors that that did not come to medical attention. Pre-natal ultrasound use is limited to academic hospitals in Thailand and, at most, is performed once between gestational ages of 18 and 22 weeks. Therefore, low risk tumors identified from prenatal ultrasound examination and other screening procedures in Western and Japanese studies 2, 4, 24 would not be detected in patients in our cohort. Patients with localized disease (stages 1 and 2) have excellent survival rates and require less treatment than those with advanced stage disease 1, 4, 28. These tumors tend to have favorable biological features 2 and have been managed by surgery alone 1, 28, 29 or observation 30-34. These studies showed that 60% of such tumors eventually regressed, and the remainder had differentiated by 18 months 30, 35, an age younger than the majority of the patients in our study.
Our study does not rule out the possibility of biologic differences between neuroblastoma in Thailand and Western countries. Recently single nucleotide polymorphisms have been identified that are associated with high-risk disease in Western populations 27, 36. Further studies may determine whether the incidence of these polymorphisms or other biologic features vary among patients of different racial or ethnic backgrounds.
Acknowledgements
This work was funded by the James Birrell Neuroblastoma Research Fund, Hospital for Sick Children (to Dr. Thorner and Dr. Irwin) and by the Ratchadapisek Somphot Endowment Fund, Chulalongkorn University (to Dr. Shanop Shuangshoti).