Longitudinal associations between child discipline methods and physical growth patterns across preschool years
Abstract
Objective
Research has documented the associations of child maltreatment with a range of physical health problems, but little is known about the physical growth patterns of children who experience maltreatment in early childhood. This study aimed to examine the association between various discipline approaches and physical growth in preschool-aged children.
Methods
In the first year of preschool, parents of 661 Chinese preschool-aged children completed a questionnaire with items pertaining to the frequency of using physical maltreatment, psychological aggression, neglect, and nonviolent discipline toward the child. Children's weight and height were assessed annually using direct assessment in the first and two subsequent years. Longitudinal analyses were performed using multiple regression models.
Results
More frequent neglect and psychological aggression during the first year of preschool were associated with a higher likelihood of a decreased BMI z score in subsequent years. Conversely, increased experience of physical maltreatment in the first year was associated with an increased likelihood of having overweight or obesity in the third year.
Conclusions
Results indicate that early maltreatment experience can impact physical growth. This highlights the importance of preventing abusive parenting and encouraging healthy habits in young children who have experienced maltreatment to decrease their future risk for weight problems.
Study Importance Questions
What is already known?
- Childhood abuse experience is associated with adulthood obesity.
What does this study add?
- Unusual physical growth patterns during early childhood may partially stem from maltreatment and result in weight problems at older ages.
How might these results change the direction of research or the focus of clinical practice?
- Implementing policies that address childcare burden and promote stress management skills in both parents and children can be effective in reducing the factors that contribute to child maltreatment.
INTRODUCTION
Much research has demonstrated the effect of child maltreatment on weight and weight-related outcomes in adulthood, but little work has been done to investigate its relationship with physical growth patterns during childhood. The first meta-analysis of studies on the association between childhood maltreatment and obesity was published in 2014. After pooling results of 33 studies on adults and 9 studies on children/adolescents, significant associations were observed only in adults [(1)]. There is also evidence indicating that the earliest age at which this association can be observed in both genders is 18 years old [(2)]. Although considerable attention has focused on the adult physical health outcomes related to child maltreatment, the absence of a correlation during childhood could be due to the lack of robust research with adequate time intervals between the maltreatment exposure and the assessment of the consequences. In 2017, a different meta-analysis was conducted, which centered on research examining differences in the risk of overweight among children and adolescents who had experienced two or more adverse events during childhood. However, only two studies included in the meta-analysis were performed in early childhood (i.e., ≤ 5 years), and the pooled results were significant primarily in studies with follow-up periods of ≥ 2 years [(3)]. A more recent review, published in 2021, also indicates that it could take anywhere from 2 to 5 years for adverse childhood experiences to have an impact on the development of childhood obesity [(4)]. A better understanding of the link between early life adversity and suboptimal growth would be useful for advancing the intervention and prevention efforts that have traditionally targeted inactivity and malnutrition as the main culprits of growth issues.
Child maltreatment is common and affect many individuals across the globe. Studies analyzing multiple sources of data indicate that over 1 billion children between the ages of 2 and 17 experienced violence in the preceding year, which accounts for more than half of all children worldwide [(5)]. Child maltreatment refers to any actions or inactions by a caregiver that causes harm or has the potential to cause harm to a child [(6)]. The four primary categories of child maltreatment are (a) physical abuse, where a child is intentionally harmed physically; (b) neglect, which includes both not providing basic care and not supervising a child adequately; (c) emotional abuse/psychological aggression, which involves consistently denying a child's fundamental emotional requirements in a severe and persistent manner; and (d) sexual abuse, where a child is subjected to sexual activity. Past studies have highlighted the importance of exploring maltreatment events that occur during early childhood (ages 3–6 years) [(7-9)], which is a critical stage in a child's development. During this period, children undergo primary developmental processes that lay the foundation for their abilities and skills. Maltreatment during this time can have significant impacts on a child's emotional, social, cognitive, and behavioral functioning and has been linked to altered brain development and increased illness severity [(10, 11)]. Despite the importance of this topic, our understanding of the physical growth of maltreated children during early childhood remains limited, with most research focusing on physical outcomes in adulthood [(1, 12)]. Only a few studies have examined the physical health consequences of maltreatment in early childhood [(7, 8, 13)].
Suboptimal growth refers to abnormal growth conditions that deviate from the median, either above or below it. A basic evaluation to assess the growth of children aged 1 month–18 years involves taking measurements of their weight and length or height and comparing them with growth standards [(14)]. Suboptimal growth can manifest as weight problems such as underweight, overweight, or obesity, as well as height issues such as stunting. If left unaddressed, these problems may persist into adulthood and increase the risk of age-related illnesses, such as accelerated cognitive decline and cardiovascular diseases [(15)]. In addition to genetic influences, environmental factors are also known to play a role in the variations of weight and height [(16)]. For instance, the context and characteristics of the trauma, such as their severity and type, may contribute to the differences observed in physical growth patterns following childhood maltreatment. Although researchers have pointed out that an acute or temporary growth failure following childhood maltreatment may not persist into adulthood [(17)], a deficit observed in a short follow-up period, particularly in early childhood, should not be neglected, as it reveals the importance and optimal timing of early intervention to promote catch-up growth. In studies examining the association between maltreatment and weight in young children [(13, 18)], mixed findings indicating risk for both weight extremes have been reported, but these studies have typically focused on one form of maltreatment. When considering multiple forms of maltreatment, researchers found no association between the number of adverse childhood experiences and weight status in children [(19)]. Hence, there are still significant gaps in our understanding of how various types of violent and nonviolent discipline methods interact to influence children's long-term growth and weight outcomes.
The present study aimed to determine whether the frequency of theoretically distinct types of maltreatment (i.e., physical maltreatment, psychological aggression, and neglect) and nonviolent disciplines experienced in the first year of preschool was directly proportional to weight and height changes in subsequent years. Our second goal was to test whether these child discipline methods predicted weight categories in subsequent years. The final goal was to determine whether specific forms of maltreatment interacted with each other to predict weight changes in the third year of preschool. We expected that a higher frequency of maltreatment during the first year of preschool would be associated with greater variations in physical growth patterns by the third year of preschool. We additionally predicted that this association would differ based on the type of maltreatment, whether it occurred alone or in conjunction with other forms of maltreatment.
METHODS
Participants and procedures
This study, consisting of 661 Chinese preschool-aged children and their parents, obtained ethics approval from the Institutional Review Board of The University of Hong Kong and Hospital Authority Hong Kong West Cluster. A three-wave longitudinal design was employed. The study took place in 2018 (the first year of preschool, T1), and we conducted two additional follow-up assessments in 2019 (the second year, T2) and 2020 (the third year, T3). Upon obtaining informed consent at the school level, invitation letters were sent to all families in the first-year classes of the selected kindergartens in Hong Kong and 661 families provided consent to participate in this study. Throughout the study period, participants had the option to withdraw from any of the follow-up assessments if they chose to do so. The children's height and weight were assessed by research assistants at the kindergartens during each assessment time point. In addition, the parents completed a questionnaire on demographic factors and another questionnaire on child maltreatment at T1.
Measures
Anthropometric assessments
At each time point, children's body weight and standing height were measured by a trained research assistant according to the standard methods. Children's weight was measured using a digital scale (Model BF-522; Tanita Corporation of America, Inc.) while they were dressed in lightweight clothing and not wearing any shoes. The measurements were recorded to the nearest 0.1 kg. To measure the standing height of the children, a portable stadiometer (Model no. 213; SECA Gmbh & Co. KG) was used, and the readings were recorded to the nearest 0.1 cm. A z score method based on the standard reference was used to calculate the standard deviation score of mean height and body mass index (BMI) of the children in this study [(20, 21)].
Questionnaires
Child maltreatment
At T1, the children's experiences of maltreatment in the preceding year were assessed by asking their parents to complete the Chinese version of the 27-item Parent-Child Conflict Tactics Scale (CTSPC) [(22)]. The CTSPC consists of six subscales, which include nonviolent discipline (four items, e.g., took away privileges or grounded him/her), psychological aggression (five items, e.g., swore or cursed at him/her), physical maltreatment (six items, e.g., slapped him/her on the hand, arm, or leg), severe physical maltreatment (three items, e.g., threw or knocked him/her down), very severe physical maltreatment (four items, e.g., burned or scalded him/her on purpose), and neglect (five items, e.g., were not able to make sure your child got the food he/she needed). This study examined all the subscales, except for the severe and very severe physical maltreatment subscales. These subscales were excluded because they were rare among the children in this study. Furthermore, their inclusion may lead to biased results because severe abuse may result in injuries that can have an impact on the child's ability to eat. On a scale of 0 to 6, the CTSPC questions were ranked with 0, meaning it did not happen, and 6, meaning it happened over 20 times. The subscale total score was determined by adding the frequency scores of the subscale items together. A higher score indicated that the parents used the discipline more frequently. The Chinese version of the CTSPC has satisfactory levels of internal consistency and validity [(23, 24)]. The subscales included in the present study had Cronbach α of 0.68 (physical maltreatment), 0.75 (psychological aggression), 0.37 (neglect), and 0.75 (nonviolent discipline).
Demographic information
At T1, parents disclosed their family's income and provided details on their own and their spouse's education level and employment status. They also reported whether their children received additional learning and developmental support services. Their children's age, gender, and residential area were obtained from school records.
Data analysis
Descriptive statistics were computed to summarize the children's demographics, maltreatment experiences, and anthropometric measurements at each time point. All children underwent the three anthropometric assessments, but the percentage of missing values for child maltreatment parameters ranged from 6.4% to 9.2%. Given the limited amount of missing data, multivariate imputation by chained equation was used to impute the missing data [(25)]. We conducted a repeated-measures ANOVA to investigate the impact of child maltreatment status at T1 on BMI z score trends across the three time points, examining both the between-subject and within-subject effects. Three linear regressions models were constructed for the associations between child maltreatment experiences and anthropometric measurements. Model 1 examined the cross-sectional relationships at T1, whereas Model 2 and Model 3 were built to test the prospective relationship of child maltreatment experiences at T1 (measured as frequency on a continuous scale) with weight and height changes at T2 and T3, respectively. In addition, the children's BMI was segregated into “underweight,” “healthy weight,” and “overweight/obesity” categories based on the International Obesity Task Force (IOTF) criteria [(26)]. Logistic regression models were used to examine the associations between weight categories and child maltreatment experiences. Because the number of underweight children was low in stratified analyses, further logistic regression analyses with the underweight group were not conducted. To examine the concurrent and predictive associations, child maltreatment experiences at T1 (measured as frequency on a continuous scale) were regressed on the overweight/obesity category at T1 in the concurrent model (Model 1). For the predictive models, the overweight/obesity categories at T2 and T3 were analyzed in Model 2 and Model 3, respectively. Covariates included in Model 1 were child age, gender, residential area, history of receiving additional early intervention services, family socioeconomic status (SES), and other types of child maltreatment exposure. Family SES was assessed by a composite index of maternal and paternal education, maternal and paternal occupation, and adjusted monthly household income using principal component analysis with varimax rotation [(27)]. Model 2 and Model 3 were further adjusted for the T1 height or BMI z score depending on the outcome of interest. One-way ANOVA with Bonferroni post hoc test was performed to determine whether the experience of multiple maltreatment types at T1 influenced the subsequent changes in BMI z scores at T3. The potential confounders were determined based on previous literature on obesity and child maltreatment, taking into account the available parameters in this study. All linear regression coefficients were standardized, and the p value < 0.05 was considered statistically significant.
RESULTS
Participants' sociodemographics
Table 1 shows the main characteristics of the participating children. The average age of the children at T1 was 3.78 years. Forty-five percent were boys. In addition, 45% had received additional early intervention services. Half of the mothers were full-time housewives, and 31.2% had completed postsecondary education. For the fathers, most of them (84.9%) were employed full-time, and 26.4% had completed postsecondary education. Regarding child maltreatment experiences, most of the children had experienced at least one episode of physical maltreatment (83.0%), psychological aggression (82.2%), or nonviolent discipline (90.5%). Among the children who had encountered physical maltreatment, 11% experienced a severe level of maltreatment, whereas 2% endured a very severe level. Neglect experiences were found in 140 (22.8%) children. The prevalence of underweight among the children remained low and stable, whereas the prevalence of overweight and obesity ranged from 13.9% to 20.0% across the 3 time points.
| Characteristics | K1 (Time 1, T1) | K2 (Time 2, T2) | K3 (Time 3, T3) |
|---|---|---|---|
| Mother | |||
| Education, n (%) | |||
| Lower secondary | 198 (30.0) | - | - |
| Upper secondary | 250 (37.8) | - | - |
| Postsecondary | 111 (16.8) | - | - |
| Undergraduate | 95 (14.4) | - | - |
| Missing | 7 (1.1) | - | - |
| Job, n (%) | |||
| Full-time | 214 (32.4) | - | - |
| Part-time | 74 (11.2) | - | - |
| Job seeking | 20 (3.0) | - | - |
| Housewife | 346 (52.3) | - | - |
| Missing | 7 (1.1) | - | - |
| Father | |||
| Education, n (%) | |||
| Lower secondary | 181 (27.4) | - | - |
| Upper secondary | 287 (43.4) | - | - |
| Postsecondary | 91 (13.8) | - | - |
| Undergraduate | 83 (12.6) | - | - |
| Missing | 19 (2.9) | - | - |
| Job, n (%) | |||
| Full-time | 561 (84.9) | - | - |
| Part-time | 25 (3.8) | - | - |
| Job seeking | 35 (5.3) | - | - |
| Househusband | 17 (2.6) | - | - |
| Missing | 23 (3.5) | - | - |
| Monthly household income (HKD '000), mean (SD) | 26.8 (18.3) | - | - |
| Family SES, mean (SD) | −0.03 (1.32) | - | - |
| Child | |||
| Age, mean (SD) | 3.78 (0.44) | - | - |
| Gender, n (%) | |||
| Boys | 297 (44.9) | - | - |
| Girls | 364 (55.1) | - | - |
| Receiving additional early intervention services, n (%) | |||
| Yes | 296 (44.8) | - | - |
| No | 365 (55.2) | - | - |
| Child maltreatment prevalencea, n (%) | |||
| Physical maltreatment | 498 (83.0) | - | - |
| Psychological aggression | 499 (82.2) | - | - |
| Neglect | 140 (22.8) | - | - |
| Nonviolent discipline | 545 (90.5) | - | - |
| Height (cm), mean (SD) | 100.0 (4.6) | 104.1 (4.8) | 114.1 (5.5) |
| Weight (kg), mean (SD) | 15.5 (2.1) | 16.7 (2.5) | 20.2 (4.1) |
| z score, mean (SD) | |||
| Height | 0.12 (1.01) | 0.17 (1.02) | 0.25 (1.03) |
| BMI | 0.07 (0.94) | 0.004 (1.01) | 0.12 (1.10) |
| BMI category, n (%) | |||
| Underweight | 10 (1.5) | 14 (2.1) | 14 (2.1) |
| Healthy weight | 551 (83.4) | 555 (84.0) | 515 (77.9) |
| Overweight | 83 (12.6) | 71 (10.7) | 94 (14.2) |
| Obesity | 17 (2.6) | 21 (3.2) | 38 (5.7) |
| Overweight or obesity | 100 (15.1) | 92 (13.9) | 132 (20.0) |
- Abbreviations: HKD, Hong Kong dollar; SES, socioconomic status.
- a Missing data not shown.
Changes in anthropometric measurements at 1 and 2 years after maltreatment exposure
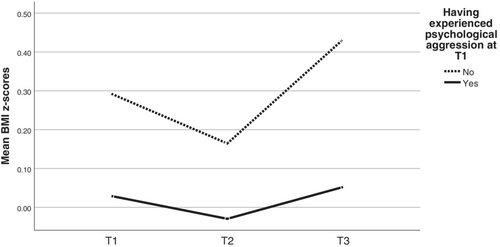
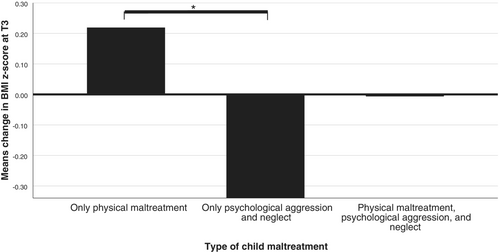
For the linear regression analysis (Table 2), despite no association with concurrent maltreatment events, neglect event frequency at T1 significantly predicted a decrease in BMI z score (β = −0.09, p = 0.032) and height z score (β = −0.12, p = 0.002) at T2 after adjusting for confounding variables. At T3, after adjusting for confounding variables, the effect of T1 neglect frequency on changes in BMI z score remained statistically significant (β = −0.11, p = 0.005). In addition, psychological aggression frequency independently predicted a decrease in BMI z score (β = −0.11, p = 0.038), whereas physical maltreatment frequency predicted an increase (β = 0.13, p = 0.007). The repeated-measures ANOVA showed that mean BMI z scores differed significantly within and between groups stratified by the respective status of physical maltreatment (F[1, 652] = 9.470, p = 0.002; Figure 1) and psychological aggression (F[1, 652] = 6.735, p = 0.010; Figure 2) across the three time points. Further analysis using one-way ANOVA with adjustment for covariates showed an association between the type of maltreatment experienced and BMI z score changes at T3 (F = 3.91, p = 0.021), with significant differences observed between children exposed to physical maltreatment only and those exposed to psychological aggression and neglect only (Figure 3). By contrast, owing to the opposing actions of physical maltreatment and psychological aggression and neglect, almost zero change in BMI z score at T3 compared to T1 was observed in the group exposed to all these three maltreatment types (mean change = −0.008), which was similar to the condition observed in the nonmaltreated group (mean change value = 0.021). For the logistic regression analysis (Table 3), after adjusting for covariates, the associations between maltreatment exposure at T1 and overweight/obesity status at T1 and T2 were not significant. However, the odds of having overweight/obesity at T3 increased with the frequency of exposure to physical maltreatment at T1 (adjusted odds ratio [aOR] = 1.06, 95% confidence interval [CI] = 1.02–1.11).
| Child discipline methods | Model 1 (T1 value) | Model 2 (T2−T1 change) | Model 3 (T3−T1 change) | |||
|---|---|---|---|---|---|---|
| Concurrent βa | p value | Predictive βb | p value | Predictive βb | p value | |
| BMI z score | ||||||
| Physical maltreatment | 0.05 | 0.297 | 0.05 | 0.334 | 0.13 | 0.007 |
| Psychological aggression | −0.02 | 0.737 | −0.01 | 0.865 | −0.11 | 0.038 |
| Neglect | −0.01 | 0.799 | −0.09 | 0.032 | −0.11 | 0.005 |
| Nonviolent discipline | 0.03 | 0.443 | 0.04 | 0.330 | −0.02 | 0.724 |
| Height z score | ||||||
| Physical maltreatment | 0.02 | 0.656 | 0.001 | 0.987 | −0.01 | 0.920 |
| Psychological aggression | 0.04 | 0.504 | 0.013 | 0.797 | 0.05 | 0.375 |
| Neglect | −0.02 | 0.616 | −0.12 | 0.002 | −0.07 | 0.093 |
| Nonviolent discipline | −0.05 | 0.286 | 0.01 | 0.836 | 0.05 | 0.285 |
- a The multivariable model simultaneously adjusted for child age, gender, residential area, history of receiving additional early intervention services, family socioeconomic status, and other types of child maltreatment exposure.
- b Model 1 additionally adjusted for the z score at T1.

| Child discipline methods | Model 1 (T1 category) | Model 2 (T2 category) | Model 3 (T3 category) | |||
|---|---|---|---|---|---|---|
| Concurrent OR (95% CI)a | p value | Predictive OR (95% CI)b | p value | Predictive OR (95% CI)b | p value | |
| Overweight or obesity (reference: healthy weight) | ||||||
| Physical maltreatment | 1.01 (0.99, 1.03) | 0.329 | 1.03 (0.995, 1.06) | 0.099 | 1.06 (1.02, 1.11) | 0.009 |
| Psychological aggression | 0.99 (0.98, 1.01) | 0.493 | 0.98 (0.95, 1.02) | 0.259 | 0.97 (0.93, 1.02) | 0.216 |
| Neglect | 0.98 (0.91, 1.06) | 0.684 | 0.96 (0.82, 1.14) | 0.652 | 0.84 (0.65, 1.09) | 0.197 |
| Nonviolent discipline | 1.00 (0.99, 1.01) | 0.892 | 1.00 (0.98, 1.02) | 0.781 | 1.01 (0.98, 1.03) | 0.615 |
- Abbreviation: OR, odds ratio.
- a The multivariable model simultaneously adjusted for child age, gender, residential area, history of receiving additional early intervention services, family socioeconomic status, and other types of child maltreatment exposure.
- b Model 1 additionally adjusted for the BMI z score at T1.
DISCUSSION
The findings of this study revealed that child maltreatment experiences during the first year of preschool can influence the trajectory of BMI z score changes in the following years. Specifically, it has two significant contributions to the field. The first contribution is the investigation of the physical health implications of child maltreatment during early childhood, which is a development stage that has received little attention. Promoting optimal physical growth during early childhood is important because it sets the foundation for future health and wellness, yet little is known about the effect of maltreatment on physical growth in this stage [(1, 3)]. The second contribution of this research is to disentangle the independent and interactive effects of different violent and nonviolent discipline methods on physical growth. The effects were examined in both categorical and continuous formats that go beyond the traditional cumulative risk approach and the emphasis on a particular weight category, as we explored differences in BMI as a marker of sensitivity to maltreatment effects.
Consistent with previous studies that explored the effect of follow-up interval on maltreatment outcomes, we noticed that the immediate impact of child maltreatment on physical growth was small. Specifically, we did not find any concurrent associations between maltreatment and physical growth patterns in the first-year assessment. However, we noticed that certain forms of maltreatment were linked to changes in anthropometric measures in subsequent years. It is worth mentioning that physical maltreatment predicted the status of having overweight or obesity only 2 years after the maltreatment incident. Focusing on events in early childhood reduces the likelihood of biases related to prior maltreatment exposure or other ecological factors that could have influenced the associations noted in previous studies involving older participants. Our findings can, therefore, reinforce prior research that indicate a minimum of 2 years for the effects of maltreatment on weight status to become apparent [(3, 4)]. Another noteworthy finding is the alarmingly high prevalence of child maltreatment reported in our study compared to a previous study conducted in Hong Kong using the same questionnaire measure, which reported rates of 69.5% for physical maltreatment, 86.3% for psychological aggression, and 21.0% for neglect among 6-year-olds [(28)]. These differences may arise from the fact that parents in our study typically completed the child maltreatment questionnaire when their children were 3 years old, as opposed to the 6-year-olds in the previous study. At the age of three, children have less developed emotional and behavioral self-regulation skills, which could result in more challenging parenting situations and potentially increase the likelihood of incidents of child maltreatment. Additionally, approximately half of the participants in our study came from disadvantaged backgrounds, which are recognized risk factors for child maltreatment [(29)].
When examining the impact of the three forms of maltreatment, physical maltreatment was most predictive of future increases in BMI and risk of having overweight/obesity, whereas psychological aggression predicted future decreases in BMI. Neglect, on the other hand, seemed to have an immediate impact on the child's weight and height during early childhood, which differed from the other two forms of maltreatment that required more time to produce noticeable effects. This finding is consistent with prior studies that found child neglect to be associated with unhealthy weight patterns in early childhood [(13, 18)]. Neglected children may experience poor growth due to either not getting enough food or consuming too many high-calorie junk foods [(30)]. The weight loss observed in the present study may be partly due to insufficient food intake, but the fact that neglect did not significantly affect height in the second year of follow-up may suggest that heredity also plays a role in height growth [(16)]. This possibility warrants further investigation in future studies.
Because the effect of psychological aggression and physical maltreatment on physical growth required 2 years to manifest, stress mechanisms were likely involved in explaining their effects. Earlier studies have highlighted the impact of stress levels on response differences [(31)]. The stress caused by psychological aggression in early childhood may cause a decrease in appetite, leading to weight loss. On the other hand, the experience of physical maltreatment during this period may cause intense stress that can alter a child's perceptual processes, making them more likely to perceive situations as threatening even if they are not. This can lead to prolonged activation of the hypothalamic-pituitary-adrenal (HPA) axis [(32)]. Although consuming hyperpalatable and comforting foods can help stop the activation of the HPA axis caused by stress, if stress persists for a long time, consuming such foods can increase the risk of obesity or even pathological eating patterns [(33)]. The experience of violence may also account for the impact of physical maltreatment on physical growth, given that nonviolent discipline methods were found to have no influence on physical growth. This finding is similar to previous research findings that reported the benefits of nonviolent discipline skills to de-escalating explosive or aggressive situations [(34)]. Collectively, these findings indicate that the experiences of discipline methods are important to elucidating variations in physical growth patterns among young children.
Finally, the frequency and interaction of different types of maltreatment were also predictive of physical growth patterns during early childhood. Specifically, the finding that a higher frequency of maltreatment in the first year of preschool predicted greater BMI changes and risk of unhealthy weight status in subsequent years is in line with prior research that reported a link between maltreatment chronicity and psychosocial outcomes [(35)]. Additionally, our results revealed that when multiple forms of maltreatment occurred simultaneously, their effects on anthropometric changes can negate each other, resulting in no discernible difference from the outcomes of nonmaltreated situations. As such, it could be difficult to notice their combined effects on physical growth in the early years. Further research is necessary to determine whether delayed growth would become more noticeable among children exposed to multiple forms of maltreatment as they age.
There are several limitations that need to be considered when interpreting the results of this study. First, in this study, approximately half of the families earned less than the average income for a 3-member household in Hong Kong. Families with higher financial resources may have additional means to counteract the negative effects of early maltreatment. These income disparities could potentially limit the generalizability of the findings to other populations with smaller income differences. Future work should examine the unique and shared influences of maltreatment exposure, protective resources, and family SES on children's physical growth. Second, this study solely focuses on the frequency of maltreatment and the duration it takes for a specific type of maltreatment to produce noticeable effects. Other dimensions of chronicity, such as the continuity of maltreatment, could also affect physical growth and should be explored in future research. Third, the use of single reporters for quantifying child maltreatment and discipline methods is susceptible to self-reporting biases. Obtaining data from third parties such as another parent or government agencies can increase the accuracy and validity of the maltreatment experiences. Finally, there were no measures of lifestyle behaviors such as exercise and eating habits, which are closely linked to physical growth and could have influenced our results.
The results of the current study have important implications for policies and services for at-risk families, especially the findings on the delayed effects of certain types of maltreatment and the role of BMI variations in response to different maltreatment types. For example, although immediate physical impairments may not be evident after maltreatment, it is important for teachers and other professionals to remain attentive to the emotional and physical needs of maltreated children, because the effects of maltreatment on physical growth may take time to become apparent. Policies aimed at improving the accessibility of stress management training programs for maltreated children are likely to be effective in reducing the adverse effects of stress caused by maltreatment. Additionally, support services should be provided to help parents effectively cope with childcare challenges and other sources of stress associated with child maltreatment.
On the other hand, because maltreatment is associated with BMI changes in early childhood, it may serve as a precursor to unhealthy weight conditions and other age-related diseases later in life. Adopting healthy lifestyle habits could be a direct and effective approach to prevent maltreated children from experiencing suboptimal growth and health. However, because most interventions for maltreated children focus on addressing mental health issues, it is imperative for policymakers and other professionals to implement more preventive efforts toward mitigating the physical health consequences. For example, lifestyle interventions that use behavioral therapy techniques to encourage healthy eating and regular exercise could be a promising way to reduce the risk of disease and confer a range of mental and physical health benefits.
CONCLUSION
Taken together, our findings contribute to the growing literature suggesting that unusual physical growth patterns during early childhood may partially stem from maltreatment and result in weight problems at older ages. Additionally, different types of maltreatment may have opposite effects due to distinct stress mechanisms. Longitudinal research that examines the co-emergence and interaction of maltreatment-induced deficits in physical and mental health since early childhood will foster a more comprehensive understanding of the developmental processes that contribute to future diseases.
AUTHOR CONTRIBUTIONS
Rosa S. Wong: Conceptualization, methodology, formal analysis, investigation, resources, writing-original draft, writing-review & editing. Keith T. S. Tung: Methodology, data curation, investigation, writing-review & editing. Frederick K. W. Ho: Methodology, investigation, writing-review & editing. Nirmala Rao: Methodology, investigation, writing-review & editing. Ko Ling Chan: Methodology, investigation, writing-review & editing. Patrick Ip: Conceptualization, methodology, investigation, resources, writing-review & editing.
ACKNOWLEDGMENTS
We thank participants for their participation in this study.
FUNDING INFORMATION
This study was supported by the Research Grants Council of the Hong Kong Special Administrative Region, China (Project number: 17606523).
CONFLICT OF INTEREST STATEMENT
The authors declared no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.





