Arm Dimensions of Patients with Obesity and Their Experiences with Blood Pressure Measurement: An Observational Study
Abstract
Objective
In patients with obesity, it was determined what proportion had an arm slant angle (SA) < 83° and which measure best predicted arm conicity. Patient experience with noninvasive blood pressure measurement was evaluated.
Methods
Arm SA was calculated from arm measurements. Linear regression determined whether BMI, weight, or right midarm circumference (MAC) best predicted conicity. Patient experiences were evaluated by survey and conventional content analysis of free-text comments.
Results
One hundred participants had a median (interquartile range; range) BMI of 44.1 (39.1-53.1; 31.1-80.8). Thirty-three (33%) had a right arm SA < 83°. Seven (7%) had a right MAC outside the recommended range. BMI, weight, and the right MAC showed low correlation with and explained little of the variation (with age and sex adjustment) in right arm SA (r = −0.29, −0.27, −0.31; P = 0.003, 0.007, 0.002; R2 = 0.09, 0.08, 0.10). Forty-two (42%) reported noninvasive blood pressure measurement caused severe pain, and 30 (30%) reported skin damage. Themes identified in free-text responses were “problems with equipment,” “feelings and experiences,” and “concerns about accuracy.”
Conclusions
Current equipment is inadequate for patients with obesity based on MAC and conicity. Pain and skin damage contributed to negative experiences of these patients.
Study Importance
What is already known?
- ► Noninvasive blood pressure measurement is known to be challenging in patients with obesity.
What does this study add?
- ► Currently recommended equipment is inadequate for patients with obesity and the process of measurement can be unpleasant.
- ► Specific equipment is necessary for less painful and more accurate noninvasive blood pressure measurement in patients with obesity.
Introduction
Noninvasive blood pressure (NIBP) measurement is a crucial component of perioperative care (1, 2). People with obesity make up an increasing proportion of patients requiring anesthetic care for elective, emergency, and weight loss surgery (3). Accurate NIBP measurement in patients with obesity can be compromised because of the size and shape of their arms (4). This may adversely affect their perioperative care (5).
The American Heart Association (AHA) provides recommended NIBP cuff sizes according to the midarm circumference (MAC) (6). The maximum arm circumference included in the AHA recommendation is 52 cm; however, there is an acknowledgement that the bladder and cuff sizes may differ according to manufacturer (6). Measurement inaccuracies can result if a cuff that is inappropriately small or inappropriately large is used (6, 7). An engineering study suggested that if significant amounts of adipose tissue are present over the brachial artery, very high cuff inflation pressures may be required for arterial compression (8).
An arm is described as conical if the upper arm circumference (at the axilla) is greater than the lower arm circumference (at the elbow). Increasing arm conicity, indicated by a decreasing arm slant angle, has been associated with NIBP measurement variation when comparing rectangular arm cuffs with tronco-conical arm cuffs (4). The largest measurement difference of up to 10 mm Hg was observed when the arm slant angle was < 83°. In conical arms (4), the bladder within the NIBP cuff tends to inflate and exert uneven pressure over the brachial artery (9). Palatini et al. (10) demonstrated that when cylindrical cuffs were used in people with cone-shaped arms, there was a greater discrepancy between the pressure inside the cuff and that exerted on the arm. While conical cuffs have been presented in the scientific literature (4, 11), rectangular cuffs remain the most widely used. Anecdotally, patients with obesity have reported significant pain from NIBP measurement; however, this has not been formally evaluated.
Other available alternatives to arm NIBP measurement in patients with obesity include invasive measurement and noninvasive monitors applied to the wrist or finger (5, 12, 13). ClearSight (Edwards Lifesciences Corp.) and CNAP (CNSystems Medizintechnik GmbH) are two such devices using finger cuffs, with limited evaluation in patients with obesity (5). The ability to predict which patients will have cone-shaped arms and therefore have inaccurate NIBP measurement may assist clinicians in selecting alternative blood pressure monitoring techniques and postoperative destination (e.g., critical care areas permitting invasive arterial monitoring).
We measured the size and shape of the arms and fingers of patients with obesity presenting to the Bariatric Surgery Outpatient Clinic to answer the following questions: what proportion of patients have a MAC outside the recommended cuff size range; what proportion of patients have a slant angle < 83°; what proportion of patients have fingers outside the cuff size range of ClearSight and CNAP; and can BMI, weight, or right MAC be used to predict arm conicity defined by the slant angle? In addition, we aimed to report the experience of these patients in having their blood pressure measured by using survey questions and free-text responses.
Methods
This manuscript adheres to STROBE (Strengthening the Reporting of Observational studies in Epidemiology) guidelines. This single-site observational study was undertaken in the Royal Brisbane and Women’s Hospital, Australia. Ethics approval was provided by the Human Research Ethics Committee of the Royal Brisbane and Women’s Hospital (HREC/2018/QRBW/46657), and the study was performed according to the Declaration of Helsinki. Participants were recruited from the Bariatric Surgery Outpatient Clinic and were eligible if they had BMI > 30, were aged ≥ 18 years, provided written informed consent, and were able to complete a short questionnaire in English. The clinic undertakes preoperative assessments and postoperative reviews for a range of surgical procedures.
BMI was calculated from the weight in kilograms and the height in meters squared, measured on the day of recruitment. Other data collected included age, sex, ethnicity, current diagnosis of hypertension, current or previous diagnosis of ischemic heart disease, and current use of antihypertensive medications.
Arm and finger measurements were taken from the right and left arms, by trained operators, using a standard medical measuring tape. Measurements were taken according to standard anthropometric measurements (14). Two measurements of arm length were obtained. Arm length A was measured with the participant standing with the elbow flexed and held by the side on the posterior aspect of the arm. The length was measured from the uppermost edge of the posterior border of the spine, extending from the acromion process to the olecranon process (14). At the midpoint of arm length A, the MAC was measured. With the participant standing and the arm hanging loosely by the side, arm length B (a nonstandard measurement) was obtained, measured on the medial aspect of the arm from the axilla to the antecubital fossa (11). This measurement was obtained in order to calculate the slant angle of the arm in the area in which a NIBP cuff is usually placed. With the arm remaining by the side, the proximal arm circumference (nonstandard measurement) was obtained at the axilla, and the distal arm circumference (nonstandard measurement) was obtained just above the elbow crease. These nonstandard measurements were used in the calculation of the slant angle. The finger circumference (nonstandard measurement) was measured at the midpoint of the middle phalanx of the middle finger, with the hands resting on a table.
The right MAC values were compared with the recommended cuff sizes (according to the MAC measurement) (6). The right finger circumference values were compared with the largest available ClearSight and CNAP finger cuff sizes. Mathematically, the section of the arm where a NIBP cuff is placed has been treated as a truncated cone (or “frustum”) (4, 11). The slant angle is the angle created between the slant of the cone and the base with the largest circumference (the upper arm circumference at the axilla). Thus, as the arm becomes more conical, the slant angle becomes smaller. The slant angle (in degrees) was calculated using the formula used by Palatini et al. (4) as follows: slant angle = arccosine ([C1 − C2] / [2π×L]) × (360/2π), in which C1 is the proximal arm circumference, C2 is the distal arm circumference, and L is arm length B.
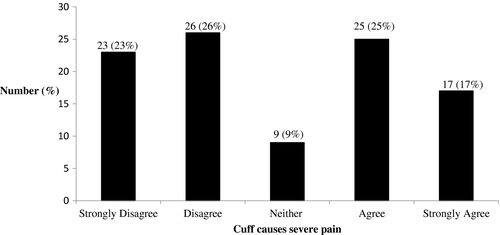
Participants were asked to identify, on an image of the human body, where in their experience the NIBP cuff was usually placed. They were asked whether they had ever experienced invasive arterial monitoring before. If so, participants were asked to respond on a 5-point Likert scale to the statement: “Blood pressure monitoring with a needle caused severe pain.” Severe pain was defined as worse than 7/10, and available responses were “strongly agree,” “agree,” “neither agree nor disagree,” “disagree,” or “strongly disagree.” Participants were asked to respond to the statement: “the arm cuff causes severe pain,” using the same definition of severe pain and responding on the same Likert scale. Participants were asked to respond to the statement: “the arm cuff has caused visible damage to my skin,” with the options “never,” “sometimes,” or “always” and, if answered in the affirmative, to describe the visible damage. Presentation of survey questions is shown in Supporting Information Figure S1. There was no missing data.
The sample size for this study was one of convenience. Participant characteristics were summarized using range with mean and SD or median and interquartile range for continuous variables (based on their distribution) and number and percent for categorical variables. Independent t tests were used to test for differences in arm measurements between males and females, and paired t tests were used to test for differences in arm measurements between left and right arms. The association between right arm slant angle and BMI, weight, and right MAC was explored using Pearson correlation coefficients. Right arm slant angle was modeled using linear regression. Separate models were created for BMI, weight, and right MAC, each adjusted for age and sex. The R2 values of these three models were compared to identify the anthropometric measure that best explained the variance in right arm slant angle. A statistical significance threshold was set at α < 0.05. Data were analyzed using Stata Statistical Software version 15 (StataCorp LLC, College Station, Texas). Responses to the survey questions were reported as number (percent) and presented as frequency histograms.
In the final free-text response, participants were asked, “Is there anything else you would like to tell us about your experience of having your blood pressure measured?” Responses were transcribed verbatim. Two experienced anesthetists (AT, VE), one with experience of qualitative research (VE), independently applied conventional content analysis (15) to interpret the data. After initial coding, the themes and concepts were identified by consensus, together with count data and illustrative quotes.
Results
One hundred participants were recruited between November 2018 and May 2019. They had a mean (SD) age of 48.5 years (12.7) and a median (interquartile range; range) BMI of 44.1 (39.1 to 53.1; 31.1 to 80.8), 75 (75%) were female, and 90 (90%) were Caucasian. Table 1 shows the indication for clinic attendance, comorbidities, and arm and finger measurements. Of the 25 participants prescribed antihypertensive medication, 12 (48%) were prescribed one medication, 9 (36%) prescribed two medications, and 4 (16%) were prescribed ≥ 3 medications. The mean (SD, range) right MAC was 42.0 cm (6.1, 30.9 to 59.6), and right slant angle was 84.0° (2.9°, 75.1° to 95.8°). Seven (7%) participants had a right MAC ≥ 52 cm and 33 (33%) had a slant angle < 83°. Nine (9%) participants had a right middle finger circumference > 6.8 cm (outside the range of the largest ClearSight finger cuff). No participants had a right middle finger circumference larger than the available CNAP finger cuff. There was no difference in the MAC or slant angle between the right and left arms. The mean MAC difference was 0.20 cm (95% CI: −0.25 to 0.65; P = 0.38), and mean slant angle difference was 0.11° (−0.18 to 0.40; P = 0.46). There was no difference between males and females in terms of the right MAC, with a mean difference of −0.25 cm (−3.60 to 3.11; P = 0.88), and there was no difference in terms of right slant angle, with a mean difference of 0.25° (−0.81 to 1.31; P = 0.64).
| Characteristic | n (%) | |
|---|---|---|
| Reason for clinic attendance | ||
| Preliminary assessment | 15 (15) | |
| Preoperative weight loss surgery | 42 (42) | |
| Postoperative review | 27 (27) | |
| Other | 16 (16) | |
| Diagnosed ischemic heart disease | 12 (12) | |
| Current diagnosis of hypertension | 32 (32) | |
| Recommended NIBP cuff size a | ||
| Standard 27-34.9 cm | 11 (11) | |
| Large 35-44.9 cm | 61 (61) | |
| Thigh 45-51.9 cm | 21 (21) | |
| ≥ 52 cm | 7 (7) | |
| BMI category, kg/m2 | n (%) | Slant angle, mean (SD) |
| 30-39.9 | 32 | 84.6 (2.4) |
| 40-49.9 | 34 | 84.3 (3.0) |
| 50-59.9 | 23 | 83.4 (3.1) |
| ≥ 60 | 11 | 82.2 (2.5) |
- According to American Heart Association and based on midarm circumference.
- NIBP, noninvasive blood pressure.
Each of the explanatory variables had low negative correlations with the right slant angle as indicated by correlation coefficients of 0.29 for BMI (P = 0.003), 0.27 for weight (P = 0.007), and 0.31 (P = 0.002) for right MAC. Table 2 shows the regression models between the outcome of right slant angle and BMI, weight, and right MAC, each adjusted for age and sex. These adjusted models explained 10% or less of the variation in the conicity of the arm. Models not adjusted for age and sex (not shown) produced similar results (adjusted R2 0.08 for BMI, 0.06 for weight, and 0.09 for right MAC).
| Regression modelsa outcome: right slant angle | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||
| β (95% CI) | P | β (95% CI) | P | β (95% CI) | P | |
| BMI | −0.08 (−0.14 to −0.02) | 0.009 | ||||
| Weight | −0.03 (−0.05 to −0.005) | 0.017 | ||||
| Right MAC | −0.14 (−0.23 to −0.04) | 0.004 | ||||
| Age | 0.02 (−0.03 to 0.06) | 0.49 | 0.01 (−0.04 to 0.06) | 0.70 | 0.02 (−0.03 to 0.06) | 0.39 |
| Sex (male) | −0.14 (−1.44 to 1.16) | 0.83 | 0.39 (−1.06 to 1.84) | 0.59 | −0.31 (−1.59 to 0.97) | 0.63 |
| Intercept | 86.87 (82.95 to 90.79) | < 0.001 | 86.70 (82.60 to 90.81) | < 0.001 | 88.80 (83.99 to 93.62) | < 0.001 |
| R 2 | 0.09 | 0.08 | 0.10 | |||
| Adjusted R2 | 0.06 | 0.05 | 0.07 | |||
- Adjusted for age and sex.
The arm was reported as the most common NIBP cuff location in 90 participants (90%), with 10 (10%) reporting most common placement on the forearm. Fifteen (15%) had previously experienced invasive blood pressure monitoring. Of those 15, 7 (47%) agreed or strongly agreed that “blood pressure monitoring with a needle caused severe pain,” whereas 6 (40%) disagreed or strongly disagreed, and 2 responded “neither agree nor disagree.” Figure 1 shows participant responses to the following statement: “The arm cuff causes severe pain (worse than 7/10).” Thirty (30%) participants reported visible skin damage from the NIBP cuff as “sometimes” or “always.” Bruising was reported by 23 participants and persistent red marks on the skin by 7 participants.
Of the 100 participants, 45 (45%) provided free-text comments; of those, 8 (17.8%) reported no problems with blood pressure measurement. Table 3 shows the identified themes and concepts within the free-text responses with illustrative quotes.
| Concept | Theme | Example |
|---|---|---|
| Cuffs are not a suitable size | Problems with equipment |
“Often the clinic doesn’t have a large enough cuff easily accessible so they can’t get a reading.” (PE22)a “Can they make a device that doesn’t hurt as much?” (PE84) |
| Correct cuffs are not available | ||
| Equipment malfunction/repeated measurements | ||
| Seeking alternatives to current equipment | ||
| Negative experiences because of pain/bruising | Patient feelings and experiences |
“The really painful times are caused by automatic machines and I have to rip the cuff off because it hurts so much.” (PE71) “The measurement is more accurate on the forearm, so I encourage people to measure on my forearm, but they don't always listen. (PE53) “Everything is generally easy.” (PE2) |
| Negative interactions with staff not knowing what to do | ||
| Positive experience with no problems | ||
| Perceived inaccuracy because of inappropriate cuff size | Concerns about accuracy of blood pressure readings |
“Most of the time my blood pressure needs to be measured more than once because of a machine error or wrong cuff size.” (PE84) “[Automated] machines measure high, but the old school manual measurements are all normal.” (PE77) |
| Perceived inaccuracy depending on whether manual or automated technique used |
- PE22 indicates unique participant identifier.
Discussion
Our study demonstrates limitations in the current equipment available for NIBP measurement and the recommendations regarding NIBP cuff size in patients with obesity. In this cohort, 7% of participants had a right MAC outside of the recommendations made by the AHA (6). Based on the arm conicity and the previous findings of Palatini et al. (4), it is likely that one-third of participants would have erroneous measurements based on the slant angle of their arm. When considering finger cuff devices as an alternative, 9% of our small cohort had a finger circumference that was outside the “large” ClearSight cuff. While all our participants would be suitable for the CNAP device based on the largest finger cuff size, 59% had a right MAC that was too large for the arm NIBP cuff that is required to calibrate the CNAP device. While the right MAC was identified as the best of three potential predictors of arm conicity, all three showed a low correlation with conicity. The regression models, after adjustment for age and sex, explained 10% or less of the variation observed in arm conicity. None of these measures adequately described the variable distribution of adipose tissue in patients with obesity. Our results are important, as they highlight the practical limitations in following NIBP measurement recommendations in a population of patients with obesity.
To our knowledge, our study is the first to specifically report on patients’ perspectives of NIBP measurement in a population of people with obesity. Nearly half reported experiencing severe pain from the NIBP cuff, with visible damage reported in one-third. Use of the forearm as the cuff location occurred in a smaller fraction of patients. Major themes identified in the free-text responses identified problems with the availability of appropriate equipment, negative experiences of pain with cuff inflation, and concerns about the accuracy of equipment.
Guidelines on NIBP measurement (6) and device validation (16) have recognized limitations when applied to people with obesity. As we have demonstrated, the recommended cuff sizes originally published by the AHA (17) and widely referenced since (6, 18, 19) do not accommodate the small fraction of patients with obesity who have an arm circumference greater than 52 cm. There have been three main bodies guiding the validation of NIBP measurement devices, which include the British Hypertension Society (most recently published 1993) (20), the European Society for Hypertension (updated in 2010) (16), and the Association for the Advancement of Medical Instrumentation (AAMI) (updated 2013) (21). Only the AAMI guideline provides strict recommendations regarding the inclusion of participants with specific arm measurements in validation studies. These limitations were highlighted in a 2018 statement by the AAMI and European Society for Hypertension proposing a universal validation protocol, which specifies the distribution of arm circumference to be included in validation populations, depending on the specifications of the device (22). This means that if a device is recommended for patients with a MAC greater than 52 cm, then patients with arms of this size must be included in the validation study.
While the limited range of cuffs according to the MAC has been recognized, the role of arm shape, or conicity, has only recently been addressed in measurement recommendations of the AHA (6), and it is not incorporated into validation protocols (16, 20, 21). However, it is increasingly appreciated as a significant problem in clinical practice (9, 23-25). The AHA recommendations now support the use of tronco-conical cuffs in people with cone-shaped arms (6). The limited evaluations published on the use of tronco-conical cuffs in people with obesity have found that they provide lower blood pressure measurements when compared with standard rectangular cuffs (4). Tronco-conical cuffs have not been adopted widely in Australia. “Wide-range devices” couple a smaller cuff bladder size with a software algorithm and may cater to a larger range of arm circumferences; however, both tronco-conical cuffs and wide-range devices require evaluation in large and diverse populations (9).
Consideration should be given to the possibility that significant variation in arm morphology across the BMI categories may preclude the arm as the ideal site of blood pressure measurement in patients with obesity. Our results highlight the fact that currently available devices using alternate sites, such as the finger, do not adequately cater to all patients who have obesity either. The largest finger cuff supplied by ClearSight was not large enough for all our patients, and this failure also was demonstrated in a pregnant population (26). While the sizes of the finger cuffs supplied with the CNAP device are ample, the device requires the use of a NIBP arm cuff for calibration. Designed for a MAC up to 40 cm, this arm cuff significantly reduces the utility of this device in people with a large arm circumference. Based on the results of a 2016 meta-analysis (27), the latest AHA recommendations (6) suggest placing arm cuffs on the wrist, with auscultation of the radial artery, when a thigh-sized cuff does not fit the arm adequately.
People with obesity are known to experience obesity stigma (28), and this has been reported in different health care contexts (29-31). Our results on the participant experience of blood pressure measurements are unique in that they focus on a frequently performed assessment from both physical and emotional perspectives. Our participants were aware of repeated measurements, cuff dysfunction, and different readings provided by different equipment. In this population, who are at risk of cardiovascular disease, health care engagement is critical. The combination of a painful experience and a lack of confidence in blood pressure measurements could have negative consequences on their overall health care engagement and literacy. This is particularly unfortunate, given that weight loss surgery has been demonstrated to result in short- and long-term reductions in blood pressure in people with obesity (32).
Our study has limitations. As an exploratory study, the sample size was one of convenience. With approximately 300 patients undergoing bariatric surgery annually in our hospital, our sample makes up around a third of the baseline bariatric surgical population. While we have provided a detailed characterization of the size and shape of our participants’ arms, we did not actually measure their blood pressure or their skinfold thickness. Our cohort included more females than males, which may present selection bias. Our findings are not generalizable to older and potentially more medically complex patients with obesity. Our use of the cutoff for slant angle < 83° was based on work by Palatini et al. (4, 9), who compared NIBP readings from a rectangular cuff with those from a tronco-conical cuff rather than with measurements from the gold standard invasive arterial monitoring.
Conclusion
We have identified that current NIBP cuff equipment and measurement recommendations accommodate many but not all patients with BMI > 30. Alternatives such as available finger cuffs are also inadequate in design for this population. In addition, the NIBP measurement was shown to be largely a negative experience for nearly half of this small sample, who experienced pain and had concerns about inaccurate measurements. Our results suggest a need for specific equipment tailored to patients with obesity. Future research will focus on a practical anthropometric predictor of which patients with obesity are most at risk for inaccurate NIBP measurements.
Disclosure
The authors declared no conflict of interest.
Author contributions
PC, KL, and CC contributed to data collection, data interpretation, and writing of the manuscript; AP contributed to quantitative data analysis, data interpretation, and writing of the manuscript; AT contributed to qualitative data analysis, data interpretation, and writing of the manuscript; VE contributed to protocol design, ethics application, qualitative analysis, data interpretation, and writing of the manuscript.





