The WORD: Outcomes of a Behavioral Weight Loss Maintenance Effectiveness Trial in Rural Black Adults of Faith
Abstract
Objective
Rural black communities bear a disproportionate burden of obesity. To increase reach among underserved groups, community-based weight loss and maintenance interventions are crucial.
Methods
The Diabetes Prevention Program (DPP) was adapted for rural black adults of faith to create The Wholeness, Oneness, Righteousness, Deliverance (WORD) trial, a group-based, community health worker–delivered weight loss intervention. A Weight Loss Only arm (16 sessions) was compared with a Weight Loss + Maintenance arm (16 + 12 sessions) in a cluster randomized controlled trial of 31 churches (n = 440). Weight and related behaviors were assessed at 0, 6, 12, and 18 months.
Results
The WORD produced weight loss from baseline to 6 months (percentage body weight change −2.47 [−3.13 to −1.80]). Among those who lost 5% of their baseline weight, there was a statistical trend of lower weight regain in the Weight Loss + Maintenance arm compared with control. Maintenance arm participants reported higher activity at 12 months. There were no between-arm differences at 18 months.
Conclusions
The WORD produced weight loss from baseline to 6 months on par with that produced by other DPP adaptations for black communities, including adaptations using health professionals. Weight regain was also consistent with that reported in prior literature. Continuing sessions as part of the church’s mission may foster adoption of DPP-based weight loss programs.
Study Importance
What is already known?
- Black adults and rural residents bear a disproportional burden of the obesity epidemic.
- Weight loss maintenance is critical to sustain the beneficial effects of weight loss on health.
- The Diabetes Prevention Program (DPP) has been successfully translated for clinic- and university-based settings to produce weight loss in diverse adults.
What does this study add?
- The study ascertains the extent to which the DPP can be successfully translated in community settings to produce and sustain weight loss in underserved groups such as rural black adults.
- The study used community health workers in translating the DPP for underserved groups.
- The study engaged faith-based networks to deliver the DPP for sustained weight loss using a rigorous randomized controlled trial design.
Introduction
The obesity epidemic affects all segments of the population, with approximately 69% of adults having overweight or obesity (1, 2). Obesity is highest among black adults at 48.1%, compared with 34.5% for white adults (2). This epidemic also disproportionately affects rural residents and communities of low socioeconomic status (3), resulting in significant health disparities. Halting the obesity epidemic through identification and implementation of effective community-based interventions is a prominent research focus.
The beneficial health effects of weight loss are well documented (4, 5). However, although evidence-based behavioral lifestyle interventions promote weight loss in the short term (6 months) (5-7), weight regain typically occurs within 1 to 3 years (5, 8). Thus, understanding the necessary conditions that support weight loss maintenance, particularly in rural and black populations, is essential for reducing obesity and associated disparities in this high-risk group.
The majority of weight loss maintenance studies focused on black adults have been conducted in clinic or academic settings (9). Some have reported success in weight loss maintenance, but these interventions have limited reach among those at highest risk, namely rural, underserved minorities with health care access barriers. To improve the reach of evidence-based weight loss maintenance interventions, effectiveness trials in community settings are needed.
Prior obesity interventions targeting underserved groups have reported the importance of considering multiple sociocultural factors that influence weight outcomes. In this respect, integration of a community-based participatory research (CBPR) approach in the context of faith communities to address unhealthy weight has been reported (10, 11), and smaller church-based trials using community health workers (CHWs) have resulted in weight change (12, 13). The geographic and social placement of churches in black and rural communities offers accessible venues for dissemination of community-based obesity interventions (14). Previous community effectiveness trials of obesity-related health behaviors have been successful in testing and facilitating the dissemination of evidence-based interventions, such as the Body and Soul project that was adopted by National Cancer Institute for national dissemination to increase fruit and vegetable intake among black communities of faith (15-17). Little is known, however, about the impact of models that integrate a CBPR approach in faith-based settings on weight loss maintenance, using empirically based obesity interventions.
The Wholeness, Oneness, Righteousness, Deliverance (WORD) trial used community- and faith-based infrastructures and adapted the Diabetes Prevention Program (DPP) to examine longer-term weight outcomes in black churches in the rural Arkansas Delta.
This paper reports on the primary outcome of weight loss maintenance and on secondary outcome changes in diet and physical activity at 12 and 18 months. The overall goal is to contribute to the evidence concerning weight loss maintenance and obesity reduction among black residents living in rural communities, particularly given the disproportionate burden of obesity both black and rural residents bear.
Methods
The WORD was a cluster randomized controlled trial that tested the effectiveness of a DPP-adapted intervention on weight loss maintenance using a CBPR approach (18). The trial spanned 18 months, with rural black churches randomly assigned to either 6 months of behavioral treatment for weight loss followed by weight loss maintenance for 12 months (Weight Loss + Maintenance) or 6 months of behavioral weight loss treatment followed by 12 months of assessment only (Weight Loss Only). The study was funded by the National Institute on Minority Health and Health Disparities, approved by the University of Arkansas for Medical Sciences Institutional Review Board, and registered at ClinicalTrials.gov (NCT02169947). Methods have been detailed previously (18).
The trial entailed a community subcontract whereby the Community Principal Investigator and his colleagues engaged their faith-based networks across the Arkansas Delta to recruit churches. Church eligibility criteria included being a black church in the Arkansas Delta. CHWs were recruited from participating churches to deliver the intervention and were responsible for advertising the study to potential participants using flyers, church bulletins, announcements from the pulpit, and word of mouth. CHW eligibility criteria included being associated with a participating church and an interest in health promotion, which were assessed by self-report. Participant eligibility criteria included having overweight or obesity and being black, 18 years or older, and associated with a participating church (detailed eligibility criteria published previously) (19). All materials were cocreated by community and academic investigators. A total of 31 churches, 61 CHWs, and 440 participants were recruited.
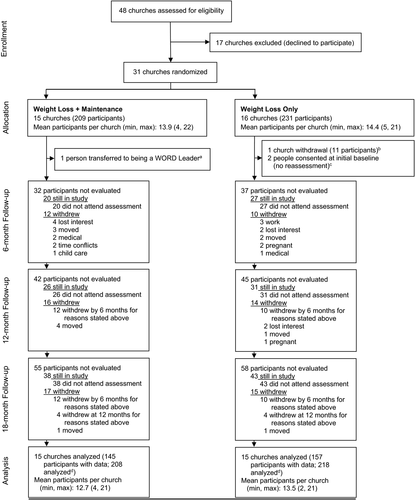
Figure 1 shows the flow of churches and participants through the study from initial eligibility assessment through 18-month follow-up.
Interventions
The DPP (20) was adapted using information from 2 previous pilots KHKY conducted with rural black faith communities (18, 21). The WORD shares components of the DPP, including program goals (i.e., 7% loss of initial body weight, 9 to 12 servings of fruit and vegetables a day, 2 to 3 servings of low-fat dairy a day, half of all starches as whole grains, 150 minutes of moderate physical activity a week); an emphasis on self-monitoring through recording weight, eating, and exercising daily; and didactic instruction to facilitate goal setting and problem solving. The WORD differs from the DPP by (1) delivering the intervention in a church setting, (2) using a small group format, and (3) training CHWs to deliver the intervention. Study staff delivered an initial 28-hour training over 4 to 6 weeks to CHWs, who received certification after passing a written examination. The initial training was then followed by booster sessions throughout intervention implementation, during which study staff assessed CHW intervention fidelity. The WORD also differs from the DPP by integrating spiritual beliefs in the curriculum for cultural appropriateness. More details regarding The WORD curriculum have been reported previously (18).
Participants who were nested within churches randomly assigned to the Weight Loss Only condition attended 16 group meetings that were held weekly for 1.5 to 2 hours over 6 months in their participating church. CHWs led sessions, which included a 40-minute behavioral module focused on making dietary and physical activity changes by drawing on strength from one’s faith, followed by a Bible study and on-site physical activity for 30 minutes.
In addition to the 6-month intervention given to Weight Loss Only participants, participants nested within churches randomly assigned to the Weight Loss + Maintenance condition continued to meet monthly for 12 months after the Weight Loss Only intervention ended. Maintenance sessions lasted approximately 1 hour and encouraged participants to continue practicing strategies associated with weight maintenance in the context of connecting faith with health. The on-site 30 minutes of physical activity after the didactic component was also continued.
Measurements
Trained study staff blinded to treatment condition collected participant data at baseline and 6, 12, and 18 months at the church where the participants' intervention group met. Weight and height data were collected individually in a private area, and the survey was self-administered in a group setting.
Sociodemographic factors were assessed by self-report and included gender, age, education, marital status, income, and employment status.
Percent change in weight was assessed between 6 and 12 months and between 6 and 18 months. Participants were weighed to the nearest 0.5 lb (0.2 kg) using a calibrated digital scale. Height (without shoes) was measured to the nearest 0.5 cm using a stadiometer. Weight and height were used to compute a continuous measure of BMI (kilograms per meter squared) (22).
Health behaviors were secondary end points. Dietary intake was assessed with the 2011 Behavioral Risk Factor Surveillance System fruit and vegetable consumption and sugar-sweetened beverage intake measures (23) and the Fat- and Fiber-related Diet Behavior Questionnaire (24). Physical activity was assessed using an adapted version of the Paffenbarger Physical Activity Questionnaire (25).
Statistical analysis
Linear mixed models were used to check for a difference between the treatment groups, accounting for within-church clustering, for both the primary outcome and the secondary outcomes. The fixed effects in the models were treatment arm (i.e., Weight Loss Only, Weight Loss + Maintenance) and, as applicable, a baseline covariate and/or a 6-month covariate corresponding to the outcome variable to adjust for any baseline and 6-month differences. The random effect in the models was church site, and the chosen covariance structure was variance components. Fit by restricted maximum likelihood was implemented in SAS PROC MIXED, a powerful method that can accommodate complex covariance structures. This method is also robust to moderate departures from multivariate normality (26). All analyses were generated using SAS version 9.4 (SAS Institute, Cary, North Carolina).
In accordance with the intention-to-treat principle, multiple imputation was implemented under the missing-at-random assumption and carried out using SAS PROC MI, in which 30 imputations were performed using Markov chain Monte Carlo methodology in which a separate chain was used for each imputation. Both the variables that were used to create the outcome variables and the predictor variables that were used in the models were included in the variable list in PROC MI and were thus imputed if missing values occurred for any of those variables. If an imputed value was out of bounds for a certain variable, then either the smallest or largest plausible value for that variable was used as the imputed value. Pertaining to the primary outcome, the percentages of missingness for body weight at baseline, 6 months, 12 months, and 18 months were 0%, 16.2%, 20.4%, and 26.5%, respectively. In addition, a sensitivity analysis was performed to explore similarity in outcomes when conducting the analysis based on participants who were and were not lost to follow-up. The significance of the primary analysis was maintained in the corresponding sensitivity analysis. The results presented are based on multiple imputation.
Sample size calculations were based on the primary outcome of weight change (kilograms) from 6 months to 18 months (weight maintenance). Data from The WORD pilot were used to estimate the power calculations (18). With an overall sample size of 450 participants (15 churches per group, 15 individuals per church) after adjusting for a 20% attrition rate, the study had 85% power to detect a difference of 2 kg between the group means at 18 months when the SD was 5.5 kg and the intracluster correlation was 0.02 using a 2-sample, cluster t test with a significance level of 0.05.
Results
Participant characteristics
A total of 440 participants were enrolled by the 31 participating churches. Churches that participated in the intervention ranged in size from less than 25 to more than 150, with 36.7% with 50 or fewer members, 26.7% with 51 to 100 members, and 36.7% with 101 or more members. Table 1 reports participant characteristics by arm. Participants were predominantly female (93.0%) and employed (72.2%), with a mean age of 49.8 (SD = 12.8) years and a mean baseline BMI of 37.2. About half reported being married or a member of an unmarried couple (47.1%), having a high school degree or less (51.1%), and having an income of less than $35,000 (53.2%). There were no significant differences between arms in demographic characteristics or in weight at baseline or at 6 months before treatment of the study arms diverged.
| Total sample (n = 426) | Weight Loss Only (n = 218) | Weight Loss + Maintenance (n = 208) | P valuea | |
|---|---|---|---|---|
| Female | 396 (93.0%) | 206 (94.5%) | 190 (91.3%) | 0.2655 |
| Age (y) | 49.8 (12.8) | 50.5 (12.2) | 49.1 (13.3) | 0.5735 |
| Marital status | 0.8754 | |||
| Married or member of an unmarried couple | 189 (47.1%) | 101 (48.3%) | 88 (45.8%) | |
| Previously married | 118 (29.4%) | 61 (29.2%) | 57 (29.7%) | |
| Never married | 94 (23.4%) | 47 (22.5%) | 47 (24.5%) | |
| Education | 0.1917 | |||
| Less than high school | 19 (4.7%) | 8 (3.8%) | 11 (5.7%) | |
| High school or GED | 187 (46.4%) | 88 (41.9%) | 99 (51.3%) | |
| College or some college | ||||
| Associate's degree | 144 (35.7%) | 75 (35.7%) | 69 (35.8%) | |
| More than bachelor's degree | 44 (10.9%) | 32 (15.2%) | 12 (6.2%) | |
| Other degree | 9 (2.2%) | 7 (3.3%) | 2 (1.0%) | |
| Income | 0.1867 | |||
| Less than $20,000 | 116 (30.0%) | 55 (27.5%) | 61 (32.6%) | |
| $20,000-$34,999 | 90 (23.3%) | 44 (22.0%) | 46 (24.6%) | |
| $35,000-$49,999 | 66 (17.1%) | 31 (15.5%) | 35 (18.7%) | |
| $50,000 or more | 115 (29.7%) | 70 (35.0%) | 45 (24.1%) | |
| Employment | 0.2289 | |||
| Employed | 288 (72.2%) | 159 (76.8%) | 129 (67.2%) | |
| Unemployed | 33 (8.3%) | 16 (7.7%) | 17 (8.9%) | |
| Retired or unable to work | 78 (19.6%) | 32 (15.5%) | 46 (24.0%) | |
| BMI (baseline) | 37.2 (8.2) | 36.7 (7.7) | 37.8 (8.6) | 0.2555 |
| BMI (6 mo) b | 36.2 (8.2) | 35.5 (7.4) | 36.9 (8.8) | 0.1787 |
| Weight (baseline), kg | 100.0 (22.7) | 98.1 (21.4) | 102.1 (23.8) | 0.1360 |
| Weight (6 mo), kg c | 97.2 (22.3) | 94.7 (20.6) | 99.9 (23.8) | 0.0958 |
- Multiple imputation not used for this table.
- a P values take into account clustering in study.
- b Weight Loss Only (n = 181); Weight Loss + Maintenance (n = 175).
- c Weight Loss Only (n = 181); Weight Loss + Maintenance (n = 176).
- GED, general equivalency diploma.
Changes in weight and related behaviors from baseline to 6 months
From baseline to 6 months, participants in both arms lost weight, reduced their BMI, and made significant changes in dietary and physical activity behaviors (Table 2). A total of 23.7% of all participants lost at least 5% of their baseline weight by 6 months. There were no significant differences between the arms in weight or BMI changes during core. The only between-arm differences in behaviors from baseline to 6 months were in substitution of high-fiber for low-fiber foods (P = 0.04), with the Weight Loss + Maintenance arm reporting more such substitutions than the Weight Loss Only group, and in recreational physical activity (P = 0.03), with the Weight Loss Only arm reporting significantly more Metabolic Equivalent of Tasks (METS) expended in recreational physical activity compared with the Weight Loss + Maintenance group. Because both arms received the same intervention during this initial 6-month study period, differences between the study arms were not expected, and the few differences that were significant may have been due to chance. Thus, for 12- and 18-month analyses, the 6-month values were treated as the “new baseline” for examining differences between the arms during maintenance, and subsequent analyses were adjusted for 6-month values.
| Mean change from baseline to 6 mo (95% CI)a | P valueb | |||
|---|---|---|---|---|
| Weight Loss Only (n = 218) | Weight Loss + Maintenance (n = 208) | Combined (n = 426) | ||
| Percent body weight change | −2.53 (−3.48 to −1.58) | −2.39 (−3.34 to −1.45) | −2.47 (−3.13 to −1.80) (< 0.0001) | 0.8367 |
| Body weight, kg | −2.63 (−3.62 to −1.64) | −2.45 (−3.45 to −1.46) | −2.54 (−3.24 to −1.84) (< 0.0001) | 0.8045 |
| BMI | −0.99 (−1.34 to −0.65) | −0.89 (−1.23 to −0.54) | −0.94 (−1.19 to −0.70) (< 0.0001) | 0.6611 |
| Total fat (frequency of substitution for lower fat; 1 = none, 5 = very often) | 0.41 (0.31 to 0.51) | 0.47 (0.37 to 0.57) | 0.44 (0.37 to 0.51) (< 0.0001) | 0.4081 |
| Fat substitute | 0.64 (0.48 to 0.79) | 0.60 (0.44 to 0.76) | 0.62 (0.51, 0.73) (< 0.0001) | 0.7842 |
| Avoid fat | 0.05 (−0.10 to 0.19) | 0.15 (0.01 to 0.29) | 0.10 (−0.006 to 0.20) (0.0642) | 0.3074 |
| Modify meat | 0.48 (0.35 to 0.60) | 0.51 (0.38 to 0.64) | 0.49 (0.41 to 0.58) (< 0.0001) | 0.7067 |
| Replace fat | 0.37 (0.25 to 0.50) | 0.45 (0.32 to 0.57) | 0.41 (0.32 to 0.50) (< 0.0001) | 0.4447 |
| Replace meat | 0.27 (0.11 to 0.42) | 0.40 (0.25 to 0.56) | 0.33 (0.22 to 0.44) (< 0.0001) | 0.2212 |
| Total fiber (frequency of substitution for higher fiber; 1 = none, 5 = very often) | 0.38 (0.27 to 0.50) | 0.51 (0.39 to 0.63) | 0.44 (0.36 to 0.53) (< 0.0001) | 0.1490 |
| Grain | 0.40 (0.26 to 0.55) | 0.51 (0.36 to 0.66) | 0.45 (0.35 to 0.56) (< 0.0001) | 0.3058 |
| Fruit and vegetables | 0.42 (0.29 to 0.56) | 0.48 (0.34 to 0.61) | 0.45 (0.36 to 0.54) (< 0.0001) | 0.5882 |
| Subfiber | 0.32 (0.15 to 0.48) (0.0001) | 0.55 (0.39 to 0.70) (< 0.0001) | 0.42 (0.30 to 0.55) | 0.0411 |
| Fruit intake (frequency consumed) | 2.12 (0.86 to 3.38) | 1.33 (0.05 to 2.60) | 1.73 (0.84 to 2.62) (0.0001) | 0.3874 |
| Vegetable intake (frequency consumed) | 3.34 (0.56 to 6.12) | 3.53 (0.76 to 6.30) | 3.44 (1.51 to 5.36) (0.0005) | 0.9239 |
| Sugar-sweetened beverage intake (frequency consumed) | −2.90 (−4.06 to −1.73) | −3.38 (−4.57 to −2.19) | −3.13 (−3.96 to −2.31) (< 0.0001) | 0.5692 |
| Total physical activity (METS) | 8.79 (6.67 to 10.91) | 6.91 (4.70 to 9.13) | 7.87 (6.32 to 9.43) (< 0.0001) | 0.2262 |
| Recreational physical activity (METS) | 5.84 (4.40 to 7.28) (< 0.0001) | 3.62 (2.16 to 5.07) (< 0.0001) | 4.76 (3.67 to 5.84) | 0.0339 |
- Each P value is adjusted for respective baseline outcome.
- a Change calculated as applicable value at 6 months minus applicable value at baseline.
- b Each P value in this column is associated with a test to determine whether there is a significant difference between 2 intervention arms with respect to mean change from baseline to 6 months for corresponding outcome.
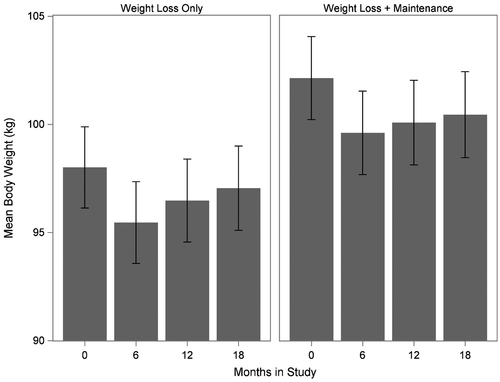
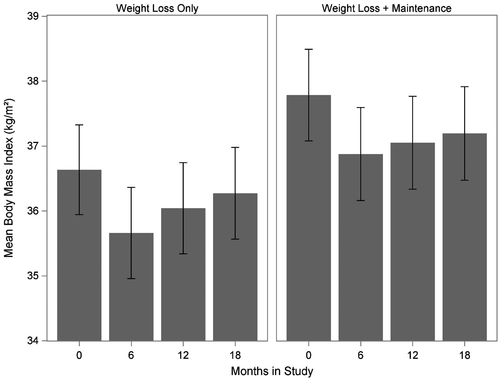
Maintenance results: body weight
After the first 6 months, Weight Loss + Maintenance participants continued to attend group sessions (now held monthly), whereas the Weight Loss Only group sessions ceased. Table 3 reports changes in weight and BMI variables during this maintenance period, adjusted for 6-month values. After another 6 months, participants in both study arms began to regain weight. Within-group analyses revealed that the weight regain from 6 to 12 months was statistically significant for the Weight Loss Only group and by 18 months, weight regain was significant for both groups. Between-group analyses indicated no significant differences in weight or BMI changes during the maintenance period. Figures 2-3 graphically show the general trend in the change in mean body weight and mean BMI, respectively, over the course of the study.
| Time point (relative to 6 mo) | Mean change from 6 mo (95% CI)a | P value | |||
|---|---|---|---|---|---|
| Weight Loss Only (n = 218) | Weight Loss + Maintenance (n = 208) | Difference between arms mean changes (95% CI)b | |||
| Percent body weight change (from baseline [6 mo]) | 12 mo | 1.12 (0.50 to 1.73) (0.0004) | 0.49 (−0.13 to 1.10) (0.1186) | 0.63 (−0.23 to 1.49) | 0.1522 |
| 18 mo | 1.67 (0.79 to 2.56) (0.0002) | 1.01 (0.09 to 1.93) (0.0324) | 0.66 (−0.65 to 1.98) | 0.3229 | |
| Body weight change (from baseline [6 mo]), kg | 12 mo | 1.04 (0.44 to 1.63) (0.0006) | 0.48 (−0.12 to 1.07) (0.1164) | 0.56 (−0.28 to 1.39) | 0.1894 |
| 18 mo | 1.58 (0.74 to 2.41) (0.0002) | 0.90 (0.04 to 1.77) (0.0408) | 0.67 (−0.57 to 1.91) | 0.2860 | |
| BMI | 12 mo | 0.38 (0.17 to 0.60) (0.0006) | 0.18 (−0.04 to 0.40) (0.1126) | 0.20 (−0.10 to 0.51) | 0.1902 |
| 18 mo | 0.60 (0.30 to 0.91) (0.0001) | 0.34 (0.02 to 0.66) (0.0362) | 0.26 (−0.19 to 0.72) | 0.2491 | |
- Each P value is adjusted for respective 6-month outcome only.
- a Change calculated as applicable value at 12 months minus applicable value at 6 months or applicable value at 18 months minus applicable value at 6 months, as appropriate.
- b Difference between arm mean changes calculated as applicable value for Weight Loss Only minus applicable value for Weight Loss + Maintenance.
Among participants who lost weight from baseline to 6 months, the majority remained under their baseline weight regardless of arm at 12 and 18 months. At 12 months, 77.3% (95% CI: 70.0% to 84.6%) of Weight Loss Only and 75.6% (68.1% to 83.1%) of Weight Loss + Maintenance participants remained under their baseline weight. At 18 months, 67.4% (59.1% to 75.6%) of Weight Loss Only and 65.9% (57.8% to 74.0%) of Weight Loss + Maintenance participants remained under their baseline weight.
Subgroup analyses examined weight regain in participants who lost at least 5% of their initial body weight during the initial 6 months of the study (Table 4). Although there was not a statistically significant between-group difference in weight regain from 6 to 12 months, there was a trend for participants in the Weight Loss Only arm to regain more weight between 6 and 12 months than participants in the Weight Loss + Maintenance arm, suggesting that weight regain may have been slower in the latter arm. However, by 18 months, there were no significant differences between the arms in weight regain.
| Time point (relative to 6 mo) | Mean change from 6 mo (95% CI)a | P value | |||
|---|---|---|---|---|---|
| Weight Loss Only (n = 57) | Weight Loss + Maintenance (n = 44) | Difference between arms mean changes (95% CI)b | |||
| Percent body weight change (from baseline [6 mo]) | 12 mo | 2.24 (0.76 to 3.72) (0.0032) | 0.67 (−0.87 to 2.21) (0.3904) | 1.57 (−0.47 to 3.60) | 0.1318 |
| 18 mo | 3.77 (1.84 to 5.71) (0.0002) | 4.02 (1.90 to 6.14) (0.0002) | −0.25 (−3.03 to 2.54) | 0.8618 | |
| Body weight change (from baseline [6 mo]), kg | 12 mo | 2.11 (0.86 to 3.36) (0.0010) | 0.61 (−0.72 to 1.94) (0.3689) | 1.50 (−0.21 to 3.22) | 0.0850 |
| 18 mo | 3.35 (1.70 to 5.00) (< 0.0001) | 3.65 (1.84 to 5.47) (< 0.0001) | −0.31 (−2.66 to 2.05) | 0.7984 | |
| BMI | 12 mo | 0.80 (0.32 to 1.27) (0.0011) | 0.26 (−0.25 to 0.76) (0.3189) | 0.54 (−0.11 to 1.19) | 0.1019 |
| 18 mo | 1.27 (0.65 to 1.89) (< 0.0001) | 1.37 (0.68 to 2.06) (0.0001) | −0.10 (−1.00 to 0.80) | 0.8271 | |
- Each P value is adjusted for respective 6-month outcome only.
- a Change calculated as applicable value at 12 months minus applicable value at 6 months or applicable value at 18 months minus applicable value at 6 months, as appropriate.
- b Difference between arm mean changes calculated as applicable value for Weight Loss Only minus applicable value for Weight Loss + Maintenance.
In the Weight Loss Only arm, participants regained by 18 months an average of 44.0% (22.6% to 65.4%; P < 0.0001), whereas participants in Weight Loss + Maintenance regained an average of 39.2% (16.5% to 61.9%; P = 0.0007). Most participants who lost at least 5% of their initial weight by 6 months remained under their baseline weight regardless of arm during maintenance. At 12 months, 97.8% (91.8% to 100.0%) of Weight Loss Only and 98.2% (92.9% to 100.0%) of Weight Loss + Maintenance participants remained under their baseline weight. At 18 months, 84.5% (73.6% to 95.4%) of Weight Loss Only and 88.0% (77.3% to 98.8%) of Weight Loss + Maintenance participants remained under their baseline weight.
Maintenance results: diet and physical activity
After weekly sessions ended at 6 months, improvements in diet and physical activity began to reverse in both arms (Table 5). For diet, within-group analyses showed changes in a negative direction (poorer dietary behaviors/outcomes) from 6 to 12 and from 6 to 18 months for both arms, with 11 of 13 changes in dietary variables reaching significance (P < 0.05) at 12 and/or 18 months for the Weight Loss Only arm. For Weight Loss + Maintenance, within-arm reversals in behavior reached significance at 12 months for fewer (6 of 13) dietary behaviors, but all changes except for sugar-sweetened beverage intake were in a negative direction by 18 months for this arm as well. Within-arm analyses for physical activity showed reversals in total and recreational activity, except at 12 months for total physical activity for the Weight Loss + Maintenance arm. There were significant reversals for Weight Loss Only at 12 months and for both arms by 18 months.
| Time point (relative to 6 mo) | Mean change from 6 mo (95% CI)a | P value | |||
|---|---|---|---|---|---|
| Weight Loss Only (n = 218) | Weight Loss + Maintenance (n = 208) | Difference between arms mean changes (95% CI)b | |||
| Total fat | 12 mo | −0.16 (−0.26 to −0.06) (0.0013) | −0.10 (−0.20 to −0.005) (0.0396) | −0.05 (−0.19 to 0.08) | 0.4423 |
| 18 mo | −0.19 (−0.28 to −0.09) (0.0002) | −0.07 (−0.18 to 0.03) (0.1668) | −0.11 (−0.25 to 0.03) | 0.1259 | |
| Fat substitute | 12 mo | −0.21 (−0.33 to −0.08) (0.0018) | −0.10 (−0.23 to 0.03) (0.1177) | −0.10 (−0.28 to 0.08) | 0.2706 |
| 18 mo | −0.28 (−0.44 to −0.13) (0.0003) | −0.10 (−0.26 to 0.06) (0.2186) | −0.18 (−0.40 to 0.04) | 0.1055 | |
| Avoid fat | 12 mo | −0.06 (−0.19 to 0.07) (0.3824) | −0.01 (−0.15 to 0.13) (0.8495) | −0.04 (−0.23 to 0.14) | 0.6360 |
| 18 mo | 0.03 (−0.10 to 0.17) (0.6305) | −0.07 (−0.20 to 0.07) (0.3310) | 0.10 (−0.09 to 0.29) | 0.3047 | |
| Modify meat | 12 mo | −0.17 (−0.31 to −0.04) (0.0138) | −0.07 (−0.21 to 0.06) (0.2999) | −0.10 (−0.29 to 0.09) | 0.3072 |
| 18 mo | −0.18 (−0.30 to −0.06) (0.0040) | −0.09 (−0.23 to 0.05) (0.2251) | −0.10 (−0.28 to 0.09) | 0.3197 | |
| Replace fat | 12 mo | −0.14 (−0.27 to −0.01) (0.0364) | −0.10 (−0.24 to 0.03) (0.1356) | −0.04 (−0.22 to 0.15) | 0.7147 |
| 18 mo | −0.21 (−0.34 to −0.08) (0.0022) | −0.03 (−0.17 to 0.11) (0.6353) | −0.18 (−0.36 to 0.01) | 0.0630 | |
| Replace meat | 12 mo | −0.17 (−0.29 to −0.05) (0.0049) | −0.23 (−0.36 to −0.10) (0.0005) | 0.06 (−0.11 to 0.23) | 0.5078 |
| 18 mo | −0.16 (−0.29 to −0.03) (0.0129) | −0.05 (−0.19 to 0.10) (0.5141) | −0.11 (−0.30 to 0.07) | 0.2337 | |
| Total fiber | 12 mo | −0.16 (−0.26 to −0.07) (0.0011) | −0.15 (−0.25 to −0.05) (0.0037) | −0.01 (−0.15 to 0.12) | 0.8453 |
| 18 mo | −0.21 (−0.32 to −0.09) (0.0004) | −0.07 (−0.18 to 0.04) (0.2169) | −0.14 (−0.29 to 0.02) | 0.0824 | |
| Grain | 12 mo | −0.23 (−0.37 to −0.10) (0.0008) | −0.21 (−0.35 to −0.07) (0.0026) | −0.02 (−0.21 to 0.17) | 0.8142 |
| 18 mo | −0.25 (−0.40 to −0.11) (0.0006) | −0.11 (−0.27 to 0.04) (0.1429) | −0.14 (−0.34 to 0.06) | 0.1805 | |
| Fruit and vegetables | 12 mo | −0.15 (−0.27 to −0.03) (0.0132) | −0.11 (−0.23 to 0.02) (0.0874) | −0.04 (−0.21 to 0.12) | 0.6032 |
| 18 mo | −0.19 (−0.34 to −0.05) (0.0076) | −0.04 (−0.18 to 0.10) (0.5570) | −0.15 (−0.35 to 0.05) | 0.1385 | |
| Subfiber | 12 mo | −0.16 (−0.29 to −0.03) (0.0168) | −0.10 (−0.24 to 0.04) (0.1555) | −0.06 (−0.23 to 0.12) | 0.5073 |
| 18 mo | −0.19 (−0.33 to −0.06) (0.0059) | −0.05 (−0.18 to 0.08) (0.4349) | −0.14 (−0.32 to 0.05) | 0.1394 | |
| Fruit intake | 12 mo | −0.53 (−1.66 to 0.60) (0.3590) | −0.42 (−1.60 to 0.76) (0.4831) | −0.11 (−1.70 to 1.49) | 0.8956 |
| 18 mo | −2.27 (−3.13 to −1.41) (< 0.0001) | −1.17 (−2.13 to −0.21) (0.0168) | −1.10 (−2.29 to 0.09) | 0.0706 | |
| Vegetable intake | 12 mo | −2.53 (−4.24 to −0.81) (0.0039) | −2.15 (−4.01 to −0.30) (0.0232) | −0.37 (−2.82 to 2.07) | 0.7633 |
| 18 mo | −3.05 (−4.51 to −1.58) (< 0.0001) | −2.21 (−3.73 to −0.69) (0.0045) | −0.84 (−2.76 to 1.08) | 0.3917 | |
| Sugar-sweetened beverage intake | 12 mo | 0.32 (−1.20 to 1.84) (0.6824) | 1.74 (0.25 to 3.23) (0.0225) | −1.42 (−3.55 to 0.71) | 0.1911 |
| 18 mo | −0.14 (−1.33 to 1.05) (0.8174) | 0.67 (−0.53 to 1.87) (0.2752) | −0.81 (−2.48 to 0.86) | 0.3405 | |
| Total physical activity (METS) | 12 mo | −2.93 (−4.68 to −1.17) (0.0011) | 0.58 (−1.30 to 2.47) (0.5416) | −3.51 (−6.03 to −0.99) | 0.0065 |
| 18 mo | −2.81 (−4.76 to −0.86) (0.0048) | −0.72 (−2.70 to 1.25) (0.4710) | −2.08 (−4.76 to 0.60) | 0.1276 | |
| Recreational physical activity (METS) | 12 mo | −2.31 (−3.54 to −1.09) (0.0002) | −0.49 (−1.74 to 0.76) (0.4458) | −1.83 (−3.52 to −0.13) | 0.0344 |
| 18 mo | −1.93 (−3.04 to −0.82) (0.0007) | −1.29 (−2.41 to −0.17) (0.0238) | −0.64 (−2.19 to 0.91) | 0.4188 | |
- Each P value is adjusted for respective 6-month outcome only, except for subfiber and recreational physical activity, in which each P value is adjusted for both baseline and 6-month respective outcomes.
- a Change calculated as applicable value at 12 months minus applicable value at 6 months or applicable value at 18 months minus applicable value at 6 months, as appropriate.
- b Difference between arm mean changes calculated as applicable value for Weight Loss Only minus applicable value for Weight Loss + Maintenance.
Between-group analyses for dietary behaviors showed a trend toward a significant difference between study arms in total fiber at 18 months, with Weight Loss Only participants slipping back into old habits to a greater extent at 18 months relative to Weight Loss + Maintenance participants. Also, there was a trend toward a significant difference at 18 months in fruit intake and replacing high-fat foods with low-fat foods, with Weight Loss Only participants showing a greater decrease in fruit intake and fat replacement behaviors at 18 months relative to Weight Loss + Maintenance participants. For physical activity, between-arm analyses showed that Weight Loss Only participants decreased total and recreational physical activity to a significantly greater degree from 6 to 12 months than the Weight Loss + Maintenance participants, but there were no significant between-arm differences in physical activity at 18 months.
Intervention adherence
There were no significant differences between study arms in sessions attended from baseline to 6 months. A total of 64.9% of participants in Weight Loss Only attended at least 50% of the 16 sessions from baseline to 6 months, whereas 57.5% of those in Weight Loss + Maintenance attended at least half of the sessions. Overall, participants who attended at least half of the sessions offered in the first 6 months lost more (3.18% [2.41% to 3.95%]) of their initial body weight than participants who attended fewer sessions. There were also no significant between-arm differences in self-monitoring booklets completed from baseline to 6 months. During maintenance, a total of 27% of participants in the Weight Loss + Maintenance arm attended at least 50% of the maintenance sessions.
Discussion
The WORD resulted in significant weight loss and beneficial changes in diet and physical activity from baseline to 6 months. Participants in both arms lost weight, decreased BMI, increased fruit and vegetable intake, decreased sugar-sweetened beverage consumption, and improved dietary choices to increase fiber intake. Both groups also significantly increased METS expended in total and recreational physical activity. Participants who attended more intervention sessions lost more weight. The magnitude of weight lost from baseline to 6 months is comparable to that of other adaptations of the DPP for black participants (27). In most of these studies, the intervention was delivered by health professionals. The WORD successfully engaged CHWs to deliver the DPP, which is arguably more economical and accessible than intervention delivery by health professionals and merits future research examining the potential cost-effectiveness of using a community health worker model to disseminate the DPP.
After weekly weight loss classes ended at 6 months, dietary and physical activity behaviors began to change in a negative direction, and this was reflected in weight regain for participants in both arms. Moreover, even for participants in the arm that continued to have monthly maintenance sessions (Weight Loss + Maintenance), adherence was low as measured by session attendance and completion of self-monitoring booklets. Despite the low adherence, maintenance sessions appeared to slow the reversals for physical activity to some extent, but by 18 months, no significant between-group differences remained.
The percent weight regained in the Weight Loss + Maintenance arm is consistent with the limited literature on behavioral weight loss maintenance in black adults that reports average weight regains ranging from 0% to 64% at 12-month follow-up and 14% to 138% at 18-month follow-up (9). In general, studies reporting lower weight regain included more resource- and time-intensive maintenance sessions (9) and were delivered by staff or health professionals instead of CHWs (9). In Kumanyika et al.’s studies (28-30), the maintenance phase included biweekly and then monthly group classes and one-on-one sessions, sometimes at the clinic where behavioral consultation was available. The maintenance phases for the original DPP (West et al. (31)) and 2 other studies (Svetkey et al. (32) and Fitzgibbon et al. (33)) also included one-on-one, in-person sessions delivered by health care personnel. These studies were also located in academic medical centers or clinics, which may have drawn a more motivated participant pool. Future studies examining intervention strategies for black adults in community settings may consider a higher maintenance dose than 12 monthly sessions delivered over the course of a year, along with strategies to improve participation in maintenance sessions that are offered.
Although weight regain in the present study was observed in both groups, with the percentage of weight regained consistent with those shown in previous studies, there were no significant between-group differences in weight regained or BMI change at 12 or 18 months. However, among those who experienced clinically significant weight loss, participants in the Weight Loss + Maintenance arm trended toward experiencing lower weight regain compared with those in the Weight Loss Only arm at 12 months. Participants who lost at least 5% of their body weight may have been more motivated to maintain the weight lost after losing such a significant amount. However, even among this subgroup, weight regain was not significantly different between arms at 18 months. Thus, maintenance sessions appeared to delay but not prevent reversals in weight loss behavior and weight regain. The lack of significant between-arm differences in weight loss maintenance may have been facilitated by the dose received (low attendance and booklet completion) by participants in the Weight Loss + Maintenance arm. Previous studies testing the addition of a maintenance component have similarly reported no significant differences in weight regain, regardless of whether participants received a formal maintenance component (29, 34, 35). In their trial of an obesity treatment intervention in diverse rural participants, Rickel et al. (34) report that the addition of a maintenance component did not affect weight loss maintenance among their black participants.
Our study engaged the community infrastructure of churches, which are well known to provide social networks and support (36, 37). Our primary hypothesis was that formal maintenance sessions might not be needed for programs conducted within stable community institutions such as churches because those institutions may provide support for weight loss after formal sessions end. In fact, 3 out of the 15 churches in the Weight Loss Only intervention reported that they continued aspects of The WORD on their own. Participants of 1 church continued to meet regularly and complete self-monitoring booklets and the other 2 churches maintained physical activity sessions. This may have affected the lack of significant differences between arms.
Given that participants in both arms began to regain weight after weekly sessions ended and that monthly maintenance sessions did not significantly mitigate weight regain in the long run, perhaps a paradigm shift is needed to foster long-term adoption of DPP-based weight loss programs in stable community institutions. Instead of tapering off to less frequent and then no group sessions after weekly sessions end, the focus could be on working with churches to maintain weekly sessions indefinitely in the same way that church meetings are held on an ongoing weekly basis. Activities to foster healthy eating, exercise, and weight loss might become part of a church’s enduring mission. Future research is needed to identify strategies fostering long-term weight maintenance in community institutions such as churches.
Limitations of the study include the focus on rural black adults of faith, which may limit generalizability. However, given the inequitable burden of obesity that rural black adults experience, the authors believe that targeting this group was critical. Churches are also a salient institution for rural black adults and a potentially sustainable network through which weight loss interventions can be disseminated and sustained.
Conclusion
The WORD is one of the few behavioral weight loss maintenance interventions designed for black adults in a community setting and delivered entirely by CHWs. To the authors’ knowledge, only one other study has engaged a community setting in testing a behavioral weight loss intervention for black adults with the primary aim of weight loss maintenance (34, 38). To successfully combat the problem of obesity, implementing and disseminating evidence-based weight loss maintenance interventions, particularly in rural, low-resource settings, are critical. Data from this study can be used to inform future studies designed to reduce overweight and obesity in underserved, hard-to-reach populations to bring health equity.
Acknowledgments
The authors acknowledge the Faith Task Force, Ellen Hutchins, Tamier Wells, Kimberly Harris, Zoran Bursac, Mick Tilford, Delia West, ShaRhonda Love, and Kenya Eddings for invaluable guidance and expertise. All of the individual participant data collected during the trial, after deidentification, will be shared. The study protocol and consent form will also be made available. The data will be available beginning 12 months following publication; there will be no end date. Data will be shared with investigators whose proposed use of the data has been approved by KHKY; the analyses may be for any purpose. Approved proposals will receive the data from KHKY.





