Body Mass Index and Kidney Disease-Related Mortality in Midlife: A Nationwide Cohort of 2.3 Million Adolescents
Funding agencies: This study was supported by a research grant from the Environment and Health Fund, Jerusalem, Israel (award number RGA 1002) to JDK.
Disclosure: The authors declared no conflict of interest.
Abstract
Objective
This study aimed to evaluate the association of body mass index (BMI) in adolescence with mortality attributed to kidney disease.
Methods
In this study, 2,294,139 Jewish Israeli adolescents with measured weight and height at 17 years old during the military fitness assessment were analyzed with a follow-up extending up to 45 years. All kidney-related outcomes, coded by the Central Bureau of Statistics from death notifications as the underlying cause of death, were obtained by linkage. Cox hazards models were applied.
Results
During 42,297,007 person-years of follow-up (median 18.4 years), 226 deaths related to kidney disease were recorded. There was an increased risk for kidney-related death among adolescents with overweight and obesity with adjusted hazard ratios of 2.7 (95% CI: 1.8-3.9) and 8.4 (5.1-13.8), respectively, with BMI between 18.5 and 22.0 kg/m2 as the reference. A 15% increased risk for kidney-related mortality (1.11-1.19) per unit increment in BMI was observed. Furthermore, a multivariable spline model indicated a minimum risk for kidney-related mortality starting at BMI of 18.6 kg/m2 with significantly increased risk seen above values of 22.8 kg/m2. The results withstood extensive sensitivity analyses, including stratification of kidney-related death attributed to acute, chronic, and total kidney disease.
Conclusions
Adolescent overweight and obesity are risk markers for kidney-related mortality over 4 decades.
Introduction
Obesity is increasingly evident in childhood and adolescence and is recognized as a global epidemic in the Western world. Its prevalence has tripled in many countries worldwide with a reported prevalence of more than 30% in the United States and other developed countries (1). Recent evidence from 2015 has suggested that chronic kidney disease (CKD) is the second leading cause of body mass index (BMI)-related disability-adjusted life-years (2). In addition, according to Global Burden of Diseases data, mortality attributed to CKD among young adults (<50 years) has increased continuously in parallel to adolescent obesity (3). In the United States, for instance, an annual increase of 1.6% was recorded between 1995 and 2015 for young adults. On the contrary, several reports have suggested that obesity does not confer a risk for future CKD (4) and may even play a protective role in certain settings (a phenomenon also referred to as the “obesity paradox”) (5).
In either case, most investigations on the association between obesity and CKD have been limited to adulthood obesity (6-8). There are limited data regarding the association between adolescent or childhood BMI and future mortality risk related to kidney disease, as opposed to the well-established association with coronary heart disease outcomes (9, 10). The few investigations that have included adolescents and documented an association between adolescent obesity and future CKD risk used the World Health Organization (11) or the U.S. Centers for Disease Control and Prevention (12) classifications. These classifications include a broad normal BMI range as a reference and, consequently, may attenuate the risk attributed to obesity (13) or mask the BMI cutoff that is associated with increased risk. Notably, these estimates may well be biased by the use of self-reported and recalled data (11).
We previously reported on the association between measured BMI at adolescence and the future risk of cardiovascular- (14) and diabetes-related (13) death in midlife. For both death causes, BMI above 20 kg/m2 at age 17 was associated with increased mortality risk. In the current report, we elucidate the association between measured adolescent BMI and death attributed to kidney disease in a nationwide cohort of 2.3 million adolescents.
Methods
Study population
The study sample comprised all 2,454,693 Israeli teenagers who underwent medical assessments at ages 16 to 19 years between January 1, 1967, and December 31, 2010, prior to military conscription, regardless of future drafting into service. Participants with missing weight and height data (n = 64,186) and those belonging to non-Jewish minorities (n = 92,377) were excluded from analysis, as they are considered unrepresentative of their source population (14). We also excluded 3,991 participants who died before 1981, the year from which the underlying cause of death was available to us (Figure 1). Included in the final study sample were 2,294,139 participants, of whom 40.4% were women. Ethical approval for the study was provided by the Israel Defense Forces Medical Corps Institutional Review Board, which waived the need for informed consent based on the strict maintenance of participants' anonymity.
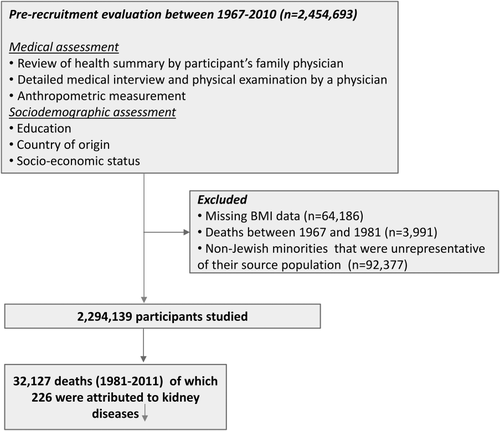
Schematic diagram of the study design. Note that nearly 80% (n = 3,188) of the 3,991 deaths that occurred before 1981 were attributed to military trauma.
Primary outcomes and documentation of the cause of death
The primary outcome of the study was kidney-related mortality coded as the underlying cause (International Classification of Diseases, Ninth Revision [ICD-9], 580-589; International Classification of Diseases, Tenth Revision [ICD-10], N00-N29). Renal cancer-related deaths were not included as an outcome. The underlying cause of death, as routinely officially coded from death notifications by the Israel Central Bureau of Statistics according to the ICD-9 and ICD-10, was linked by using the participants' national identification number. The cause of death was available to us only from 1981 and onward. The occurrence of death among recruits on active duty or in reserve service is documented in Israel Defense Forces records since 1967 with an indicator of deaths caused by service-related trauma (no other causes are provided). Follow-up ceased on the date of death from any cause or June 30, 2011, whichever came first.
Data collection and study variables
The health examination was performed by military physicians who also reviewed the previous medical history provided by the family physician. Standardized measurements of weight and height were undertaken by trained personnel with each participant barefoot and in underwear; BMI was calculated. Data regarding socioeconomic status, education, country of origin, and country of birth were recorded. Education was dichotomized into those with 12 versus ≤ 11 years of formal schooling (15). Socioeconomic status, based on the locality of residence at the time of examination (14), was grouped into low, medium, and high. Country of origin (classified as the birthplace of the father or grandfather, if the father was born in Israel) and country of birth were grouped as reported elsewhere (14, 15). Blood pressure measurements at rest in the sitting position were collected from 1967 but were computerized only from 1977 onward. These measurements were conducted with an appropriately sized cuff on the right arm using a manual sphygmomanometer as detailed elsewhere (16).
Statistical analysis
Adolescents in our study were expected to have completed more than 98.5% of their growth (17), thereby permitting the use of absolute BMI measures as a continuous or categorical variable. We grouped BMI categories according to a modified classification of the World Health Organization that included the division of the normal range to low-normal (18.50 ≤ BMI < 21.99) and high-normal (22.0 ≤ BMI < 24.99). The abnormal BMI subgroups included underweight (BMI < 18.50), overweight (25.0 ≤ BMI < 29.99), and obesity (BMI ≥ 30). Person-year mortality rates were calculated with follow-up commencing from 1981. Cox proportional hazard models were used to estimate the hazard ratios (HRs) and 95% CIs for kidney mortality with the low-normal group as the reference category. The following two main prespecified models were applied: unadjusted and a multivariable model adjusted for age, sex, year of birth, education, and country of origin. Variables in multivariable models were included only if they were associated with kidney mortality. In the absence of interaction between sex and BMI for kidney mortality (P > 0.6 for all models), we analyzed men and women grouped together.
Several sensitivity analyses were conducted. We restricted the Cox analysis to those with an unimpaired medical status at baseline (i.e., no indication of any medical diagnosis in the prerecruitment medical evaluation that would limit eligibility for combat service) as reported previously (14, 18) to avert confounding by a preexisting medical diagnosis, such as diabetes, hypertension, history of kidney injury, or rheumatic disease. The analysis was also stratified by deaths occurring prior to or later than age 50 (median age of death was 49.6 years), by deaths occurring before or later than 2006 (the median year of CKD deaths), and by deaths attributed to acute (ICD-9: 584, ICD-10: N17; n = 59 deaths), chronic (ICD-9: 585, ICD-10: N18; n = 117), and unspecified reason of kidney injury (ICD-9: 586, ICD-10: N179; n = 44). We conducted a sensitivity analysis limited to those examined from 1977 onward (the period for which computerized blood pressure data were available) and included mean blood pressure ([2 × PDiastolic + PSystolic]/3) as a continuous variable in the multivariable model. Multiple imputation was applied to those with missing data (1.4% of examinees) as described previously (14). Analyses were performed by using SPSS Statistics (version 23.0; IBM Corp., Armonk, New York).
Results
Table 1 summarizes the characteristics of the study participants. The mean age at enrollment was 17.3 ± 0.4 years, with more than 85% of participants being assessed between the ages of 17 and 18. Although 84% of the adolescents were born in Israel, substantial heterogeneity in their origins was observed, reflecting the diversity of the worldwide Jewish immigration to Israel. Most participants (80%) had a full high school education.
| BMI categories (kg/m2) | ||||||
|---|---|---|---|---|---|---|
| <18.5 | 18.5-21.99 | 22.0-24.99 | 25.0-29.99 | ≥30.0 | Total | |
| N participants | 315,066 | 1,126,717 | 549,602 | 239,423 | 63,331 | 2,294,139 |
| % Males | 59 | 60 | 59 | 58 | 60 | 60 |
| Age ± SD (y) | 17.3 ± 0.4 | 17.3 ± 0.4 | 17.3 ± 0.4 | 17.3 ± 0.4 | 17.4 ± 0.5 | 17.3 ± 0.4 |
| Height ± SD (boys) (cm) | 173.2 ± 7.0 | 173.4 ± 6.8 | 173.7 ± 6.8 | 174.0 ± 6.9 | 174.0 ± 7.5 | 173.5 ± 6.8 |
| Height ± SD (girls) (cm) | 162.8 ± 6.3 | 162.1 ± 6.0 | 161.8 ± 6.1 | 161.8 ± 6.2 | 162.3 ± 6.4 | 162.1 ± 6.1 |
| Mean BMI ± SD (kg/m2) | 17.5 ± 0.8 | 20.3 ± 1.0 | 23.3 ± 0.8 | 26.8 ± 1.4 | 32.9 ± 2.7 | 21.6 ± 3.4 |
| 12 years schooling (%) | 79 | 80 | 81 | 81 | 81 | 80 |
| Low residential SES | 24 | 25 | 23 | 25 | 27 | 24 |
| Born in Israel | 85 | 84 | 84 | 84 | 85 | 84 |
| Country of origin (%) | ||||||
| Israel | 6 | 6 | 6 | 6 | 6 | 6 |
| USSR | 13 | 12 | 13 | 14 | 14 | 13 |
| Asia | 24 | 24 | 25 | 24 | 25 | 24 |
| Africa | 23 | 24 | 24 | 24 | 25 | 24 |
| Europe | 30 | 32 | 31 | 31 | 29 | 31 |
| Ethiopia | 4 | 1 | 1 | 1 | 1 | 1 |
- Countries of origin classified by the father's or grandfather's country of birth (if the father was born in Israel) and grouped into the following six geographical areas: former Union of Soviet Socialist Republics (USSR), Asia (not including Asian USSR), Africa (predominantly North Africa, excluding South Africa and Ethiopia), Europe (and the following countries of emigration from Europe: North and South America, South Africa, Australia, and New Zealand, and excluding European USSR), Ethiopia, and Israel.
- SES, socioeconomic status.
The follow-up characteristics across the BMI categories are shown in Table 2. The median follow-up since 1981 (18.4 years) was lower in those with a higher BMI, a consequence of the later onset of the increasing prevalence of overweight and obesity in our cohort in the 1980s (15). During 42,297,007 person-years of follow-up, there were 226 deaths attributed to kidney injury out of a total of 32,127 deaths that were recorded in the cohort between 1981 and 2011; 83% of these (n = 187) occurred in men; 5.8%, 18.6%, 49.6%, and 97.6% occurred before age 30, 40, 50, and 60 years, respectively, with 50.4% of these deaths (n = 114) occurring from 2006 onward. The mortality rate increased steeply across age groups (Supporting Information Table S1). The mean age at death attributed to kidney disease was 48.1 ± 9.2, reflecting the relatively young ages of the cohort at end of the follow-up.
| BMI (kg/m2) | ||||||
|---|---|---|---|---|---|---|
| <18.5 | 18.50-21.99 | 22.0-24.99 | 25.0-29.99 | ≥30.0 | Totala | |
| Kidney disease-related mortality: all participants (226 deaths) | ||||||
| N participants | 19 | 96 | 55 | 37 | 19 | 226 |
| Deaths in men | 17 | 81 | 45 | 29 | 15 | 187 |
| Follow-up (y) (mean ± SD) | 18.2 ± 9.6 | 19.1 ± 9.8 | 18.5 ± 9.9 | 16.7 ± 9.8 | 13.6 ± 9.1 | 18.4 ± 9.8 |
| Median follow-up (y) (25th, 75th) | 18.1 (10.0, 28.1) | 19.4 (10.6, 30.1) | 18.6 (9.8, 29.5) | 16.0 (8.1, 25.7) | 11.7 (6.0, 19.8) | 18.4 (9.9, 29.10) |
| Cumulative follow-up (person-years) | 5,747,457 | 21,507,635 | 10,177,773 | 4,004,835 | 859,307 | 42,297,007 |
| Crude incidence (death/105 person-years) | 0.331 | 0.446 | 0.540 | 0.923 | 2.211 | 0.534 |
| HR (unadjusted)b | 0.80 | 1 (Ref) | 1.24 | 2.36 | 7.30 | 1.15 |
| 95% CI | 0.49-1.30 | 0.89-1.72 | 1.61-3.44 | 4.45-11.95 | 1.11-1.19 | |
| P | 0.366 | 0.210 | 9.52 × 10−6 | 2.95 × 10−15 | 4.92 × 10−17 | |
| HR (multivariable)b | 0.84 | 1 (Ref) | 1.32 | 2.64 | 8.40 | 1.16 |
| 95% CI | 0.51-1.37 | 0.95-1.84 | 1.80-3.87 | 5.11-13.81 | 1.13-1.20 | |
| P | 0.486 | 0.101 | 6.62 × 10−7 | 5.04 × 10−17 | 2.03 × 10−19 | |
| Kidney disease-related mortality among participants with unimpaired health (159 deaths) | ||||||
| N deaths | 12 | 71 | 43 | 25 | 8 | 159 |
| Deaths in men | 10 | 61 | 34 | 19 | 7 | 131 |
| HR (multivariable) | 0.87 | 1 (Ref) | 1.40 | 2.62 | 7.30 | 1.16 |
| 95% CI | 0.47-1.61 | 0.96-2.05 | 1.66-4.15 | 3.50-15.23 | 1.11-1.21 | |
| P | 0.657 | 0.080 | 3.93 × 10−5 | 1.17 × 10−7 | 5.51 × 10−10 | |
- Person-time incidence rate per 100,000 person-years of follow-up shown. Association assessed with Cox models adjusted for age, sex, birth year, education, and country of origin. For all outcomes, there was a significant trend across BMI categories (P ≤ 0.001).
- a Values reflect total sum of BMI categories or HR (±95% CI) for death attributed to kidney disease for every unit increment in BMI.
- b No interaction between sex and BMI for kidney disease-related mortality in unadjusted or multivariable model (P = 0.646 and 0.712, respectively).
- HR, hazard ratio.
Table 2 delineates follow-up time, crude person-year incidence rates, and adjusted Cox analysis across BMI groups. There was a graded increase in incidence, generally commencing from the low-normal BMI category (18.5 ≤ BMI < 22.0) onward. When analyzed as a continuous variable, BMI was associated with an unadjusted HR of 1.15 (1.11-1.19; P = 4.9 × 10−17) per unit increment in BMI for kidney disease mortality that persisted in the multivariable model: 1.16 (1.13-1.20; P = 2.0 × 10−19). When BMI was treated as categorical variable, the following high adjusted HRs for kidney disease mortality were evident for overweight and, particularly, adolescents with obesity: 2.6 (1.8-3.9) and 8.4 (5.1-13.8), respectively (with the low-normal BMI as the reference). BMI of 22.0 to 24.99 was associated with borderline significance (HR = 1.3; 95% CI: 1.0-1.8; P = 0.1). Figure 2 shows the Cox survival function of the study outcomes. Multivariable spline models indicated a minimum risk for renal mortality at BMI of 18.6, with a significantly increased risk seen above adolescent BMI values of 22.8 (Supporting Information Figure S1).
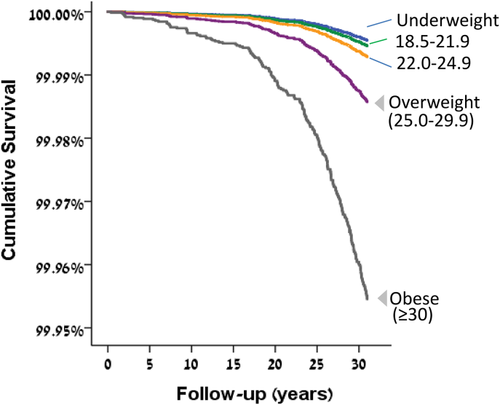
Relationship between BMI at adolescence and kidney disease survival. Multivariable Cox survival functions by BMI groupings are shown for mortality attributed to kidney disease. Models were adjusted for sex, age, birth year, education, and country of origin. [Color figure can be viewed at wileyonlinelibrary.com]
A series of sensitivity analyses was conducted. The restriction of the study sample to those with unimpaired health (Table 2) had little effect on the risk estimates among adolescents with overweight and obesity, thereby minimizing the possibility that concurrent medical conditions biased the association between BMI and kidney mortality. Risk estimates among adolescents with overweight and obesity persisted when the cohort was stratified by the age of death, but they were slightly stronger among those who died after the age of 50 years than those who died before (overweight, HR = 3.3 vs. 2.1; obesity, HR = 10.5 vs. 6.7) (Supporting Information Table S2). Similarly, results generally persisted when the cohort was stratified by the period of death, although risk estimates were slightly higher among adolescents with BMI in the high-normal, overweight, and obesity range for deaths occurring from 2006 onward than for the earlier period (HRs of 1.5, 3.0, and 8.8 vs. 1.1, 2.2, and 7.9, respectively) (Supporting Information Table S2). Limiting the analysis to participants enrolled in the study from the time when blood pressure data were available (1977 onward) yielded an unchanged risk when mean blood pressure was added to the multivariable model (52 deaths; HR = 1.16 per unit increment in BMI; 95% CI: 1.13-1.20). The association between BMI and kidney disease mortality also persisted when the latter was stratified by acute, chronic, or unspecified kidney injury. The computed HRs were 1.13 (1.05-1.21; P = 0.001), 1.19 (1.14-1.24; P = 4.9 × 10−15), and 1.15 (1.06-1.24; P = 3.8 × 10−5) per unit increment in BMI, respectively, and 2.1 (1.0-4.5; P = 0.048), 3.1 (1.8-5.2; P = 2.1 × 10−6), and 2.3 (1.0-5.5; P = 0.052) among adolescents with overweight compared with the low-normal BMI group, respectively.
Discussion
In this large nationwide cohort, we report on the association between late adolescent BMI and adult kidney disease-related mortality. The main findings of this study suggest that overweight and obesity increase the future risk for kidney disease-related mortality in apparently healthy teenagers with HRs of 2.7 and 8.4, respectively. Specifically, we observed a 16% increased risk for every unit increment in BMI. These findings persisted in a series of sensitivity analyses including stratification of kidney mortality because of acute or chronic kidney disease. Although the HRs for overweight- and obesity-related kidney mortality were high, the actual incidence of kidney-related mortality in our relatively young cohort was low but will increase sharply as the cohort ages. Interestingly, these point estimates were higher than those reported in this cohort for total cardiovascular (overweight, 2.3 [2.0-2.6]; obesity, 3.5 [2.9-4.1]; reference, BMI percentiles 5th-25th) (14) and cardiovascular cause-specific mortality (between 9% and 15.7% increased risk for the specific outcomes for every unit increment in BMI) (18).
In line with our findings, data from the Global Burden of Diseases project showed that approximately one-fourth of kidney mortality can be attributed to adulthood overweight and obesity (19). Also, a report that linked adult BMI with cause-specific mortality in a collaborative analyses of 57 studies showed a HR of 1.6 (95% CI: 1.3-2.0) for death because of renal disease per 5 BMI units in the range of > 25 (20). This value is modestly lower than the HR equivalent in our study (1.9; 95% CI: 1.7-2.0). The higher risk estimate reported here may reflect the stronger association between obesity and mortality and CKD incidence (11) at younger ages.
An earlier investigation from this cohort (12), as well as others (21), established the association between adolescent overweight and obesity and the risk of end-stage renal disease, a less frequent outcome than mortality among CKD patients (22, 23), especially among young adults (24). For this cohort, the adjusted risk estimates among adolescents with overweight and obesity for incident end-stage renal disease were 3.0 and 6.9, respectively, similar to the values reported here. Thus, having obesity may not only lead to CKD, but also probably an increased risk of CKD-related death once established CKD exists. This contradicts the notion of a protective role of obesity suggested by previous studies that highlighted the “obesity paradox in CKD patients” (5).
Adolescent BMI is clearly a risk marker, but is it a causal risk factor? We were unable to control for adolescent risk factors, such as smoking, exercise, and physical fitness (25), or for adult BMI. We consider two pathways by which adolescent BMI might influence kidney outcomes. First, adolescent BMI has been causally associated with multiple cardiometabolic risk markers, as demonstrated by Mendelian randomization studies, even within the nonobese BMI range (26). This is consistent with our observation that the risk estimate for the association between BMI and kidney-related mortality persisted when the study sample was limited to those with unimpaired health. Young prepubertal children with obesity already present significantly lower glomerular filtration rate estimates, suggesting some degree of adiposity-induced renal impairment (27). Adolescents with severe obesity were shown to have increased urinary excretion of kidney injury biomarkers that may persist years after significant weight loss induced by bariatric surgery (28), with higher rates of renal complications following elective procedures (29). Furthermore, early exposure to obesity at age 20 was associated with a higher risk for future CKD (11) or cause-specific mortality (30) than that conferred by the onset of obesity later in life. This may relate to a longer duration of exposure to obesity from adolescence than observed in adulthood. Second, as BMI shows tracking across age (31), and strongly from age 18 (32), it is likely that adulthood BMI mediates the association of adolescent BMI with kidney disease, at least in part. This pathway might explain the borderline association of high-normal BMI with kidney-related mortality. As adult measures of BMI were unavailable to us, we were unable to address this question.
Our study has certain limitations. First, as noted, we could not assess an independent effect of adolescent BMI in the absence of adult measures of BMI. Second, data on cause-specific death were unavailable to us for the first 14 years of this cohort. Yet deaths attributed to kidney disease before age 30 accounted for only 5.8% of the total kidney-related deaths recorded during the 31-year follow-up period, indicating that the potential effect of these missing data should be minimal. Third, we were unable to account for cardiovascular lifestyle risk factors in adolescence, such as physical activity and smoking, that may confound the BMI association. However, adjustment for sociodemographic variables that were previously shown to be strongly related to smoking in a subpopulation of this cohort (33) did not attenuate the association. Fourth, the mean age of kidney-related deaths was 48.1 years as our follow-up encompassed young and midadulthood, thereby reflecting mortality in young adulthood. We show, nevertheless, that cause-specific mortality in our cohort is representative of the Israeli population (13, 14) and is also similar to that reported by other cohorts with similar ages at enrollment and duration of follow-up (34). Fifth, waist circumference, which reflects abdominal adiposity and has been shown to be associated with mortality (35) and CKD incidence (36) independently of BMI, was not measured in our cohort. Nevertheless, BMI is a well-studied measure that is currently recommended by the US Preventive Services Task Force as the screening measure of choice for childhood and adolescent obesity (37). Finally, the outcome of the study, kidney disease-related mortality, may be underestimated by deaths attributed to cardiovascular or diabetic causes (38). Nevertheless, similar to the United States and other high-income countries, kidney-related mortality is ranked among the 10 leading causes of death in the general population (39, 40). The strengths of the study include the standardized measurement rather than recalled height and weight (41), the large sample size that provides stable estimates, and the extended follow-up.
In conclusion, in this large nationwide cohort, we confirmed the association between adolescent overweight and obesity and the deleterious consequences related to kidney disease. Our data suggest that BMI among adolescents with unimpaired health is a strong predictor of kidney mortality because of both acute and chronic kidney injury in early and midadulthood, with increased risk already seen within the currently accepted normal BMI range. The secular increase in overweight and obesity prevalence may account for a substantial and increasing burden of kidney-related mortality.





