Incremental Treatment Costs Attributable to Overweight and Obesity in Patients with Diabetes: Quantile Regression Approach
Funding agencies: This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number HI13C1480).
Disclosure: The authors declared no conflict of interest.
Abstract
Objective
This study aimed to estimate treatment costs attributable to overweight and obesity in patients with diabetes who were less than 65 years of age in the United States.
Methods
This study used data from the Medical Expenditure Panel Survey from 2001 to 2013. Patients with diabetes were identified by using the International Classification of Diseases, Ninth Revision, Clinical Modification code (250), clinical classification codes (049 and 050), or self-reported physician diagnoses. Total treatment costs attributable to overweight and obesity were calculated as the differences in the adjusted costs compared with individuals with diabetes and normal weight. Adjusted costs were estimated by using generalized linear models or unconditional quantile regression models.
Results
The mean annual treatment costs attributable to obesity were $1,852 higher than those attributable to normal weight, while costs attributable to overweight were $133 higher. The unconditional quantile regression results indicated that the impact of obesity on total treatment costs gradually became more significant as treatment costs approached the upper quantile.
Conclusions
Among patients with diabetes who were less than 65 years of age, patients with diabetes and obesity have significantly higher treatment costs than patients with diabetes and normal weight. The economic burden of diabetes to society will continue to increase unless more proactive preventive measures are taken to effectively treat patients with overweight or obesity.
Introduction
Diabetes affects approximately 29.1 million people in the United States, with 1.7 million new cases diagnosed each year (1). The number of persons in the United States with diabetes is projected to reach 39 million by the year 2050 (2). Simultaneously, the prevalence of overweight and obesity in the United States has increased steadily over the past several decades, and if these trends continue, 86.3% of adults will have overweight or obesity by 2030 (3). Individuals with obesity have an increased risk of developing diabetes (4, 5), and rising obesity rates are a significant contributing factor to the current diabetes epidemic.
There is a significant economic burden associated with diabetes, with total costs estimated at $245 billion in the United States in 2012 (6). With the increasing prevalence of diabetes, the annual associated economic impact is expected to increase to $349 billion in the United States and anywhere from $802 billion to $1.452 trillion globally by the year 2040 (7). Because patients with diabetes have higher rates of health-related absenteeism and reduced work productivity, diabetes also has significant indirect costs, which are responsible for an estimated additional $69 billion in reduced national productivity (6). Patients who were diagnosed with diabetes and who had overweight or obesity incurred greater costs and more lost time at work than their counterparts with diabetes and normal weight (8).
Individuals with obesity face various financial and medical difficulties, which can be mitigated through weight loss. Individuals with obesity incur approximately 19% to 36% higher total medical costs than those with normal weight as a result of higher rates of emergency room visits, hospitalizations, physician visits, and prescription drug use (9-11). Previous studies have shown that, in particular, when examining the subpopulation of patients who also have type 2 diabetes along with obesity, weight loss has been associated with the use of fewer medications, lower health care costs, and improved glycemic control in both interventional and retrospective observational studies (12, 13). Even moderate weight loss resulted in lower diabetes medication costs among patients with type 2 diabetes (14). Weight loss among patients with type 2 diabetes has further benefits of reducing diabetes- and cardiovascular-related mortality (15).
Given the increasing prevalence of diabetes and its relationship to obesity, it is important to estimate the additional cost burden attributable to overweight and obesity among patients with diabetes. However, most of these previous studies have utilized traditional linear regressions or logistic regressions, with a focus on upper percentiles of body mass index (BMI); while such approaches have examined the effect of obesity-related covariates on the mean of the dependent variable, effects may vary depending on the distribution of weight. Alternate analytic approaches (such as quantile regression) that account for the different effects of covariates at distinct weight thresholds have not been previously utilized to explore the relationship between obesity-related covariates and health care costs (16-19). The objectives of this study were to calculate total treatment costs among patients with diabetes who have normal weight, overweight, and obesity, to estimate additional treatment costs attributable to increased weight, and to investigate the impact of weight on attributable costs over the distribution of those costs.
Methods
Study design and database
This cross-sectional study used the Medical Expenditure Panel Survey (MEPS) data from 2001 to 2013. The MEPS database is a nationally representative survey of the US civilian noninstitutionalized population designed to collect health care information, such as demographic characteristics, health conditions, health status, use of medical services, charges and source of payments, satisfaction with care, and health insurance coverage. Thirteen years of MEPS data were pooled to increase sample sizes for robust analyses across subgroups and to allow for statistical precision of estimates, resulting in a total sample size of 13,939 patients with diabetes. Pooled survey weights were used for the analysis by using the method provided by the Agency for Healthcare Research and Quality to ensure that the study sample and results were generalizable to the US population (20).
Subjects
Patients with diabetes who were less than 65 years of age were identified through the following three methods: self-reported diagnosis based on whether they answered yes to the question, “Have you ever been told by a doctor or another health professional that you have diabetes?”, an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code of 250, or a clinical classification (CC) code of 049 (diabetes without complications) or 050 (diabetes with complications). All patients over the age of 65 were excluded regardless of the severity of complications because of diabetes. The study population was limited to persons younger than 65 years of age because the treatment costs of elderly patients with diabetes (older than 65 years) may be more likely to be influenced by comorbidities that were related to aging rather than by weight status. The CC code was generated by using Clinical Classification Software (formerly known as Clinical Classifications for Health Care Policy Research; Agency for Healthcare Research and Quality, Rockville, Maryland), which aggregates conditions and V codes into mutually exclusive categories, most of which are clinically homogeneous (20).
Patients with diabetes who had the following conditions were excluded from the study: women with a diagnosis code for pregnancy (i.e., ICD-9-CM code of 633-650 or CC code of 177-196), malignancy (i.e., ICD-9-CM code of 140-239, CC code of 011-045, use of cancer medications, or an affirmative answer to the question about cancer diagnosis), kidney dialysis (i.e., ICD-9-CM code of V56 or CC code of 158), human immunodeficiency virus (i.e., ICD-9-CM code of 042, 043, 996, V08, V42, V43, or V49, CC code of 005, or use of immunosuppressant), or BMI < 18.5 kg/m2. Because the above conditions resulted in large treatment costs that were less directly related to overweight or obesity, we excluded patients with these conditions.
Height and weight were collected based on participant self-report, and BMI was calculated in kilograms per meters squared. Patients with diabetes were selected based on the inclusion and exclusion criteria and were further categorized into three groups based on BMI levels as per the World Health Organization criteria: normal (18.5 kg/m2 ≤ BMI < 25 kg/m2), overweight (25 kg/m2 ≤ BMI < 30 kg/m2), or obesity (BMI ≥ 30 kg/m2) to measure the impact of obesity on total treatment costs (21).
Study variables
The primary study outcome variable was annual total treatment costs, which were composed of medical costs plus prescription drug costs. Medical costs were those associated with outpatient and/or office-based visits, emergency room visits, and hospitalizations (excluding all costs related to dental work or injuries). The total treatment costs were defined as the sum of direct payments for care provided during 1 year, including out-of-pocket costs and costs to the private insurer, Medicaid, Medicare, and other sources (20). Additional self-reported patient information used in the study analysis included the following: age (i.e., 18-50 and 51-64 years), race/ethnicity (i.e., non-Hispanic white, non-Hispanic non-white, Hispanic, other), education level (i.e., less than high school, high school graduate, more than high school, other), marital status (i.e., married, widowed, divorced, separated, and never married), insurance status (i.e., public only, private only, both, and uninsured), number of emergency room visits and hospitalizations, and comorbidities.
Relevant comorbidities were identified by using patient self-reported ICD-9-CM codes and included heart disease (ICD-9-CM code of 410-417 or 420-429 or CC code of 100,101,103,104, or 108), hypertension (ICD-9-CM code of 401-405 or CC code of 98 or 99), hyperlipidemia (ICD-9-CM code of 272, 440, 445, or V77 or CC code of 53, 114, or 116 ), kidney disease (nephropathy) (ICD-9-CM code of 285, 580-588, 590, 593, 595, 596, 599, or 791 or CC code of 156-159, 161, or 162), neuropathy (ICD-9-CM code of 337, 340, 349, 354-358, or 713 or CC code of 80, 81, or 95), retinopathy (ICD-9-CM code of 362, 364-366, 368, 369, 377, or 379 or CC code of 87-91), skin disease (ICD-9-CM code of 707 or CC code of 199), stroke (ICD-9-CM code of 430-438 or CC code of 109-113), and vascular disease (ICD-9-CM code of 441-448 or 451-459 or CC code of 115-121).
Statistical analysis
The average annual treatment costs per patient were calculated as the sum of all per patient costs incurred during a 1-year period divided by the number of study patients. Treatment costs per patient were highly skewed because of the variable nature of both the treatment duration and the costs associated with diabetes-related complications for individual patients (22). Therefore, a 95% confidence interval (CI) was calculated for mean costs by using the bias-corrected and accelerated methods of parametric bootstrapping with a resampling of 1,000 times.
A generalized linear model (GLM) with the log link function and a gamma distribution was used to determine significant factors associated with treatment costs based on the results of several tests, including Pregibon link test, Pearson correlation test, modified Hosmer and Lemeshow test, and modified Park's test (23). Costs attributable to overweight (obesity) were defined as the average costs per patient that could have been avoided if patients with overweight or obesity had normal weight (24). Because treatment costs were skewed with heteroscedastic variance, the attributable costs were estimated by using two methods: the GLM for the average attributable costs and the unconditional quantile regression for the quantile of the cost distribution (18,25-27).
Costs attributable to overweight were calculated in the following way: the GLM was used to estimate treatment costs on all the covariates, including age, gender, BMI status, race, level of education, type of health insurance, marital status, insurance status, number of emergency room visits or hospitalizations, diabetic medication dosage form, and comorbidities (i.e., heart disease, hypertension, hyperlipidemia, nephropathy, neuropathy, retinopathy) for patients with normal weight and overweight.
By using these estimated parameters, the mean costs were predicted for patients who had overweight, with the dummy variable for overweight set to one. The mean costs were also predicted for patients with overweight, with the dummy variable for overweight set to zero. The difference between these two estimated costs in patients with overweight represents the incremental costs that could have been reduced if patients with overweight had normal weight (i.e., attributable to overweight) (23, 25, 26). The same procedure was performed for patients with obesity.
Unconditional quantile regression was used because estimated costs may vary across the distribution of treatment costs (18, 19, 27, 28). If the impact of overweight and obesity on treatment costs varied across the distribution of treatment costs, then estimation methods for the mean treatment costs, such as GLM, could not account for these differences. Unconditional quantile regression produces different estimates of the impact of overweight or obesity on treatment costs according to quantiles and is also insensitive to outliers. Thus, this method enables the evaluation of the relationship of independent variables across the full range of a continuous dependent variable as opposed to simply its mean. Calculating predicted costs for each BMI group by using the unconditional quantile regression was similar to the GLM.
For all analyses, MEPS sampling and variance adjustment weights were utilized by using the subpop option within the survey procedure to reflect the survey design structure when the national representative values were estimated. All costs were adjusted to 2015 US dollars by using the medical care component of the 2015 US consumer price indices, which were based on prescription drug, physicians' service, inpatient hospital services, and outpatient hospital services. Data were analyzed by using SAS 9.2 (SAS Institute, Cary, North Carolina) and Stata software 10.1 (Stata Corp., College Station, Texas).
Results
The study sample consisted of 13,939 patients with diabetes across all BMI categories. Overall, 12.1% of patients with diabetes had normal weight, 27.4% had overweight, and 60.5% had obesity (Table 1). The mean patient age was 51.2 years, and patients with normal weight were younger than their counterparts with obesity or overweight (P < 0.001). Comorbid heart disease, hypertension, hyperlipidemia, nephropathy, and neuropathy were more common among patients with overweight and obesity than among patients with normal weight. Patients with diabetes and obesity had a slightly higher number of outpatient visits than their counterparts with normal weight.
| Total | Normal (18.5 ≤ BMI < 25) | Overweight (25 ≤ BMI < 30) | Obesity (BMI ≥ 30) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample | Weight N | % | Sample | Weight n | % | Sample | Weight n | % | Sample | Weight n | % | P valueb | |
| All sample in MEPS | 303,805 | 215,399,734 | 100 | 105,602 | 78,741,252 | 36.6 | 108,091 | 76,346,282 | 35.4 | 90,112 | 60,312,200 | 28.0 | |
| Patients with diabetes | 13,939 | 8,578,835 | 1,740 | 1,035,233 | 12.1 | 3,922 | 2,352,466 | 27.4 | 8,277 | 5,191,136 | 60.5 | ||
| Age (mean) | (51.20) | (49.07) | (51.74) | (51.38) | < 0.001 | ||||||||
| 18-50 | 5,810 | 3,394,039 | 39.6 | 768 | 466,292 | 45.0 | 1,525 | 859,596 | 36.5 | 3,517 | 2,068,151 | 39.8 | < 0.001 |
| 51-64 | 8,129 | 5,184,796 | 60.4 | 972 | 568,941 | 55.0 | 2,397 | 1,492,871 | 63.5 | 4,760 | 3,122,984 | 60.2 | |
| Gender | |||||||||||||
| Male | 6,649 | 4,487,047 | 52.3 | 828 | 501,004 | 48.4 | 2,223 | 1,442,870 | 61.3 | 3,598 | 2,543,173 | 49.0 | < 0.001 |
| Female | 7,290 | 4,091,788 | 47.7 | 912 | 534,229 | 51.6 | 1,699 | 909,596 | 38.7 | 4,679 | 2,647,963 | 51.0 | |
| Use of antidiabetic medication | |||||||||||||
| None | 3,781 | 2,210,598 | 25.8 | 589 | 347,585 | 33.6 | 1,129 | 632,270 | 26.9 | 2,063 | 1,230,743 | 23.7 | < 0.001 |
| Oral only | 6,968 | 4,345,141 | 50.7 | 654 | 360,055 | 34.8 | 1,932 | 1,154,244 | 49.1 | 4,382 | 2,830,842 | 54.5 | |
| Insulin only | 1,487 | 942,848 | 11.0 | 338 | 235,734 | 22.8 | 452 | 306,016 | 13.0 | 697 | 401,097 | 7.7 | |
| Both | 1,703 | 1,080,248 | 12.6 | 159 | 91,858 | 8.9 | 409 | 259,936 | 11.1 | 1,135 | 728,454 | 14.0 | |
| N of ER visits (mean) | (0.48) | (0.46) | (0.40) | (0.52) | 0.011 | ||||||||
| 0 | 10,500 | 6,477,197 | 75.5 | 1,364 | 809,681 | 78.2 | 3,089 | 1,848,192 | 78.6 | 6,047 | 3,819,324 | 73.6 | < 0.001 |
| 1-2 | 2,715 | 1,657,311 | 19.3 | 292 | 177,157 | 17.1 | 670 | 408,635 | 17.4 | 1,753 | 1,071,519 | 20.6 | |
| ≥ 3 | 724 | 444,327 | 5.2 | 84 | 48,395 | 4.7 | 163 | 95,639 | 4.1 | 477 | 300,293 | 5.8 | |
| N of OB/OP visits (mean) | (8.95) | (7.16) | (7.79) | (9.82) | < 0.001 | ||||||||
| 0 | 1,754 | 848,898 | 9.9 | 316 | 162,026 | 15.7 | 601 | 280,939 | 11.9 | 837 | 405,933 | 7.8 | < 0.001 |
| 1-6 | 7,224 | 4,352,657 | 50.7 | 938 | 544,079 | 52.6 | 2,099 | 1,247,173 | 53.0 | 4,187 | 2,561,404 | 49.3 | |
| 7-12 | 2,538 | 1,688,165 | 19.7 | 263 | 187,421 | 18.1 | 648 | 422,768 | 17.8 | 1,627 | 1,077,977 | 20.8 | |
| ≥ 13 | 2,423 | 1,689,115 | 19.7 | 223 | 141,707 | 13.7 | 574 | 401,586 | 17.1 | 1,626 | 1,145,822 | 22.1 | |
| Comorbidityb | |||||||||||||
| Heart disease | 603 | 371,656 | 4.3 | 48 | 31,240 | 3.02 | 147 | 85,499 | 3.6 | 408 | 254,916 | 4.9 | < 0.001 |
| Hypertension | 1,922 | 1,065,266 | 12.4 | 164 | 84,363 | 8.15 | 516 | 282,083 | 12.0 | 1,242 | 698,820 | 13.5 | < 0.001 |
| Hyperlipidemia | 2,490 | 4,654,468 | 54.3 | 266 | 143,766 | 13.89 | 727 | 431,607 | 18.4 | 1,497 | 911,454 | 17.6 | < 0.001 |
| Nephropathy | 262 | 144,903 | 1.7 | 38 | 17,349 | 1.68 | 71 | 38,761 | 1.7 | 153 | 88,793 | 1.7 | 0.977 |
| Neuropathy | 121 | 87,789 | 1.0 | 8 | 5,524 | 0.53 | 31 | 21,228 | 0.9 | 82 | 61,037 | 1.2 | 0.169 |
| Retinopathy | 134 | 87,313 | 1.0 | 14 | 9,413 | 0.91 | 40 | 26,850 | 1.1 | 80 | 51,050 | 1.0 | 0.810 |
- a Patients with diabetes identified based on ICD-9-CM code (250), CC code (049, 050), or physician diagnosis.
- b Differences among patients with normal weight, overweight, and obesity were tested by using ANOVA or Wald χ2 tests.
- MEPS, Medical Expenditures Panel Survey; Weight N, weighted number in the whole population in the United States; ER, emergency room; OB/OP, office based/outpatient.
Mean total treatment costs were $7,529 for patients with normal weight, $7,703 for patients with overweight, and $9,462 for patients with obesity (P < 0.001) (Table 2). Patients with obesity had higher mean medical costs (obesity: $6,225, overweight: $5,162, normal weight: $5,130; P = 0.006). Mean prescription medication costs were significantly higher for patients with obesity ($3,236) than for patients with normal weight ($2,399) or overweight ($2,541) (P < 0.001). Compared with patients without obesity, patients with obesity aged 51 to 64 years had significantly higher total mean annual health care costs ($10,552 vs. $8,141 for patients with normal weight and $8,811 for patients with overweight; P < 0.001).
| Total | Normal (18.5 ≤ BMI < 25) | Overweight (25 ≤ BMI < 30) | Obesity (BMI ≥ 30) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | (Bootstrap 95% CI) | Mean | (Bootstrap 95% CI) | Mean | (Bootstrap 95% CI) | Mean | (Bootstrap 95% CI) | P valuea | |
| Total treatment costs | $8,746 | ($8,378 to $9,114) | $7,529 | ($6,470 to $8,588) | $7,703 | ($7,025 to $8,381) | $9,462 | ($8,990 to $9,933) | < 0.001 |
| Medical costs | $5,802 | ($5,466 to $6,137) | $5,130 | ($4,159 to $6,101) | $5,162 | ($4,558 to $5,767) | $6,225 | ($5,785 to $6,666) | 0.006 |
| Inpatient | $2,940 | ($2,667 to $3,213) | $2,755 | ($1,980 to $3,530) | $2,648 | ($2,141 to $3,155) | $3,109 | ($2,738 to $3,481) | 0.201 |
| ER visits | $385 | ($348 to $422) | $419 | ($261 to $578) | $368 | ($298 to $439) | $385 | ($346 to $425) | 0.819 |
| OB/OP visits | $2,477 | ($2,329 to $2,624) | $1,955 | ($1,642 to $2,268) | $2,146 | ($1,936 to $2,355) | $2,731 | ($2,521 to $2,941) | < 0.001 |
| Prescription drugs | $2,945 | ($2,838 to $3,051) | $2,399 | ($2,119 to $2,679) | $2,541 | ($2,307 to $2,775) | $3,236 | ($3,113 to $3,360) | < 0.001 |
| Age | |||||||||
| 18-50 | $7,158 | ($6,618 to $7,697) | $6,782 | ($5,072 to $8,493) | $5,780 | ($4,919 to $6,641) | $7,815 | ($7,095 to $8,535) | 0.065 |
| 51-64 | $9,786 | ($9,286 to $10,286) | $8,141 | ($6,819 to $9,462) | $8,811 | ($7,854 to $9,768) | $10,552 | ($9,898 to $11,207) | < 0.001 |
| Gender | |||||||||
| Male | $8,695 | ($8,138 to $9,253) | $7,592 | ($5,834 to $9,350) | $8,071 | ($7,117 to $9,024) | $9,267 | ($8,548 to $9,986) | 0.029 |
| Female | $8,802 | ($8,351 to $9,253) | $7,470 | ($6,218 to $8,722) | $7,121 | ($6,298 to $7,944) | $9,649 | ($9,029 to $10,268) | < 0.001 |
| Use of antidiabetic medications | |||||||||
| None | $6,532 | ($5,893 to $7,171) | $6,383 | ($4,498 to $8,269) | $4,957 | ($4,209 to $5,705) | $7,383 | ($6,503 to $8,264) | 0.051 |
| Oral only | $7,707 | ($7,234 to $8,180) | $6,164 | ($4,164 to $8,165) | $6,889 | ($5,981 to $7,797) | $8,236 | ($7,672 to $8,800) | 0.013 |
| Insulin only | $12,978 | ($11,627 to $14,330) | $10,511 | ($8,159 to $12,863) | $11,637 | ($9,129 to $14,145) | $15,452 | ($13,451 to $17,453) | 0.002 |
| Both | $13,766 | ($12,444 to $15,087) | $9,559 | ($7,420 to $11,699) | $13,371 | ($10,802 to $15,940) | $14,437 | ($12,785 to $16,088) | 0.036 |
| Comorbidity | |||||||||
| Heart disease | $21,084 | ($18,477 to $23,690) | $12,428 | ($7,271 to $17,585) | $23,462 | ($17,163 to $29,761) | $21,347 | ($18,277 to $24,417) | 0.201 |
| Hypertension | $6,461 | ($5,850 to $7,072) | $4,955 | ($3,834 to $6,075) | $6,597 | ($4,951 to $8,243) | $6,588 | ($5,952 to $7,223) | 0.225 |
| Hyperlipidemia | $7,462 | ($6,754 to $8,170) | $7,472 | ($4,681 to $10,263) | $7,346 | ($5,771 to $8,921) | $7,516 | ($6,773 to $8,258) | 0.905 |
| Nephropathy | $20,842 | ($16,639 to $25,045) | $18,933 | ($9,411 to $28,455) | $15,824 | ($8,856 to $22,793) | $23,405 | ($17,308 to $29,503) | 0.184 |
| Neuropathy | $15,588 | ($10,664 to $20,512) | $29,183 | ($−2,047 to $60,413) | $13,161 | ($2,377 to $23,944) | $15,202 | ($10,072 to $20,331) | 0.546 |
| Retinopathy | $9,948 | ($7,051 to $12,844) | $11,990 | ($−5,383 to $29,364) | $8,872 | ($5,675 to $12,069) | $10,137 | ($6,577 to $13,697) | 0.929 |
- Costs were converted to 2015 values and are per patient, per year.
- a P values represented significance of mean costs among three groups within each variable category.
- ER, emergency room; OB/OP, office based/outpatient.
Figure 1 shows the adjusted treatment costs attributable to overweight and obesity compared with the treatment costs for patients with normal weight. Among the total treatment costs attributable to obesity, the medical service-related costs were $1,133 (P < 0.001) and prescription related costs were $719 (P < 0.001), resulting in a total of $1,852. The adjusted prescription drug costs attributable to overweight were $130.
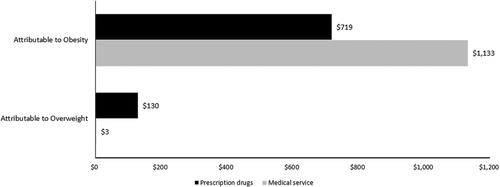
Adjusted treatment costs attributable to overweight and obesity in patients with diabetes.
Table 3 shows that patients with both diabetes and obesity had total treatment costs that were 29% higher (cost ratio = 1.29; 95% CI: 1.16-1.43) than those who had diabetes and had normal weight after adjusting for study variables. Patients with diabetes and overweight also had significantly higher total annual treatment costs than their counterparts with diabetes and normal weight (cost ratio = 1.17; 95% CI: 1.05-1.30).
| Unadjusted model | Adjusted model | |||||
|---|---|---|---|---|---|---|
| Cost ratio | (95% CI) | P value | Cost ratio | (95% CI) | P value | |
| BMI | ||||||
| Normal | 1 | 1 | ||||
| Overweight | 1.02 | (0.88-1.19) | 0.77 | 1.17 | (1.05-1.30) | 0.003 |
| Obesity | 1.26 | (1.09-1.45) | 0.002 | 1.29 | (1.16-1.43) | < 0.001 |
| Age | ||||||
| 18-50 | 1 | 1 | ||||
| 51-64 | 1.37 | (1.23-1.52) | < 0.001 | 1.79 | (1.7-1.87) | < 0.001 |
| Gender | ||||||
| Male | 1 | 1 | ||||
| Female | 1.01 | (0.92-1.12) | 0.807 | 1.01 | (0.91-1.12) | 0.829 |
| Insurance status | ||||||
| Public only | 1 | 1 | ||||
| Private only | 0.65 | (0.59-0.71) | < 0.001 | 0.69 | (0.53-0.90) | 0.007 |
| Both | 1.48 | (1.21-1.80) | < 0.001 | 1.21 | (0.94-1.55) | 0.136 |
| Uninsured | 0.4 | (0.31-0.44) | < 0.001 | 0.34 | (0.25-0.46) | < 0.001 |
| Use of antidiabetic medication | ||||||
| None | 1 | 1 | ||||
| Oral only | 1.18 | (1.05-1.33) | 0.006 | 1.81 | (1.68-1.96) | < 0.001 |
| Insulin only | 1.97 | (1.72-2.29) | < 0.001 | 3.03 | (2.57-3.59) | < 0.001 |
| Both | 2.11 | (1.83-2.43) | < 0.001 | 2.11 | (1.93-2.30) | < 0.001 |
| Comorbidity | ||||||
| Heart disease | 2.58 | (2.27-2.93) | < 0.001 | 1.84 | (1.55-2.18) | < 0.001 |
| Hypertension | 0.71 | (0.64-0.80) | < 0.001 | 1.19 | (1.10-1.28) | < 0.001 |
| Hyperlipidemia | 0.83 | (0.74-0.92) | 0.001 | 1.13 | (1.08-1.17) | < 0.001 |
| Nephropathy | 2.44 | (1.97-3.02) | < 0.001 | 1.26 | (1.15-1.38) | < 0.001 |
| Neuropathy | 1.80 | (1.31-2.47) | < 0.001 | 2.15 | (1.80-2.58) | < 0.001 |
| Retinopathy | 1.14 | (0.87-1.49) | 0.341 | 1.21 | (1.12-1.31) | < 0.001 |
- a Cost ratios estimated by using generalized linear model with log link function and gamma distribution after adjusting for study variables, including race, level of education, marital status, insurance status, number of emergency room visits and/or hospitalizations, and comorbidities. See “Statistical analysis” for detailed descriptions of variables included in model.
Table 4 shows that total treatment costs increased because of obesity by $83, $71, $516, $1,021, and $3,985 at the 10th, 25th, 50th, 75th, and 90th percentiles, respectively, compared with those of patients with normal weight after adjusting for other variables. The treatment costs attributable to obesity were not significant in most quantiles of the distribution except for the 50th and 90th percentiles. The effects of obesity on attributable costs were small at the bottom quantiles but more pronounced at higher quantiles. The treatment costs attributable to overweight were not significant in all quantiles of the distribution, as all 95% CIs for treatment costs attributable to overweight included a cost of zero.
| 10th percentile | 25th percentile | 50th percentile | 75th percentile | 90th percentile | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coeff | (95% CI) | Coeff | (95% CI) | Coeff | (95% CI) | Coeff | (95% CI) | Coeff | (95% CI) | |
| BMI | ||||||||||
| Normal | 0 | 0 | 0 | 0 | 0 | |||||
| Overweight | 87 | (−127 to 301) | 38 | (−239 to 315) | 229 | (−281 to 740) | 384 | (−851 to 1,619) | 1,999 | (−1,380 to 5,378) |
| Obesity | 83 | (−121 to 287) | 71 | (−195 to 337) | 516 | (31 to 1,002) | 1,021 | (−149 to 2,191) | 3,985 | (822 to 7,149) |
| Age | ||||||||||
| 18-50 | 0 | 0 | 0 | 0 | 0 | |||||
| 51-64 | 127 | (3 to 252) | 177 | (9 to 345) | 280 | (−37 to 597) | 451 | (−337 to 1,239) | −199 | (−2,648 to 2,251) |
| Gender | ||||||||||
| Male | 0 | 0 | 0 | 0 | 0 | |||||
| Female | 232 | (101 to 364) | 244 | (73 to 415) | 477 | (150 to 805) | 1,029 | (180 to 1,879) | 1,019 | (−1,610 to 3,648) |
| Insurance status | ||||||||||
| Public only | 0 | 0 | 0 | 0 | 0 | |||||
| Private only | −70 | (−270 to 130) | 44 | (−275 to 362) | 602 | (−16 to 1,219) | 1,201 | (−160 to 2,561) | 2,334 | (−1,958 to 6,626) |
| Both | 15 | (−302 to 332) | 270 | (−206 to 745) | 1,538 | (578 to 2,497) | 3,511 | (994 to 6,028) | 11,189 | (1,780 to 20,599) |
| Uninsured | −1,082 | (−1,363 to −801) | −1,013 | (−1,393 to −634) | −1,205 | (−1,857 to −553) | −1,695 | (−3,098 to −293) | −3,415 | (−7,758 to 928) |
| Use of antidiabetic medication | ||||||||||
| None | 0 | 0 | 0 | 0 | 0 | |||||
| Oral only | 1,416 | (1,232 to 1,600) | 1,392 | (1,185 to 1,600) | 1,496 | (1,154 to 1,839) | 1,871 | (1,096 to 2,645) | 651 | (−1,775 to 3,076) |
| Insulin only | 1,673 | (1,448 to 1,899) | 2,138 | (1,848 to 2,428) | 3,319 | (2,759 to 3,879) | 5,791 | (4,257 to 7,325) | 10,005 | (5,094 to 14,915) |
| Both | 1,730 | (1,549 to 1,911) | 2,192 | (1,956 to 2,428) | 3,961 | (3,482 to 4,439) | 7,882 | (6,406 to 9,359) | 11,961 | (6,904 to 17,018) |
- Coefficients estimated after adjusting for study variables, including race, level of education, marital status, insurance status, number of emergency room visits or hospitalizations, and comorbidities. See “Statistical analysis” for detailed descriptions of variables included in model.
The treatment costs attributable to overweight (top) and obesity (bottom) over the distribution of the costs are depicted in Figure 2. Variations in costs attributable to overweight and obesity became more pronounced as cost approached the upper percentiles.
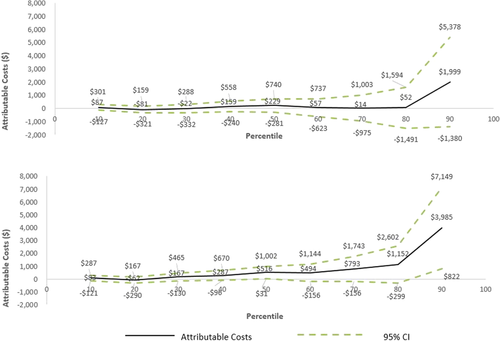
Distribution of adjusted treatment costs attributable to overweight (top) and obesity (bottom) by percentile of total treatment costs. [Color figure can be viewed at wileyonlinelibrary.com]
Discussion
Patients with diabetes and obesity were estimated to have $1,852 in additional yearly direct costs attributable to their obesity compared with patients with diabetes and normal weight. Among patients with overweight, however, the direct costs attributable to overweight were only slightly higher than those incurred by patients with normal weight. Adjusted treatment costs among patients with obesity were 29% higher than those of patients with normal weight, with medication use and number of outpatient visits having the greatest effect on treatment costs attributable to overweight and obesity. In this study, two statistical methods, GLM and the unconditional quantile regression method, were used to estimate the predicted costs. Each method showed a consistent effect of obesity on total health care costs compared with the costs in patients with diabetes and normal weight. Furthermore, among patients with obesity, the unconditional quantile regression method presented a consistent increase in treatment costs attributable to overweight and obesity with increasing total health care costs. This finding suggests that although the largest impact of weight reduction on total expenditures would be expected to occur among patients with diabetes who have the highest total health care costs, weight reduction may also reduce total costs even among patients with obesity and the lowest total health care costs, presumably those with moderate disease severity and lowest overall comorbidity.
The prediction from the GLM was a point estimate of the conditional mean of the treatment costs given the independent variables. The GLM describes the way that the mean of the treatment cost changes with BMI after adjusting for other covariates (16, 29). However, the conditional mean represented only the center of the distribution of the treatment costs. If BMI affects only the location of the distribution of the treatment costs but not the scale or shape of the distribution of the treatment costs, then the GLM may reliably estimate the attributable costs (27). However, the impact of BMI on treatment costs was not constant across the distribution of the treatment costs, as indicated by Figures 1 and 2. The attributable costs were different among the quantiles, and the CIs were not constant. To address these nonconstant impacts of BMI on the distribution of treatment costs, the unconditional quantile regression was used when estimates of the various quantiles of the treatment costs were desired (27, 28). This method accounts for the important relationship between BMI and treatment costs that differs along the entire treatment costs distribution. For example, the costs attributable to obesity for the quantiles from the 10th to 50th were lower than the average costs attributable to obesity, and those for the quantlies from the 75th to 90th were higher than the average costs attributable to obesity. This finding suggests that the impact of obesity on treatment costs could be higher for severe patients because these patients may have higher treatment costs.
Our results are consistent with previous studies that have demonstrated that obesity significantly contributes to increased total medical costs (8, 9, 11). One prior study found that patients with diabetes and obesity had total medical expenditures that were $1,980 ($2,520 in 2015 dollars) higher than those of patients with normal weight (8). Another study also found the increasing effect of obesity on the costs of diabetes care, albeit to a lesser degree, by about $600 to $700 ($860-$1,000 in 2015 dollars) relative to individuals with normal weight (9). The effect that obesity has on diabetes treatment and costs is likely to be multifactorial. Obesity may also place a patient with diabetes at greater risk for hospitalization from diabetes-related complications (30). In this study, obesity was associated with an 11% increase in costs. Similarly, another study reported that obesity increased the costs of diabetes treatment by 19% (9). The results suggest that improving weight control among patients with diabetes is likely to yield financial benefits as well as lower overall patient morbidity.
These prior studies have overlooked the fact that the effects of covariates are not the same across the distributions of overweight and obesity. They used traditional regression models, which could not investigate the varied effects of overweight and obesity on treatment costs based on their respective distributions. However, our results using the unconditional quantile regression demonstrated that the effects of overweight and obesity varied depending on the distribution of treatment costs in patients with diabetes.
This finding has been demonstrated in previous studies examining different weight-reduction interventions. A study found that patients with diabetes and obesity who had bariatric surgery experienced significant weight loss, which eventually resulted in a 70% decrease in total health care costs when calculated three years postsurgery (31). Recently, the International Diabetes Federation Taskforce on Epidemiology and Prevention of Diabetes issued a statement in support of bariatric surgery as an appropriate treatment option for patients with type 2 diabetes with BMIs of 35 kg/m2 or higher as well as for patients with BMIs of 30 to 35 kg/m2 who had major cardiovascular disease risk factors (32). Another study found that a primary care weight management program resulted in a cost savings sufficient to offset the total costs of the program after 2 years (33).
In Australia, a modest weight loss (1.4% of baseline body weight) was associated with a significant reduction in the costs of diabetes medications among 590 patients with type 2 diabetes (14). Yu used a simulated model to demonstrate that a 1% decrease in body weight among patients with obesity resulted in a 3.6% decrease (i.e., US $369 in 2015) in total annual treatment costs and a 5.8% decrease (i.e., US $189 in 2015) in diabetes-related treatment costs (34). In addition, a recent study found that a treatment cost reduction can be achieved in patients with higher BMIs (35). The results showed that with a 10% reduction in weight, the decrease in annual medical care costs for patients with a BMI of 45 kg/m2 (US $7,093) was seven times that of those with a BMI of 30 kg/m2 (US $1,076).
Our findings should be interpreted in the context of several limitations that warrant discussion. The MEPS data relies on patient self-reporting for disease diagnosis, which may underestimate the true prevalence of medical conditions because undiagnosed conditions would not be accurately captured. This issue may also result in the under inclusion of individuals with diabetes who have less severe disease (36, 37). Furthermore, BMI values may have been underestimated because people with overweight and obesity may over-report their height and under-report their weight. The prevalence of obesity based on self-reported weight and height in MEPS data is lower than the estimate based on measured weight and height in the National Health and Nutrition Examination Survey data (35). As a result, medical costs may have been underestimated, as the comparison group composed of individuals with normal weight may have actually included patients with overweight. Although patients aged 65 years and older who had some severe diabetic complications were excluded, patients who may have experienced prior weight loss because of uncontrolled diabetes may have been classified as patients with normal weight in our study. Such patients may have higher medical costs than other patients with diabetes and obesity. Their treatment costs were more associated with comorbidities that were related to aging rather than comorbidities associated with obesity status. Because of the pooled cross-sectional nature of MEPS data, direct causal inferences between obesity and treatment costs in patients with diabetes should be made with caution. However, this study examined the association between obesity and treatment costs in patients with diabetes and was strengthened by its estimation of the precise effects of overweight and obesity on treatment costs by using the unconditional quantile regression in a nationally representative, cross-sectional data set. The GLM with log link function and gamma distribution was also used to estimate effects of overweight and obesity on total treatment costs both with and without adjustment for the study variables in the model, but there is a possibility of over-controlling for medical conditions in the adjusted model (38, 39).
Conclusion
This study provides important evidence from a nationally representative sample of patients that individuals with diabetes and overweight or obesity have significantly higher treatment costs that are directly attributable to overweight or obesity than patients with diabetes and normal weight. The impact of obesity on treatment costs gradually increases as cost approaches the upper quantile of treatment costs. The economic burden of diabetes to society will continue to rise unless more proactive preventive measures are taken to effectively treat patients with diabetes and overweight and obesity.





