A Prospective Study of Obesity, Metabolic Health, and Cancer Mortality
Funding agencies: This study was supported by award R01-NR012726 from the National Institute for Nursing Research, UL1-RR025777 from the National Center for Research Resources, K08HL096841 from the National Heart, Lung, and Blood Institute, and by grants from the Center for Clinical and Translational Science and the Lister Hill Center for Health Policy of the University of Alabama at Birmingham. The REGARDS study was supported by cooperative agreement U01-NS041588 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health (NIH), Department of Health and Human Service. TA was supported by grants U54 CA118948 and K01 TW010271-01A1 from NIH. JM received grant support from grants R25 CA47888 and T32CA190194 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Disclosure: MS reports salary support to study patterns of statin use in Medicare and other large databases from Amgen; salary support for a research grant on lipids and CHD outcomes from diaDexus; consulting to help with FDA application from diaDexus; salary support for research grants from NIH and AHRQ. The other authors declared no conflict of interest.
Author contributions: TA led the design, analysis, interpretation of data, and writing of the manuscript. TA and JM conducted the statistical analysis and drafting of the manuscript. TA, JM, MP, SJ, MG, JS, VH, MS, SG contributed to the interpretation of data and writing and reviewing of the manuscript. All authors have read and approved the final version of the manuscript.
Abstract
Objective
This study examined whether metabolic health status is associated with risk of cancer mortality and whether this varies by body mass index (BMI) category.
Methods
A prospective study of 22,514 participants from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort was performed. Metabolically unhealthy status was defined as having three or more of the following: (1) elevated fasting glucose, (2) high triglycerides, (3) dyslipidemia, (4) hypertension, and (5) elevated waist circumference. Participants were categorized into normal weight (BMI 18.5-24.9 kg/m2), overweight (BMI 25.0-29.9 kg/m2), and obesity (BMI ≥ 30 kg/m2) groups. Cox proportional hazards regression was performed to estimate hazards ratios (HRs) and 95% confidence intervals (CIs) for cancer mortality during follow-up.
Results
Among participants with normal weight, participants who were metabolically unhealthy had an increased risk of cancer mortality (HR: 1.65; 95% CI: 1.20-2.26) compared with metabolically healthy participants. The overall mortality risk for participants who were metabolically unhealthy and had normal weight was stronger for obesity-related cancers (HR: 2.40; 95% CI: 1.17-4.91). Compared with participants with normal weight, those who were metabolically healthy and overweight were at a reduced risk of any cancer mortality (adjusted HR: 0.79; 95% CI: 0.63-0.99).
Conclusions
There was an increased risk of overall and obesity-related cancer mortality among metabolically unhealthy participants with normal weight.
Introduction
Obesity has long been understood to increase the risk of cancer mortality (1-5), and it is also an established risk factor for multiple chronic diseases, including type 2 diabetes, cardiovascular disease, metabolic syndrome, and cancer. The prevalence of obesity in the United States has reached epidemic proportions, with up to two-thirds of US adults currently in the overweight or obesity categories (6). Concurrently, the prevalence of metabolic syndrome, a cluster of cardiometabolic risk factors that include high fasting blood glucose, low high-density lipoprotein (HDL) cholesterol, high blood pressure, and high triglycerides, has also increased rapidly (7). However, a 2008 study based on data from the US National Health and Nutrition Examination Survey showed that 32% of US adults with obesity were metabolically healthy; i.e., they had none or one of the cardiometabolic risk factors typically associated with obesity (8). Clinical research studies have suggested that this subgroup of metabolically healthy individuals with obesity displays favorable insulin, inflammatory, and lipid profiles and may be at a lower risk for obesity-related chronic conditions compared with metabolically unhealthy counterparts (9). This raises the intriguing question of whether there is a consistent association between metabolic health status and the risk of adverse health outcomes in US adults and whether the association varies by body mass index (BMI) category (10).
Recent studies have provided some evidence for differences in the biological response to obesity and the risk of cancer based on metabolic health status. For instance, a 2014 study observed a 200% increased risk of cancer among adults with overweight and elevated blood glucose, compared with a 50% increased risk among adults with overweight and normal glucose (11). Two other recent studies examined metabolic health status and obesity in relation to cancer mortality among Korean adults; both studies observed a significantly lower risk of cancer mortality among metabolically healthy adults with obesity compared with those who were metabolically unhealthy with obesity (12, 13). This is in line with prior studies that have shown that metabolically healthy individuals with obesity may be at a lower or similar risk of cardiovascular diseases compared with adults without obesity and, thus, may be protected against the cardiometabolic complications of obesity (9). The evidence on whether metabolically healthy obesity is similarly associated with cancer mortality among US adults remains sparse. If we find consistent scientific evidence that the influence of metabolic health status on cancer outcomes varies by BMI, this information will add to the growing literature regarding the importance of metabolic risk factors in cancer prognosis. In this study, we examine the association between metabolic health and obesity (as categorized by BMI) on cancer mortality in a national US population of black and white participants.
Methods
Data source
The Reasons for Geographic and Racial Differences in Stroke (REGARDS) is one of the largest ongoing national longitudinal cohorts of community-dwelling adults in the United States (14). Designed to identify contributors to racial and geographic differences in stroke mortality, the cohort included 30,239 participants aged ≥ 45 years at baseline; 45% were male, 41% were black, and 69% were > 60 years old. Participants were recruited between January 2003 and October 2007, and detailed information about demographics, health behaviors, chronic medical conditions, physical status, diet, and medications was collected (14). During the course of the prospective follow-up, participants are contacted by telephone every 6 months to identify any medical event or hospitalizations experienced since the prior contact. For statistical analysis, we excluded participants who were missing data on metabolic components (4,846), had a prior history of cancer diagnosis at baseline (2,175), were missing data on follow-up time (236), or had BMI <18.5 kg/m2 (349), leaving a total of 22,514 participants for analysis.
Cancer mortality outcome
The primary outcome in this study was death caused by any cancer. Cancer mortality was ascertained by using death certificates, medical records, interviewed proxies, and linkages with the Social Security Death Index as well as the National Death Index. Date of death was confirmed by using death certificates, the Social Security Death Index, and/or the National Death Index, and cause of death was adjudicated by a committee of experts by using all available information as recommended by national guidelines (15). As a secondary outcome, we examined obesity-related cancer deaths, defined as cancers of the breast, colorectal, kidney, pancreas, endometria, and esophagus (16). The follow-up time for each participant was calculated from the enrollment date through the date of cancer death, death, or last telephone follow-up through December 31, 2012.
Main exposure variables
The main exposure variables of interest were metabolic health and BMI category. First, we defined metabolic health by using the criteria for metabolic syndrome proposed by international consensus in 2009 (17). These criteria define metabolic syndrome based on the presence of three or more of the following components: (1) an elevated waist circumference > 102 cm for males or > 88 cm for females; (2) elevated triglycerides ≥ 150 mg/dL or reported use of medication for elevated triglycerides; (3) reduced HDL cholesterol, defined as < 40 mg/dL for males and < 50 mg/dL for females, or the use of lipid lowering medications; (4) elevated blood pressure, defined as systolic blood pressure ≥ 130 mm Hg, diastolic blood pressure ≥ 80 mm Hg, or the reported use of antihypertensive agents; and (5) elevated glucose, defined as fasting glucose ≥ 100 mg/L or the use of insulin or oral hypoglycemic agents. For this analysis, metabolically unhealthy participants were those with at least three of the five metabolic syndrome components, while metabolically healthy participants were those with fewer than three. We further defined BMI category based on interviewer-measured participant height and weight during the baseline in-home examination. We classified BMI category into the following three categories as recommended by the Centers for Disease Control and Prevention: (1) normal weight = BMI < 25.0 kg/m2, (2) overweight = BMI between 25.0 and 29.9 kg/m2, and (3) obesity = BMI ≥ 30 kg/m2 (18) As a sensitivity analysis, we further classified metabolically unhealthy as those with at least two of the five metabolic syndrome components and conducted a subgroup analysis focusing only on mortality due to obesity-associated cancers.
Participant characteristics
Baseline demographic variables used in the analysis included age, race, sex, household income, education, and geographic region. Health behaviors included tobacco, alcohol use, and physical activity. Baseline chronic medical conditions included atrial fibrillation, chronic kidney disease, deep vein thrombosis (DVT), myocardial infarction (MI), peripheral artery disease (PAD), and stroke. Excluding components of metabolic syndrome, an individual-level comorbidity score was created based on the sum of the total number of comorbidities at baseline for each participant (i.e., atrial fibrillation, chronic kidney disease, coronary artery disease, DVT, MI, PAD, and stroke). We presented the distribution of comorbidity scores as means and standard deviations.
Statistical analysis
We compared baseline characteristics by metabolic health and BMI category by using χ2 tests for categorical characteristics, analysis of variance (ANOVA) for normal continuous variables, and a Wilcoxon test for non-normal continuous variables. We estimated any cancer and obesity-related cancer mortality rates per 1,000 person-years by using Poisson regression for each weight status category. To estimate the hazards of cancer mortality, we fit three series (for each BMI category group) of Cox proportional hazard models, examining the association between metabolic health status and time to cancer death. We examined the effect of each metabolic syndrome component, as well as total number of metabolic syndrome components, on cancer mortality and stratified by BMI category by using Cox regression. In a secondary analysis, we performed additional Cox proportional hazard models to estimate the hazards of obesity-related cancer mortality by metabolic health status. To account for all-cause mortality as a competing risk, we employed the Fine and Gray method of Cox regression to calculate the subdistribution hazard of cancer mortality and obesity-related cancer mortality (19). We adjusted all models for age, race, sex, education, income, tobacco use, alcohol use, physical inactivity, low-density lipoprotein cholesterol, and comorbidity score. We assessed for multicollinearity among our study covariates by calculating the variance inflation factors (VIFs). To obtain the VIFs, we regressed each explanatory variable onto all other covariates. There was no evidence of multicollinearity between the covariates, and all VIFs were less than 1.50. In sensitivity analyses, we examined the effect of BMI category on cancer mortality by using Cox regression and additionally stratified by metabolic health status. We also examined the main effect of obesity on obesity-related cancer mortality by using Cox regression and additionally stratified by metabolic health status. Models examining the main effect of BMI on any cancer mortality or obesity-related cancer mortality were additionally adjusted for metabolic health status when not stratified by metabolic health status. We conducted sensitivity analyses excluding all cancer deaths within the first 2 years of entry into the REGARDS cohort as well as excluding all participants with comorbidities at baseline. The results of all models were expressed as adjusted hazard ratios (HRs) and the corresponding 95% confidence intervals (CIs). Participants were censored at the time of death, loss to follow-up, or the end of cancer mortality ascertainment (December 31, 2012). SAS version 9.4 (SAS Institute Inc, Cary, North Carolina) and Stata version 13 (StataCorp LLC, College Station, Texas) were used for all statistical analyses. Two-sided P < 0.05 was considered statistically significant.
Ethical statement
The institutional review board of all participating universities approved the study and all participants provided written informed consent.
Results
Among 30,239 REGARDS participants, 7,725 were excluded, resulting in 22,514 for analysis. Of the included participants, 5,377 (23.9%) were categorized as having normal weight, 8,351 (37.1%) had overweight, and 8,786 (39.0%) had obesity. In general, metabolically unhealthy participants were older, had lower education and income, and were more likely to be current tobacco users (Table 1; P < 0.01) compared with metabolically healthy participants in all weight categories. In addition, metabolically unhealthy participants with normal weight had a greater prevalence of atrial fibrillation, coronary artery disease, DVT, diabetes, dyslipidemia, hypertension, MI, PAD, and stroke (P < 0.01). Similar patterns were observed among participants with overweight and obesity, although the prevalence of diabetes was much higher among metabolically unhealthy participants with overweight and obesity.
| Normal weight, BMI 18.5-24.9 kg/m2 (n = 5,377) | Overweight, BMI 25.0-29.9 kg/m2 (n = 8,351) | Obesity, BMI ≥ 30 kg/m2 (n = 8,786) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MH (n = 4,720) | MU (n = 657) | P valued | MH (n = 5,503) | MU (n = 2,848) | P valued | MH (n = 2,872) | MU (n = 5,914) | P valued | |
| Agea | 65.5 (10.2) | 68.4 (9.2) | < 0.01 | 64.2 (9.3) | 66.4 (9.1) | < 0.01 | 62.1 (8.7) | 63.0 (8.5) | < 0.01 |
| Race (%) | |||||||||
| Black | 1,365 (28.9) | 204 (31.0) | 0.3 | 1,963 (35.7) | 1,045 (36.7) | 0.4 | 1,545 (53.8) | 2,907 (49.2) | < 0.01 |
| White | 3,355 (71.1) | 453 (69.0) | 3,540 (64.3) | 1,803 (63.3) | 1,327 (46.2) | 3,007 (50.8) | |||
| Sex (%) | |||||||||
| Male | 2,020 (42.8) | 285 (43.4) | 0.8 | 2,980 (54.2) | 1,353 (47.5) | < 0.01 | 1,029 (35.8) | 2,250 (38.1) | 0.04 |
| Female | 2,700 (57.2) | 372 (56.6) | 2,523 (45.9) | 1,495 (52.5) | 1,843 (64.2) | 3,664 (61.9) | |||
| Education ≤ high school (%) | 415 (8.8) | 107 (16.3) | < 0.01 | 483 (8.8) | 412 (14.5) | < 0.01 | 319 (11.1) | 888 (15.0) | < 0.01 |
| Income ≤ $20,000 (%) | 683 (14.5) | 162 (24.7) | < 0.01 | 628 (11.4) | 582 (20.4) | < 0.01 | 488 (17.0) | 1,278 (21.6) | < 0.01 |
| Current tobacco use (%) | 865 (18.4) | 186 (28.4) | < 0.01 | 646 (11.8) | 491 (17.3) | < 0.01 | 278 (9.7) | 780 (13.2) | < 0.01 |
| Heavy alcohol use (%) | 280 (6.0) | 32 (5.0) | < 0.01 | 258 (4.8) | 104 (3.7) | < 0.01 | 86 (3.1) | 158 (2.7) | < 0.01 |
| No physical activity (%) | 1,332 (28.7) | 287 (44.4) | < 0.01 | 1,427 (26.3) | 1,039 (37.1) | < 0.01 | 1,028 (36.2) | 2,406 (41.3) | < 0.01 |
| Chronic medical conditions (%) | |||||||||
| Atrial fibrillation | 375 (8.1) | 75 (11.7) | < 0.01 | 369 (6.8) | 273 (9.8) | < 0.01 | 204 (7.3) | 542 (9.4) | < 0.01 |
| Chronic lung disease | 403 (8.6) | 55 (8.4) | 0.9 | 433 (7.9) | 255 (9.0) | 0.09 | 289 (10.1) | 658 (11.1) | 0.1 |
| Coronary artery disease | 689 (14.9) | 157 (24.5) | < 0.01 | 788 (14.6) | 646 (23.0) | < 0.01 | 337 (12.0) | 1,179 (20.3) | < 0.01 |
| Deep vein thrombosis | 187 (4.0) | 40 (6.2) | 0.01 | 201 (3.7) | 151 (5.3) | < 0.01 | 157 (5.5) | 394 (6.7) | 0.03 |
| Myocardial infarction | 497 (10.7) | 111 (17.3) | < 0.01 | 546 (10.1) | 449 (16.0) | < 0.01 | 240 (8.5) | 842 (14.5) | < 0.01 |
| Peripheral artery disease | 105 (2.2) | 27 (4.1) | < 0.01 | 89 (1.6) | 81 (2.9) | < 0.01 | 27 (0.9) | 139 (2.4) | < 0.01 |
| Stroke | 246 (5.2) | 73 (11.2) | < 0.01 | 221 (4.0) | 236 (8.3) | < 0.01 | 101 (3.5) | 385 (6.5) | < 0.01 |
| Comorbidity scorea, b | 0.52 (0.92) | 0.80 (1.10) | < 0.01 | 0.48 (0.86) | 0.73 (1.05) | < 0.01 | 0.47 (0.85) | 0.69 (1.02) | < 0.01 |
| Follow-up yearsc | 6.9 (5.5-8.2) | 6.5 (4.6-8.2) | 0.01 | 7.1 (5.6-8.4) | 6.9 (5.4-8.4) | < 0.01 | 6.8 (5.6-8.2) | 6.8 (5.4-8.2) | 0.12 |
| BMIa | 23.3 (1.4) | 22.7 (1.6) | < 0.01 | 27.3 (1.4) | 27.8 (1.4) | < 0.01 | 34.3 (4.4) | 36.0 (5.2) | < 0.01 |
- a Means (standard deviations).
- b Comorbidity score presented as means and standard deviations of the sum total of comorbidities.
- c Median (interquartile range).
- d Significance determined by using ANOVA (normal continuous), Wilcoxon (nonparametric continuous), and χ2 tests. MH, metabolically healthy; MU, metabolically unhealthy, defined as presence of three or more metabolic components, including elevated fasting glucose, high triglycerides, dyslipidemia, hypertension, and high waist circumference.
There were 766 (3.4%) cancer deaths observed among 22,750 study participants over a mean follow-up time of 6.5 years. The most common cancer types were lung (28.9%), gastrointestinal (19.6%), and hematological (10.8%) cancers (Supporting Information Table S1). Among participants with normal weight, metabolically unhealthy participants were at a 65% increased risk of cancer mortality (adjusted HR: 1.65; 95% CI: 1.20-2.26) compared with metabolically healthy participants (Table 2), and metabolically unhealthy participants with normal weight had the lowest survival probability over the follow-up period (Figure 1). Even when considering all-cause mortality as a competing risk (Table 2), the increased risk of cancer mortality among participants with normal weight persisted when comparing metabolically unhealthy with metabolically healthy participants (adjusted HR: 1.67; 95% CI: 1.21-2.30). However, there was no statistically significant increased risk of cancer mortality for metabolically unhealthy participants with overweight (adjusted HR: 0.89; 95% CI: 0.67-1.17) or obesity (adjusted HR: 1.12; 95% CI: 0.84-1.49).
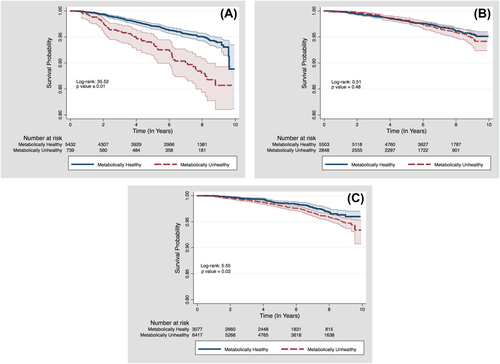
Kaplan-Meier survival plots for time to cancer death by metabolic health status, stratified by BMI category. (A) Among participants in the normal weight BMI category. (B) Among participants in the overweight BMI category. (C) Among participants in the obesity BMI category.
| Any cancer deathsb | Obesity-related cancer deathsc | |
|---|---|---|
| Normal weight (BMI 18.5-24.9 kg/m2) | ||
| MH (cancer deaths/at risk), n | 199/4,720 | 30/4,720 |
| MU (cancer deaths/at risk), n | 57/657 | 12/657 |
| MH mortality per 1,000 person-years (95% CI) | 6.45 (5.62-7.42) | 0.97 (0.68-1.39) |
| MU mortality per 1,000 person-years (95% CI) | 13.94 (10.75-18.10) | 2.93 (1.66-5.17) |
| Hazard ratio (95% CI): referent group MH | 1.65 (1.20-2.26) | 2.40 (1.17-4.91) |
| Subdistribution hazard ratio (95% CI)d: referent group MH | 1.67 (1.21-2.30) | 2.37 (1.13-4.98) |
| Overweight (BMI 25.0-29.9 kg/m2) | ||
| MH (cancer deaths/at risk), n | 167/5,503 | 41/5,503 |
| MU (cancer deaths/at risk), n | 88/2,848 | 13/2,848 |
| MH mortality per 1,000 person-years (95% CI) | 4.50 (3.87-5.24) | 1.11 (0.81-1.50) |
| MU mortality per 1,000 person-years (95% CI) | 4.74 (3.85-5.85) | 0.70 (0.41-1.21) |
| Hazard ratio (95% CI): referent group MH | 0.89 (0.67-1.17) | 0.58 (0.30-1.12) |
| Subdistribution hazard ratio (95% CI)d: referent group MH | 0.85 (0.64-1.13) | 0.57 (0.30-1.09) |
| Obesity (BMI ≥ 30 kg/m2) | ||
| MH (cancer deaths/at risk), n | 71/2,872 | 20/2,872 |
| MU (cancer deaths/at risk), n | 184/5,914 | 49/5,914 |
| MH mortality per 1,000 person-years (95% CI) | 3.76 (2.98-4.75) | 1.06 (0.68-1.64) |
| MU mortality per 1,000 person-years (95% CI) | 4.83 (4.18-5.58) | 1.29 (0.97-1.70) |
| Hazard ratio (95% CI): referent group MH | 1.12 (0.84-1.49) | 1.17 (0.68-2.02) |
| Subdistribution hazard ratio (95% CI)d: referent group MH | 1.09 (0.81-1.46) | 1.15 (0.67-1.97) |
- a Models adjusted for age, race, sex, education, income, tobacco use, alcohol use, physical inactivity, low-density lipoprotein cholesterol, and comorbidity score.
- b 766, total any cancer deaths.
- c 165, total obesity-related cancer deaths, including breast, colorectal, kidney, pancreatic, endometrial, and esophageal cancers.
- d Estimated using Fine and Gray method, accounting for 2,971 all-cause deaths as competing risk; models adjusted for age, race, sex, education, income, tobacco use, alcohol use, physical inactivity, low-density lipoprotein cholesterol, and comorbidity score. Bold indicates statistically significant association at 0.05 alpha level.
- MH, metabolically healthy; MU, metabolically unhealthy, defined as presence of three or more metabolic components, including elevated fasting glucose, high triglycerides, dyslipidemia, hypertension, and high waist circumference.
When focused on mortality due to obesity-related cancers, there were 165 total events over the observation period (Table 2). Among participants with normal weight, metabolically unhealthy participants were at more than a twofold increased risk of an obesity-related cancer death (adjusted HR: 2.40; 95% CI: 1.17-4.91) compared with metabolically healthy participants. There was no statistically significant risk of obesity-related cancer mortality for metabolically unhealthy participants with overweight (adjusted HR: 0.58; 95% CI: 0.30-1.12) or obesity (adjusted HR: 1.17; 95% CI: 0.68-2.02). Similar results were obtained in analyses unadjusted for comorbidities (data not shown). In both unadjusted (P = 0.0002) and adjusted models (P = 0.0232), the interaction terms between metabolic health status and obesity category were significant (data not shown).
In a sensitivity analysis excluding participants with comorbidities at baseline (n = 8,333; 49% of cancer deaths), a metabolically unhealthy status was associated with a statistically nonsignificant 42% increased risk of any cancer mortality among participants with normal weight; however, the association with obesity-related cancer mortality became stronger (HR: 3.31; 95% CI: 1.38-7.95). In a separate sensitivity analysis excluding participants who experienced a cancer death within the first 2 years of entry into the REGARDS cohort (n = 111), the association between metabolically unhealthy status and any cancer mortality among participants with normal weight became slightly attenuated but remained statistically significant (HR: 1.52; 95% CI: 1.07-2.16).
We further analyzed the association between BMI categories and any cancer mortality or obesity-related cancer mortality stratified by metabolic health status (Tables 3, 4. Participants with overweight (adjusted HR: 0.65; 95% CI: 0.54-0.79) or obesity (adjusted HR: 0.76; 95% CI: 0.61-0.94) had a reduced risk of any cancer mortality after adjusting for metabolic health status (Table 3). Metabolically healthy participants with overweight, but not obesity, were at a reduced risk of any cancer mortality compared with participants with normal weight (adjusted HR: 0.79; 95% CI: 0.63-0.99), while metabolically unhealthy participants with overweight (adjusted HR: 0.39; 95% CI: 0.27-0.55) or obesity (adjusted HR: 0.51; 95% CI: 0.36-0.70) were at a significantly reduced risk of any cancer mortality. The associations for obesity-related cancer mortality were mostly nonsignificant (Table 4).
| Any cancer deaths | ||||||
|---|---|---|---|---|---|---|
| Overall | Deaths/at risk (n) | Mortality ratea (95% CI) | Model 1b, HR (95% CI) | Model 1 subdistribution, HR (95% CI)c | Model 2d HR (95% CI) | Model 2 subdistribution, HR (95% CI)c |
| Normal weight (referent) | 256/5,377 | 7.33 (6.49-8.29) | - | - | - | - |
| Overweight | 255/8,351 | 4.58 (4.05-5.18) | 0.67 (0.55-0.81) | 0.69 (0.57-0.83) | 0.65 (0.54-0.79) | 0.67 (0.55-0.82) |
| Obesity | 255/8,786 | 4.48 (3.96-5.06) | 0.81 (0.67-0.98) | 0.82 (0.68-0.99) | 0.76 (0.61-0.94) | 0.78 (0.62-0.97) |
| Metabolically healthy | ||||||
| Normal weight (referent) | 199/4,720 | 6.45 (5.62-7.42) | - | - | - | - |
| Overweight | 167/5,503 | 4.50 (3.87-5.24) | 0.79 (0.63-0.99) | 0.83 (0.66-1.03) | - | - |
| Obesity | 71/2,872 | 3.76 (2.98-4.75) | 0.89 (0.66-1.20) | 0.91 (0.68-1.22) | - | - |
| Metabolically unhealthy | ||||||
| Normal Weight (Referent) | 57/657 | 13.94 (10.75-18.07) | - | - | - | - |
| Overweight | 88/2,848 | 4.74 (3.85-5.85) | 0.39 (0.27-0.55) | 0.39 (0.28-0.56) | - | - |
| Obesity | 184/5,914 | 4.83 (4.18-5.58) | 0.51 (0.36-0.70) | 0.51 (0.36-0.71) | - | - |
- a Rate per 1,000 person-years.
- b Adjusted for age, race, sex, education, income, tobacco use, alcohol use, physical inactivity, low-density lipoprotein cholesterol, and comorbidity score.
- c Estimated using Fine and Gray method, accounting for all-cause mortality as competing risk; models adjusted for age, race, sex, education, income, tobacco use, alcohol use, physical inactivity, low-density lipoprotein cholesterol, and comorbidity score.
- d Adjusted for age, race, sex, education, income, tobacco use, alcohol use, physical inactivity, low-density lipoprotein cholesterol, comorbidity score, and metabolic health status. Metabolically unhealthy defined as presence of three or more metabolic components, including elevated fasting glucose, high triglycerides, dyslipidemia, hypertension, and high waist circumference. Normal weight: BMI 18.5-24.9 kg/m2; overweight: BMI 25.0-29.9 kg/m2; obesity: BMI ≥ 30 kg/m2. Bold indicates statistically significant association at 0.05 alpha level.
| Obesity-related cancer deaths | ||||||
|---|---|---|---|---|---|---|
| Overall | Deaths/at risk (n) | Mortality ratea (95% CI) | Model 1b, HR (95% CI) | Model 1 subdistribution, HR (95% CI)c | Model 2d, HR (95% CI) | Model 2 subdistribution, HR (95% CI)c |
| Normal weight (referent) | 42/5,377 | 1.20 (0.19-1.63) | - | - | - | - |
| Overweight | 54/8,351 | 0.97 (0.74-1.27) | 0.86 (0.57-1.31) | 0.89 (0.58-1.35) | 0.85 (0.56-1.31) | 0.88 (0.56-1.37) |
| Obesity | 69/8,786 | 1.21 (0.96-1.53) | 1.32 (0.87-2.01) | 1.32 (0.87-2.01) | 1.29 (0.82-2.05) | 1.29 (0.79-2.09) |
| Metabolically healthy | ||||||
| Normal weight (referent) | 30/4,720 | 0.97 (0.68-1.39) | - | - | - | - |
| Overweight | 41/5,503 | 1.11 (0.81-1.50) | 1.29 (0.79-2.12) | 1.33 (0.82-2.17) | - | - |
| Obesity | 20/2,872 | 1.06 (0.68-1.64) | 1.50 (0.82-2.77) | 1.52 (0.83-2.80) | - | - |
| Metabolically unhealthy | ||||||
| Normal weight (referent) | 12/657 | 2.93 (1.67-5.17) | - | - | - | - |
| Overweight | 13/2,848 | 0.70 (0.41-1.21) | 0.27 (0.12-0.63) | 0.27 (0.12-0.64) | - | - |
| Obesity | 49/5,914 | 1.29 (0.97-1.70) | 0.65 (0.33-1.31) | 0.61 (0.30-1.25) | - | - |
- a Rate per 1,000 person-years.
- b Adjusted for age, race, sex, education, income, tobacco use, alcohol use, physical inactivity, and comorbidity score.
- c Estimated using Fine and Gray method, accounting for all-cause mortality as competing risk; models adjusted for age, race, sex, education, income, tobacco use, alcohol use, physical inactivity, low-density lipoprotein cholesterol, and comorbidity score.
- d Adjusted for age, race, sex, education, income, tobacco use, alcohol use, physical inactivity, comorbidity score, and metabolic health status. Metabolically unhealthy defined as presence of three or more metabolic components, including elevated fasting glucose, high triglycerides, dyslipidemia, hypertension, and high waist circumference. Normal weight: BMI 18.5-24.9 kg/m2; overweight: BMI 25.0-29.9 kg/m2; obesity: BMI ≥ 30 kg/m2. Bold indicates statistically significant association at 0.05 alpha level.
The cardiometabolic component that was most associated with any cancer mortality was reduced HDL cholesterol (overall adjusted HR: 1.20; 95% CI: 1.03-1.40), with the highest risk observed among participants with normal weight (adjusted HR: 1.89; 95% CI: 1.43-2.49) (Table 5). The cardiometabolic components most associated with obesity-related cancer mortality were reduced HDL cholesterol (adjusted HR: 2.45; 95% CI: 1.25-4.79) and elevated fasting glucose (adjusted HR: 2.00; 95% CI: 1.04-3.85). In addition, participants with normal weight with one (adjusted HR: 1.67; 95% CI: 1.08-2.57) and three or more (adjusted HR: 2.31; 95% CI: 1.44-3.72) cardiometabolic components were at a significantly increased risk of cancer mortality when compared with participants with no components. Participants with normal weight with at least three metabolically unhealthy components were at nearly a fourfold increased risk of obesity-related cancer mortality (adjusted HR: 3.78; 95% CI: 1.16-12.31) compared with those with none (Table 5).
| Obesity status | ||||
|---|---|---|---|---|
| All | Normal weight (BMI 18.5-24.9 kg/m2) | Overweight (BMI 25.0-29.9 kg/m2) | Obesity (BMI ≥ 30 kg/m2) | |
| Cancer mortality | ||||
| Componentsc | ||||
| High WC | 1.00 (0.86-1.17) | 1.21 (0.74-1.97) | 1.05 (0.79-1.39) | 1.37 (0.86-2.18) |
| Elevated triglycerides | 0.95 (0.80-1.13) | 1.10 (0.80-1.52) | 1.17 (0.88-1.56) | 0.75 (0.55-1.01) |
| Reduced HDL cholesterol | 1.20 (1.03-1.40) | 1.89 (1.43-2.49) | 0.84 (0.64-1.11) | 1.26 (0.97-1.65) |
| Elevated blood pressure | 1.14 (0.95-1.38) | 1.21 (0.90-1.62) | 1.03 (0.76-1.41) | 1.35 (0.89-2.05) |
| Elevated fasting glucose | 1.01 (0.87-1.18) | 1.01 (0.75-1.36) | 0.99 (0.76-1.30) | 1.14 (0.88-1.49) |
| Overalla | Ref | 0.67 (0.55-0.80) | 0.82 (0.68-0.99) | |
| Obesity-related cancer mortalityb | ||||
| Componentsc | ||||
| High WC | 1.29 (0.92-1.79) | 0.71 (0.17-3.06) | 0.86 (0.45-1.61) | 4.22 (1.02-17.40) |
| Elevated triglycerides | 0.87 (0.60-1.28) | 1.34 (0.62-2.88) | 0.89 (0.46-1.73) | 0.61 (0.33-1.10) |
| Reduced HDL cholesterol | 1.21 (0.87-1.68) | 2.45 (1.25-4.79) | 0.70 (0.38-1.31) | 1.15 (0.70-1.90) |
| Elevated blood pressure | 1.32 (0.88-1.98) | 1.17 (0.57-2.37) | 1.28 (0.64-2.55) | 1.36 (0.64-2.89) |
| Elevated fasting glucose | 1.20 (0.87-1.66) | 2.00 (1.04-3.85) | 1.04 (0.59-1.83) | 0.94 (0.58-1.54) |
| Overalla | Ref | 0.86 (0.57-1.31) | 1.32 (0.87-2.01) | |
| Cancer mortality | ||||
| Number of metabolically unhealthy components | ||||
| 0 (Referent) | - | - | - | - |
| 1 | 1.31 (0.94-1.82) | 1.67 (1.08-2.57) | 1.07 (0.62-1.84) | 0.78 (0.17-3.56) |
| 2 | 1.28 (0.92-1.77) | 1.48 (0.93-2.36) | 1.13 (0.67-1.93) | 1.13 (0.27-4.65) |
| 3+ | 1.29 (0.95-1.77) | 2.31 (1.44-3.72) | 0.95 (0.56-1.62) | 1.18 (0.29-4.77) |
| P value for trend | 0.41 | < 0.01 | 0.74 | 0.65 |
| Obesity-related cancer mortalityb | ||||
| Number of metabolically unhealthy components | ||||
| 0 (Referent) | - | - | - | - |
| 1 | 2.25 (0.94-5.40) | 1.74 (0.56-5.40) | 2.85 (0.66-12.36) | Undefined |
| 2 | 2.72 (1.15-6.39) | 1.92 (0.59-6.28) | 2.68 (0.62-11.62) | Undefined |
| 3+ | 2.65 (1.14-6.15) | 3.78 (1.16-12.31) | 1.41 (0.31-6.45) | Undefined |
| P value for trend | 0.12 | 0.10 | 0.15 | 0.46 |
- a Models adjusted for age, sex, race, education, income, tobacco use, alcohol use, physical inactivity, and comorbidity score.
- b 165 obesity-related cancer deaths included breast, colorectal, kidney, pancreatic, endometrial, and esophageal cancers.
- c Referent groups for each hazard ratio is absence of metabolic component. 766 cancer deaths. Bold indicates statistically significant association at 0.05 alpha level.
- WC, waist circumference; HDL, high-density lipoprotein.
Discussion
In this large prospective cohort of black and white adults, we observed that metabolic health status was a strong predictor of cancer mortality among participants with normal weight. Metabolically unhealthy participants experienced a significantly higher risk of cancer mortality during follow-up compared with metabolically healthy participants in the normal weight category, with an observed 65% increased risk. In addition, metabolically unhealthy participants with normal weight were at a twofold increased risk of obesity-related cancer mortality compared with those who were metabolically healthy. Among participants with overweight and obesity, there was no significantly increased risk of cancer mortality because of a metabolically unhealthy status observed after adjusting for age, sex, income, tobacco use, alcohol use, and physical activity at baseline. However, when restricted to the major obesity-related cancers (breast, colorectal, kidney, pancreatic, endometrial, and esophageal cancers), there was a twofold increased risk of mortality observed among metabolically unhealthy versus metabolically healthy participants with normal weight. Participants with normal weight and at least three altered cardiometabolic components had almost a twofold (all cancers) to more than a threefold (obesity-related cancers) increased risk of cancer mortality compared with participants with none. Low HDL cholesterol was the cardiometabolic risk factor most consistently associated with the risk of cancer mortality, while elevated fasting glucose was also important for obesity-associated cancer mortality, suggesting a likely biological mechanism linking metabolic health status and cancer mortality.
There has been increasing recognition of the importance of metabolic factors in influencing health risks and mortality outcomes (9, 20-22). Metabolic dysregulation, in addition to chronic inflammation, genomic alterations, and immune system dysfunction, has been shown to influence cancer etiology and mortality, and an increasing number of studies have begun to directly assess the mechanisms through which metabolic dysfunction affects cancer outcomes independent of body weight, with mixed results (12, 13). A 2012 study of more than 22,000 adults in England and Scotland observed that metabolically healthy adults with obesity were not at an increased risk of cancer mortality compared with metabolically healthy adults without obesity, while all adults (regardless of obesity status) with two or more metabolic risk factors (i.e. metabolically unhealthy) had a 59% to 64% increased risk of mortality (23). Similarly, a 2014 study among Korean adults observed that regardless of BMI category, metabolically unhealthy participants were at a significantly higher risk for cancer mortality compared with metabolically healthy adults (12). In contrast, a 2013 systematic review and meta-analysis concluded that adults with obesity were at an increased risk for mortality compared with adults with normal weight, even in the absence of metabolic abnormalities (22).
We observed a significant association between reduced HDL cholesterol and cancer mortality among participants. This suggests that the biological mechanism linking obesity, metabolic dysregulation, and cancer mortality may involve dyslipidemia, and clinical strategies focused on cholesterol management may provide added benefits to cancer patients in addition to other strategies, such as exercise and dietary recommendations, to reduce metabolic dysfunction. Other studies have observed a reduced risk of cancer with increased HDL cholesterol (24, 25), while some studies have suggested that the HDL-apolipoprotein ratio may be a stronger indicator of the risk of cancer mortality (24). Future work in this area is warranted, as very few studies have directly examined HDL cholesterol levels and cancer-specific mortality prospectively. Another potential biological mechanism for this association may be through the relationship between insulin resistance and liver fat content, which may act as an independent risk factor for cancer mortality separate from the well-established association with visceral fat mass. Several studies have observed that higher liver fat content and nonalcoholic fatty liver disease increase the risk of cardiovascular diseases (26) and type 2 diabetes (27, 28), via insulin resistance, independent of visceral fat mass. This may be an important underlying mechanism for the higher risk of cancer mortality among metabolically unhealthy individuals with normal weight. Research studies focused on assessing liver fat content in addition to visceral fat among metabolically unhealthy adults may further shed light on this mechanism. Other potential mechanisms include inflammatory profile imbalance because of increased adiposity and genetic or epigenetic changes, which are important consequences of altered metabolic components, such as obesity, dyslipidemia, and high blood pressure, and may play an important role in the function of the genes responsible for tumor angiogenesis, apoptosis, or metastasis.
Though still the subject of much debate, there is compelling evidence that obesity status itself may be a less informative risk or prognostic factor for many diseases, including cancer. In fact, our findings as well as others (29, 30) have indicated that metabolic health status may be a more important cancer prognostic factor that should be evaluated in addition to obesity. We observed a consistently higher risk of cancer mortality among metabolically unhealthy participants with normal weight, with associations that were significantly higher when focused on obesity-related cancers. In addition, regardless of metabolic health status, we observed a lower risk of cancer death among participants with overweight and obesity. There is a large body of literature regarding the role of inflammation in cancer prognosis (31, 32), and our observation that the metabolic health components most associated with mortality were reduced HDL cholesterol and elevated fasting glucose supports the hypothesis that tissue inflammation and insulin resistance, rather than obesity per se, is associated with cancer prognosis. However, considerable debate remains regarding the direct effects of obesity, versus mediating factors such as inflammation and/or metabolic dysregulation, on cancer mortality. Future prospective studies of cancer will be needed to definitively identify which risk factors are most strongly associated with cancer mortality and can be valuable targets of clinical interventions for cancer patients.
There are some limitations to this research. First, there are currently no established criteria for defining metabolically healthy obesity, and this analysis was based on the definition proposed in the joint harmonized criteria for metabolic syndrome. It is impossible to assess whether our definition overestimated or underestimated the prevalence of metabolic health. However, by using a strict criterion of three out of five altered metabolic components, we reduced the likelihood of overestimation, and our results did not change significantly after a sensitivity analysis using two out of five components to define metabolic health. Second, metabolic health and BMI category were assessed at baseline, and while this reduced the likelihood of reverse causality bias, it is likely that metabolic health and/or BMI category changed over the course of follow-up. However, by excluding participants with a history of cancer at baseline, we further reduced the likelihood of reverse causality. There were likely some participants who were classified as “cancer-free” at baseline but who had undiagnosed cancer; this may lead to biased estimates, especially if those participants are more likely to have normal weight. To address this possibility, we conducted a sensitivity analysis excluding all cancer deaths occurring in the first 2 years after entry into the cohort, and our results remained consistent. We expect that these changes will be nondifferential in relation to baseline metabolic health or BMI status and that our observed estimates will likely underestimate the true association between metabolic health status and cancer mortality within the REGARDS cohort. In addition, we observed stronger associations between metabolic health status and cancer mortality when focused on obesity-related cancers, and this association became stronger when excluding participants with comorbidities at baseline. Third, our cohort had only up to 10 years of follow-up time, limiting our availability to observe cancer-specific deaths that will occur as the cohort ages. Fourth, even though REGARDS is a large prospective cohort study with more than 30,000 participants, we were limited by the number of cancer mortality events observed, which inhibited our ability to conduct race- and sex-stratified analyses. The strengths of this analysis included the use of a large prospective cohort study and cancer mortality outcomes obtained by using standardized adjudication techniques that minimized the chances of outcome misclassification. Baseline measures of obesity and metabolic health components were directly measured by highly trained interviewers during in-home visits and were therefore less vulnerable to misclassification or recall bias.
In conclusion, we provide evidence that metabolic health status is an important prognostic factor for cancer among adults with normal weight. Longer follow-up times in the REGARDS cohort will enable us to better characterize this association by cancer type, in different racial and sex groups, and to better evaluate the biological mechanisms underlying this association in order to inform specific strategies to reduce the risk. Meanwhile, clinical and public health strategies to reduce obesity and improve metabolic health status among metabolically unhealthy adults, especially adults with normal weight, may go a long way in improving cancer outcomes specifically, and health outcomes in general, among US patients.





