Metabolic Benefits of Prior Weight Loss with and without Exercise on Subsequent 6-Month Weight Regain
Funding agencies: This research was supported by funds from a Senior Research Career Scientist Award (ASR) and a Career Development Award IK2RX-000944 (MCS) from the United States Department of Veterans Affairs Rehabilitation Research and Development Service and the Geriatric Research, Education and Clinical Center at the Baltimore Veterans Affairs Medical Center and by the National Institutes of Health grants R01-AG19310, R01-AG20116, P30-AG028747, and P30-DK072488.
Disclosure: The authors declared no conflict of interest.
Clinical trial registration: ClinicalTrials.gov identifier NCT00882141.
Abstract
Objective
To determine the 6-month follow-up effects after intentional 6-month weight loss alone (WL) and after weight loss with aerobic exercise (AEX + WL) on body composition, glucose metabolism, and cardiovascular disease risk factors in older postmenopausal women and to identify the mechanisms for weight regain.
Methods
Women (n = 65, BMI > 25 kg/m2) underwent maximal oxygen consumption testing, dual-energy x-ray absorptiometry, computed tomography scans, and oral glucose tolerance tests before and after 6 months of AEX + WL or WL and at 12 months ad libitum follow-up. Insulin sensitivity (M) (hyperinsulinemic-euglycemic clamp) was measured at baseline and 6 months. Thirty WL and thirty-five AEX + WL women completed a follow-up at 12 months.
Results
Similar weight loss was observed (−8%) in both groups from 0 to 6 months. Total fat mass, fat-free mass, visceral fat area, subcutaneous abdominal and midthigh fat areas, fasting glucose, insulin levels, homeostatic model assessment of insulin resistance (HOMA-IR), insulin areas under the curve, and triglyceride levels decreased similarly after WL and AEX + WL and remained lower at 12 months than at baseline, despite weight regain at 12 months. Initial M was associated with weight regain (r = −0.40, P < 0.01). Weight regain was related to independent changes in leptin and HOMA-IR from 6 to 12 months in a multiple regression model (r = 0.77, P < 0.0001).
Conclusions
Reductions in body fat and improvements in insulin sensitivity after AEX + WL and WL were maintained at 12 months despite modest weight regain. Baseline insulin resistance partially predicted the magnitude of weight regain in postmenopausal women.
Introduction
Overweight and obesity, present in more than half of all middle-aged and older women (1), are associated with the development of type 2 diabetes (2). Weight loss of as little as 3% reduces the risk for the development of type 2 diabetes and reduces obesity-associated cardiovascular risk factors (3). Yet in adults who participate in weight loss studies, most subjects regain almost half the weight lost within the following 2 years and return to baseline weight within the next 3 to 5 years (4-6). Thus, long-term success in maintaining the reduced weight is a challenge.
Successful weight maintenance is likely multifactorial, dependent on both environmental and psychological factors such as dietary strategies (length of time weight loss is maintained, self-monitoring weight, eating breakfast), physical activity (∼1 h/d), and having low levels of depression and disinhibition (7). Other predictors associated with weight maintenance following weight loss have included meal provision, type of diet, genetic factors, resting energy expenditure, and certain hormones (8-12). Adipose tissue hormones, including leptin, as well as gut hormones and neuropeptides affect appetite and, thus, influence energy balance (13, 14). Leptin has beneficial effects on glucose metabolism by decreasing glycemia, insulinemia, and insulin resistance. There is also some evidence that insulin sensitivity (M) predicts weight gain (15, 16), although limited studies (16) have utilized the measurement of M by the glucose clamp to examine this relationship and others have suggested that changes in M during weight loss do not predict weight regain (17).
Weight regain may be accompanied by deterioration in cardiovascular disease (CVD) risk factors back to baseline (18, 19). Increases in total cholesterol, triglycerides, glucose, insulin, and homeostatic model assessment of insulin resistance (HOMA-IR) in postmenopausal women are directly associated with weight regain (20). Given the importance of abdominal fat in cardiovascular risk, it is possible that alterations in central body fat are important in the worsening of metabolic risk associated with weight regain.
We hypothesized that postmenopausal women who initially participate in a 6-month intervention of weight loss combined with aerobic exercise (AEX + WL) will have less weight regain and better metabolic profiles over a 6-month follow-up than women who initially participate in a weight loss only (WL) intervention. The aim of this study was to determine the 6-month follow-up effects after intentional 6-month WL or AEX + WL on body composition, glucose metabolism, and CVD risk factors in older postmenopausal women. We also investigated potential mechanisms for weight regain by examining the role of leptin and M by hyperinsulinemic-euglycemic clamps.
Methods
Subjects
Subjects were African American and Caucasian women with overweight and obesity (BMI > 25 kg/m2; range: 25-47 kg/m2) aged 45 to 76 years from the Baltimore/Washington area. Women had not menstruated for at least 1 year and were weight stable (< 2-kg weight change in past year) and sedentary (< 20 min of aerobic exercise two times per week). Individuals with untreated hypertension or hyperlipidemia were referred to their doctor for evaluation and entered the study if they were treated with an antihypertensive or lipid-lowering drug that did not affect glucose metabolism, were stable on the medications for at least 3 months, and agreed to remain on the medication throughout the study. Subjects were nonsmokers; showed no evidence of cancer, liver, renal, or hematological disease, or other medical disorders; and underwent a Bruce graded treadmill test to exclude those with asymptomatic coronary artery disease. A total of 103 women completed the initial study (WL, n = 50 and AEX + WL, n = 53) (21). Of these women, 65 (n = 30 in WL and n = 35 in AEX + WL) women (20 African American, 11 WL, 9 AEX + WL and 45 Caucasian, 24 WL, 21 AEX + WL) returned at the 1-year mark for testing (Figure 1). Body composition and hyperinsulinemic-euglycemic clamp results were published before and after 6 months of AEX + WL and WL (21); however, the 12-month follow-up effects were not examined. Data are presented only for those who had some 12-month follow-up testing. Each participant provided written informed consent approved by the University of Maryland Baltimore Institutional Review Board.
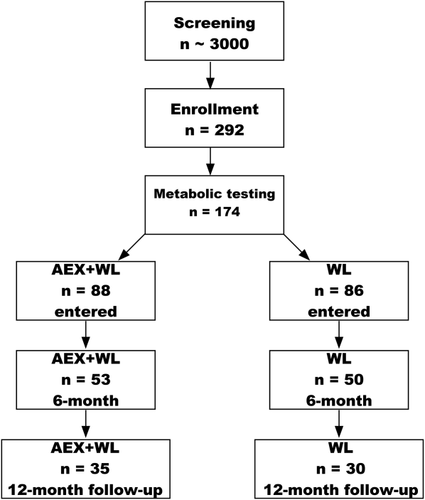
CONSORT diagram.
Procedures
Subjects received instruction in maintaining a weight-stable Therapeutic Lifestyle Changes (TLC) diet (22) (consuming < 30% of total calories as total fat, 10% as saturated fat, 300 mg of cholesterol, and 2,400 mg of sodium per day) from a registered dietitian (RD) 1 d/wk for 6 to 8 weeks prior to initial testing. Subjects were weight stable ± 2% on the TLC diet for at least 2 weeks prior to the initial, 6-month, and 12-month testing. AEX + WL subjects had all metabolic tests performed 24 to 36 hours after the last exercise session.
Maximal oxygen consumption and body composition
Maximal oxygen consumption (VO2max) was measured by using a continuous treadmill test protocol (21). Fat mass, lean tissue mass, and bone mineral content (fat-free mass [FFM] = lean + bone) were determined by dual-energy x-ray absorptiometry (Prodigy, LUNAR Radiation Corp., Madison, Wisconsin). A single computed tomography scan (Siemens SOMATOM Sensation 64 Scanner, Fairfield, Connecticut) at the L4 to L5 region was used to determine visceral and subcutaneous abdominal adipose tissue area and analyzed by using Medical Image Processing, Analysis and Visualization version 7.0.0 (NIH Center for Information Technology, Bethesda, Maryland). A second scan of the right midthigh was used to quantify intramuscular fat area (low-density lean tissue), subcutaneous fat, and muscle area (21).
Fasting blood draw and oral glucose tolerance test
Blood samples were drawn after a 12-hour fast and at 30-minute intervals for 2 hours after ingestion of 75 g of glucose. Plasma glucose concentrations were measured by using the glucose oxidase method (2300 STAT Plus, YSI, Yellow Springs, Ohio), and plasma insulin and leptin were measured by radioimmunoassay (Millipore, St. Charles, Missouri). HOMA-IR was calculated as ([fasting insulin (µU/mL) × fasting glucose (mmol/L)] / 22.5) (23). All samples were measured in duplicate. Glucose tolerance status (24) was determined for each subject by using American Diabetes Association criteria. Plasma triglyceride and cholesterol levels were averaged from three fasting blood draws analyzed by using enzymatic methods (UniCel DxC 880i, Beckman Coulter, Inc., Brea, California) (25, 26), and high-density lipoprotein cholesterol (HDL-C) was measured in the supernatant after precipitation with dextran sulfate (low-density lipoprotein cholesterol [LDL-C] = total cholesterol − [triglyceride level / 5 + HDL-C]) (27).
Indirect calorimetry
Subjects reported to our lab first thing in the morning after a 12-hour fast. Resting metabolic rate (RMR) was measured for 30 minutes under a canopy in a thermoneutral environment with indirect calorimetry conducted by using a SensorMedics DeltaTrac (Yorba Linda, California). Energy expenditure was calculated by using the Weir equation (28).
Hyperinsulinemic-euglycemic clamps
Subjects were provided with meals based on a eucaloric diet for 2 days before the clamp to control nutrient intake. Testing was performed in the morning after a 12-hour fast. Whole-body M was measured during a 180-minute 80 mU/m−2/min−1 (Humulin R, Eli Lilly Co., Indianapolis, Indiana) hyperinsulinemic-euglycemic clamp (29, 30) in 45 women (n = 20 WL, n = 25 AEX + WL). Subject characteristics were not different between those who underwent the clamp and those who did not (data not shown). M was calculated from the amount of glucose infused after correction for glucose equivalent space (glucose space correction) and expressed per kilogram of FFM. The glucose clamp was conducted before and after the 6-month AEX + WL and WL but not at the 12-month follow-up.
Interventions
Women in the AEX + WL and WL groups attended weekly weight loss classes led by a RD for instruction in the principles of a hypocaloric diet (−500 kcal/d) according to TLC guidelines. Weight loss instructions included following the “heart healthy” dietary modification guidelines plus beginning a 250 to 350 kcal/d hypocaloric diet with a goal of ∼5% to 10% weight loss over the study duration. Diets were monitored with 7-day food records using the American Diabetes Association exchange list system. In addition to the weight loss classes, women in the AEX + WL group also exercised on a treadmill three times per week at our facility. Each exercise session included a 5- to 10-minute warm-up phase and a 5- to 10-minute cooldown phase. Exercise intensity was prescribed to a target heart rate, and heart rate was monitored each session by using monitors (Polar Electro Inc., Lake Success, New York). The duration of exercise began with 30-minute sessions at ∼50% to 60% of heart rate reserve and progressed to > 85% for 45 to 50 minutes for the 6 months (21). Average compliance to the exercise sessions was 87% and average compliance to the diet classes was 86% in months 0 to 6. During the 6-month follow-up period, women were given the option of attending a 1-hour, face-to-face, monthly group nutrition class focused on the principles of the TLC diet, and women were encouraged to continue monitoring intake; however, attendance and food recording were optional. Class topics refreshed participants' knowledge and included the following: coping with slips and binges, problem solving, healthy habits, self-talk, and stress management. The AEX + WL group could use the exercise facility three times per week for 1 hour if desired where only exercise safety, and not the exercise prescription or exercise intensity, was monitored. Women in the AEX + WL group attended ∼27% of the exercise sessions and women attended ∼29% of the RD sessions per month during the follow-up.
Data analysis
Statistics were run only on subjects who completed 0-, 6-, and 12-month evaluations. Some women did not complete all testing at the 12-month evaluation; sample sizes were equal across each time point for each variable, but not all variables had the same sample size. Statistical analyses were performed by using a two-way analysis of variance (ANOVA) with AEX + WL and WL as in-between variables and time as a within variable. The Bonferroni post hoc test was used when the overall effects were significant. Pearson correlations and multiple regressions were used to assess relationships between key variables. Statistical significance was set at a two-tailed P < 0.05. Data were analyzed by using SPSS Statistics (IBM Corp., Armonk, New York); results were expressed as mean ± SEM.
Results
Effects on body weight and composition
Weight and body fat did not differ between groups at baseline (Table 1). There were no group × time or group effects on body weight or body composition measured by dual-energy x-ray absorptiometry. There was a significant time effect for body weight, BMI, % fat, fat mass, and FFM. Both groups lost ∼8% (P < 0.0001) of their body weight at 6 months, regained ∼1%, and thus maintained a significant loss of 7% at 12 months (P < 0.001). Mean weight gain from 6 to 12 months was 1.7 ± 0.6 kg for WL and 1.6 ± 0.4 kg for AEX + WL. The relationship between the change in weight between 0 to 6 months and between 6 to 12 months was not significant (r = 0.08, P = 0.54), indicating that those who lost the most weight initially were not the same individuals who had the greatest weight regain. The reduction in BMI, % fat, fat mass, and FFM with WL and AEX + WL at 6 months remained significant at 12 months (Table 1).
| Baseline | 6 months | 12 months | Group × time | Overall group | Overall time | 6 vs. 0 | 12 vs. 6 | 12 vs. 0 | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean ± SEM | Mean ± SEM | Mean ± SEM | P | P | P | P | P | P | ||
| Weight (kg) | WL | 35 | 88 ± 3 | 80 ± 2 | 82 ± 3 | 0.98 | 0.17 | 0.000 | < 0.001 | < 0.001 | < 0.001 |
| AEX + WL | 30 | 83 ± 3 | 75 ± 2 | 77 ± 3 | |||||||
| BMI (kg/m2) | WL | 35 | 33.2 ± 0.9 | 30.3 ± 0.9 | 31.0 ± 0.9 | 0.96 | 0.23 | 0.000 | < 0.001 | < 0.001 | < 0.001 |
| AEX + WL | 30 | 31.7 ± 1.0 | 28.8 ± 0.9 | 29.4 ± 1.0 | |||||||
| Total body fat (%) | WL | 28 | 47.1 ± 0.8 | 43.8 ± 1.2 | 45.0 ± 1.1 | 0.39 | 0.61 | 0.000 | < 0.001 | < 0.001 | < 0.001 |
| AEX + WL | 23 | 47.1 ± 1.0 | 42.7 ± 1.3 | 43.8 ± 1.3 | |||||||
| Fat mass (kg) | WL | 28 | 41.1 ± 1.9 | 35.4 ± 2.0 | 36.4 ± 2.0 | 0.39 | 0.67 | 0.000 | < 0.001 | < 0.001 | < 0.001 |
| AEX + WL | 23 | 40.3 ± 2.1 | 33.5 ± 2.2 | 35.2 ± 2.3 | |||||||
| FFM (kg) | WL | 28 | 45.3 ± 1.2 | 43.8 ± 1.1 | 43.4 ± 1.2 | 0.13 | 0.78 | 0.000 | < 0.001 | < 0.001 | < 0.001 |
| AEX + WL | 23 | 44.4 ± 1.4 | 43.2 ± 1.2 | 43.5 ± 1.3 | |||||||
| Midthigh muscle area (cm2) | WL | 27 | 72.4 ± 2.8 | 69.9 ± 2.8 | 70.0 ± 3.0 | 0.001 | 0.38 | 0.43 | 0.08 | 0.93 | 0.20 |
| AEX + WL | 20 | 71.1 ± 2.8 | 76.2 ± 2.7* | 75.7 ± 3.3 | < 0.01 | 0.99 | < 0.05 | ||||
| Midthigh subcutaneous fat area (cm2) | WL | 27 | 157.0 ± 8.9 | 131.5 ± 8.3 | 139.1 ± 8.1 | 0.54 | 0.78 | 0.000 | < 0.001 | < 0.001 | < 0.001 |
| AEX + WL | 20 | 150.2 ± 11.0 | 131.0 ± 10.1 | 135.6 ± 11.0 | |||||||
| Midthigh intramuscular fat area (cm2) | WL | 27 | 20.1 ± 1.5 | 19.4 ± 1.7 | 20.9 ± 1.9 | 0.12 | 0.76 | 0.56 | 0.81 | 1.0 | 1.0 |
| AEX + WL | 20 | 20.1 ± 1.4 | 19.6 ± 1.5 | 18.6 ± 1.5 | |||||||
| RMR (kcal/d) | WL | 21 | 1,472 ± 53 | 1,388 ± 59 | 1,446 ± 52 | 0.94 | 0.75 | 0.03 | < 0.01 | < 0.05 | 0.41 |
| AEX + WL | 17 | 1,447 ± 59 | 1,355 ± 66 | 1,433 ± 57 | |||||||
| VO2max (L/min) | WL | 12 | 1.52 ± 0.10 | 1.44 ± 0.06 | 1.38 ± 0.07 | 0.04 | 0.02 | 0.02 | 0.14 | 0.29 | 0.09 |
| AEX + WL | 17 | 1.80 ± 0.11* | 1.95 ± 0.15† | 1.65 ± 0.08* | < 0.05 | < 0.01 | < 0.05 | ||||
- *P < 0.05, †P < 0.001, AEX + WL vs. WL.
There were no baseline differences between groups. There was a group × time interaction in muscle area (P < 0.001), which increased at 6 months after AEX + WL (P < 0.01), did not significantly change from 6 to 12 months, and remained higher at 23 months (P < 0.05) than at baseline. Midthigh muscle area did not change after 6 or 12 months in the WL group. There were no group × time or group effects for other computed tomography outcomes. There were no significant changes in low-density lean tissue area after WL and AEX + WL at 6 or 12 months. The reductions in visceral fat areas were comparable at 20% and 18% after WL and AEX + WL at 6 months (P < 0.0001) and remained significantly lower at 12 months than initially, despite an insignificant increase of 8.1% in the WL group and 1.3% in the AEX + WL group from 6 to 12 months (Figure 2). Subcutaneous abdominal fat area also decreased after WL and AEX + WL at 6 months (−14 and −15%, P < 0.0001) and was still reduced at 12 months (P < 0.0001, Figure 2). Overall, midthigh subcutaneous fat decreased at 6 months post WL or post AEX + WL (P < 0.001) and was higher at 12 months than at 6 months (P < 0.001), but it remained lower at 12 months than at baseline (P < 0.001).
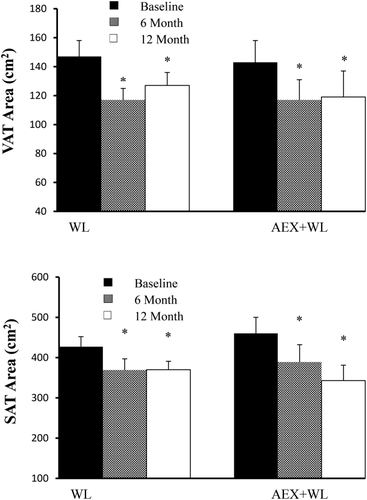
Visceral fat (VAT) area and subcutaneous fat (SAT) area at baseline, 6 months, and 12-month follow-up in WL and AEX + WL groups. *P < 0.0001 versus baseline.
Effects on VO2max
There was a group × time interaction for VO2max (P < 0.05). VO2max increased 8% with AEX + WL (P < 0.05), which was significantly different (P < 0.05) than the 4% decrease with WL. VO2max declined 13% from 6 to 12 months in the AEX + WL group (P < 0.001), such that it was no longer different than the initial VO2max. In the WL group, VO2max decreased another 4% from 6 to 12 months, although this was not significant. Both groups had an overall −7% change in VO2max over the year.
Effects on blood parameters
There were no baseline differences between groups, group × time interactions, or group effects for triglycerides, total cholesterol, LDL-C, or HDL-C (Table 2). Overall, triglyceride levels decreased after 6 months of WL and AEX + WL (P < 0.01), did not change from 6 to 12 months, and were lower at 12 months than baseline (P < 0.01). Total cholesterol and LDL-C decreased at 6 months (both P < 0.005). Overall, there was a significant increase from 6 to 12 months in total cholesterol (P < 0.005) and LDL-C (P < 0.01). Total cholesterol and LDL-C were not different between 12 months and baseline. Overall, HDL-C increased at 6 months (P < 0.01), was higher at 12 months than at 6 months (P < 001), and remained higher at 12 months compared with baseline (P < 0.001). There was not a group × time interaction or group effect for plasma leptin, which decreased overall from baseline to 6 months (P < 0.001), increased from 6 to 12 months (P < 0.005), and was not different at 12 months than at baseline (P = 0.09).
| Baseline | 6 months | 12 months | Group × time | Overall group | Overall time | 6 vs. 0 | 12 vs. 6 | 12 vs. 0 | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean ± SEM | Mean ± SEM | Mean ± SEM | P | P | P | P | P | P | ||
| Triglycerides (mg/dL) | WL | 34 | 128 ± 11 | 113 ± 9 | 107 ± 8 | 0.49 | 0.24 | 0.000 | < 0.01 | 1.0 | < 0.01 |
| AEX + WL | 28 | 117 ± 7 | 94 ± 6 | 94 ± 6 | |||||||
| Cholesterol (mg/dL) | WL | 34 | 197 ± 7 | 192 ± 6 | 204 ± 8 | 0.49 | 0.50 | 0.000 | < 0.005 | < 0.005 | 1.0 |
| AEX + WL | 28 | 198 ± 6 | 186 ± 5 | 194 ± 7 | |||||||
| LDL-C (mg/dL) | WL | 34 | 121 ± 6 | 116 ± 5 | 128 ± 7 | 0.35 | 0.99 | 0.000 | < 0.005 | < 0.01 | 1.0 |
| AEX + WL | 28 | 123 ± 5 | 112 ± 4 | 118 ± 6 | |||||||
| HDL-C (mg/dL) | WL | 34 | 55 ± 2 | 57 ± 2 | 61 ± 2 | 0.75 | 0.38 | 0.000 | < 0.01 | < 0.01 | < 0.001 |
| AEX + WL | 28 | 52 ± 2 | 55 ± 2 | 57 ± 2 | |||||||
| Fasting glucose (mg/dL) | WL | 31 | 99 ± 2 | 92 ± 2 | 92 ± 2 | 0.30 | 0.41 | 0.000 | < 0.001 | 1.0 | < 0.001 |
| AEX + WL | 25 | 95 ± 2 | 90 ± 2 | 92 ± 2 | |||||||
| Fasting insulin (pmol/L) | WL | 26 | 93 ± 7 | 71 ± 5 | 72 ± 6 | 0.96 | 0.24 | 0.000 | < 0.001 | 1.0 | < 0.01 |
| AEX + WL | 18 | 80 ± 9 | 59 ± 5 | 58 ± 5 | |||||||
| HOMA-IR | WL | 25 | 3.75 ± 0.31 | 2.75 ± 0.23 | 2.77 ± 0.26 | 0.99 | 0.28 | 0.000 | < 0.001 | 1.0 | < 0.005 |
| AEX + WL | 18 | 3.16 ± 0.37 | 2.24 ± 0.22 | 2.21 ± 0.20 | |||||||
| Glucose AUC (mg/dL·120 min) | WL | 31 | 17,578 ± 645 | 16,492 ± 570 | 17,080 ± 661 | 0.22 | 0.12 | 0.01 | < 0.05 | 1.0 | < 0.05 |
| AEX + WL | 25 | 16,364 ± 718 | 15,670 ± 634 | 15,068 ± 736 | |||||||
| Insulin AUC (pmol/liter·120 min ) | WL | 25 | 51,258 ± 3,947 | 43,207 ± 3,176 | 44,883 ± 3,457 | 0.09 | 0.63 | 0.000 | < 0.001 | 1.0 | < 0.001 |
| AEX + WL | 18 | 55,466 ± 4,651 | 41,066 ± 3,743 | 36,120 ± 4,075 | |||||||
| Leptin (ng/mL) | WL | 15 | 29.2 ± 2.6 | 22.8 ± 2.4 | 28.9 ± 3.3 | 0.27 | 0.08 | 0.000 | < 0.001 | < 0.005 | 0.09 |
| AEX + WL | 21 | 25.4 ± 2.2 | 17.8 ± 2.0 | 20.1 ± 2.8 | |||||||
| Systolic blood pressure (mm Hg) | WL | 19 | 120 ± 3 | 114 ± 3 | 116 ± 3 | 0.93 | 0.90 | 0.003 | < 0.01 | 0.49 | 0.62 |
| AEX + WL | 20 | 118 ± 3 | 114 ± 4 | 117 ± 4 | |||||||
| Diastolic blood pressure (mm Hg) | WL | 19 | 66 ± 2 | 64 ± 2 | 66 ± 2 | 0.57 | 0.88 | 0.07 | 0.06 | 1.0 | 0.50 |
| AEX + WL | 20 | 68 ± 2 | 65 ± 2 | 65 ± 2 | |||||||
Effects on glucose metabolism
Fasting and total areas under the curve (AUCs) for glucose and insulin, leptin, and HOMA-IR were not different at baseline between groups (Table 2). There were not any group × time interactions or group effects. Fasting glucose, fasting insulin, and HOMA-IR decreased after 6 months (P < 0.001) and did not change from 6 to 12 months. Overall, fasting glucose (P < 0.001), fasting insulin (P < 0.01), and HOMA-IR (P < 0.005) remained lower at 12 months than at baseline. Likewise, total insulin AUC decreased at 6 months (P < 0.001), did not significantly change from 6 to 12 months, and remained lower at 12 months than at baseline (P < 0.001). Total glucose AUC also decreased from baseline to 6 months (P < 0.05), did not change from 6 to 12 months, and remained lower at 12 months (P < 0.05). There was no group × time interaction for M (WL: 61.6 ± 4.2 vs. 64.1 ± 4.0 µmol·
 and AEX + WL: 67.6 ± 3.4 vs. 75.4 ± 3.4 µmol·
and AEX + WL: 67.6 ± 3.4 vs. 75.4 ± 3.4 µmol·
 ), which increased from baseline to 6 months (64.9 ± 2.6 vs. 70.4 ± 2.7 µmol·
), which increased from baseline to 6 months (64.9 ± 2.6 vs. 70.4 ± 2.7 µmol·
 , P < 0.05).
, P < 0.05).
Effects on RMR
There were no group × time interaction or group effects for RMR. RMR declined after WL and AEX + WL (P < 0.01), increased from 6 to 12 months (P < 0.05), and was not different at 12 months from the baseline (P = 0.41).
Baseline predictors of weight regain (6 to 12 months)
Initial M was associated with weight change/regain (r = −0.40, P < 0.01, Figure 3). Initial RMR was also associated with weight change/regain (r = 0.27, P < 0.05). However, baseline VO2max, fasting glucose, insulin, leptin, glucose120min, and glucose and insulin AUCs were not associated with weight change/regain (r = −0.01 to 0.10, P = 0.97 to 0.12). In a multiple regression model with baseline leptin and M, only baseline M was independently correlated with weight change/regain (r2 = 0.18, P < 0.05). Compliance with the exercise sessions from 6 to 12 months was associated with less weight change/regain from 6 to 12 months in the AEX + WL group (r = −0.44, P < 0.05).
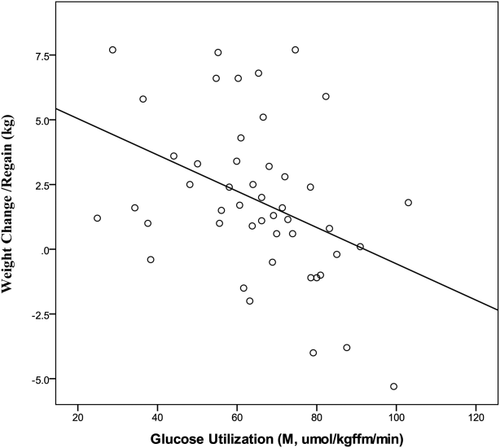
Relationship of M to weight regain in postmenopausal women. (r = −0.40, P = 0.005).
Metabolic changes associated with weight regain (6 to 12 months)
Weight change/regain was associated with an increase in fasting glucose, insulin, leptin, insulin at 120 minutes, insulin AUC, and HOMA-IR from 6 to 12 months (Table 3). Weight change/regain was not associated with the change in VO2max. Weight change/regain was related to independent changes in leptin and HOMA-IR from 6 to 12 months in a multiple regression model (r = 0.77, P < 0.0001).
| ΔWeight r | P | |
|---|---|---|
| ΔFasting glucose | 0.26 | 0.05 |
| ΔFasting insulin | 0.42 | 0.004 |
| ΔFasting leptin | 0.61 | 0.0001 |
| ΔGlucose @120min | 0.14 | 0.31 |
| ΔInsulin @120min | 0.39 | 0.008 |
| ΔGlucose AUC | 0.20 | 0.15 |
| ΔInsulin AUC | 0.39 | 0.01 |
| ΔRMR | 0.20 | 0.23 |
| ΔHOMA-IR | 0.49 | 0.001 |
| ΔVO2max | −0.31 | 0.098 |
- Δ is from 6 to 12 months.
Discussion
This study compared the effects of WL and AEX + WL on body composition and metabolic changes during a 6-month ad libitum follow-up after intentional weight loss in postmenopausal women. Although the hypothesis was that the AEX + WL group would have less weight regain and better metabolic profiles, findings indicate that weight regain and metabolic changes at follow-up were not different between groups. Overall weight regain was associated with a worsening of glucose metabolism. Furthermore, greater baseline M by the glucose clamp partially predicted less weight regain, and changes in plasma leptin and HOMA-IR during the follow-up partially predicted weight regain. This suggests that initial M is partially protective against weight regain.
Multiple factors are associated with the ability to sustain weight loss over a long period of time. A recent meta-analysis of 45 trials established that weight regain 12 months after weight loss was reduced by an average of 1.5 kg when adults with obesity participated in lifestyle interventions focusing on both dietary intake and physical activity, compared with a control/minimal care intervention (31). In the current study, weight regain was not different between groups, independent of initial assignment. Groups were equally compliant with attending the weight maintenance classes. Yet our results, contrary to our hypothesis, indicate that initial participation in AEX + WL was not better than WL because both groups had better CVD and diabetes risk factor profiles at 12 months, and there was no difference between groups. This may be because of our findings that VO2max declined during the follow-up in the AEX + WL group as a whole, reverting to initial fitness values, and because the women attended less than 30% of the available exercise sessions during follow-up. Although fitness declined in the AEX + WL group by 12 months, better compliance in continuing to exercise from 6 to 12 months was associated with less weight regain. It would have been useful to know exercise intensity adherence and to measure free-living physical activity at the 12-month visit to determine whether energy expenditure differed between the groups. Weekday total activity decreased 23% after 6 months for WL but not for AEX + WL, indicating that both structured and nonstructured activity is impacted if women undergo weight loss without participating in physical activity (32).
Despite an overall similar weight regain of ∼2 kg in both groups at 12 months, total body fat, visceral fat, subcutaneous abdominal fat, and midthigh fat remained lower than at baseline. The maintenance of loss of abdominal and midthigh subcutaneous fat despite minimal weight regain suggests that the weight regain occurred in other depots or is too small to contribute to the change in body weight. In the current study, both groups had improvements in triglyceride and HDL-C levels after the initial WL and AEX + WL, which were maintained at 12 months, suggesting some residual effect of the initial treatment. Systolic blood pressure declined after initial weight loss and did not change during the follow-up. Perhaps this is caused by the fact that these postmenopausal women had, on average, normal blood pressure levels and by the fact that many were medicated throughout the study. Thus, the benefits of initial WL or AEX + WL on body composition, triglycerides, HDL-C, and blood pressure were maintained despite weight regain. This should be considered in light of our findings that the moderate increase in VO2max might have contributed to the lack of difference in body composition and M values between the groups at 6 months and might have influenced the similar change between 6 to 12 months in AEX + WL and WL.
In the Study of the Effects of Diet on Metabolism and Nutrition (STEDMAN) project, fasting insulin and HOMA-IR declined after 6 months of weight loss and showed a sustained reduction at 12 months despite weight regain of between 2 and 17.5 lb in the majority of subjects (n = 19), with only two subjects remaining weight stable (< 1-lb gain or loss) and six continuing to lose weight (18). Our results confirm these findings for WL and add that AEX + WL also resulted in a sustained improvement in glucose metabolism, including reductions in fasting glucose and insulin, as well as in insulin AUC levels from the oral glucose tolerance test (OGTT), each of which remained lower at 12 months than at baseline despite weight regain. Similarly, the decrease in HOMA-IR with WL and AEX + WL persisted at 12 months, suggesting a sustained reduction in insulin resistance. Thus, some metabolic improvements are maintained despite some regain of body weight.
Weight cycling (5-lb weight change) was associated with incident diabetes, higher fasting glucose, greater HOMA-IR measures, and higher systolic blood pressure in adults followed for 2 years in the Diabetes Prevention Program (33). In the Look AHEAD (Action for Health in Diabetes) trial of adults aged 45 to 76 years, the initial weight loss and weight loss during the first year were predictive of greater improvements in glycosylated hemoglobin, HDL-C, and systolic blood pressure at the 4-year follow-up (34). In a study of postmenopausal women, total cholesterol, LDL-C, insulin, and HOMA-IR were worse at 12 months than at baseline in women who regained ≥ 2 kg of weight by 12 months in comparison with women who maintained or lost weight at 12 months (20). Our study supports this because the data indicate a relationship between weight regain and the change in metabolic profiles from 6 to 12 months. Although the amount of weight regain in our study was on average ∼50% less than the average 4-kg regain reported by Beavers et al. (20), in whose study there was a worsening of metabolic profiles, their follow-up was twice as long (e.g., 12 months) and was associated with greater weight regain. This suggests that the magnitude of weight regain and duration of follow-up are important predictors of which metabolic improvements are maintained.
An examination of predictors of weight regain implicates the importance of M in weight regain. In the Quebec Family Study, reduced OGTT glucose120min levels were associated with weight gain over a 6-year follow-up, which was speculated to be caused by an increase in hunger (15). In addition, subjects with obesity with the lowest glucose levels during the OGTT had the greatest weight regain after a weight loss program by drug therapy plus energy restriction or weight loss by energy restriction alone (15). In a small sample (n = 10) of women with moderate obesity who underwent a 3-month weight loss program, weight regain at 12 and 18 months correlated with the change in insulin sensitivity by the glucose clamp from baseline to the weight maintenance phase (16). In our study, initial fasting glucose, glucose120min levels, and glucose AUC were not associated with weight regain; however, women with the highest M measured during the glucose clamp at baseline had the smallest weight regain at 12 months. A review of literature concludes that changes in leptin, taken alone, are not sufficient to predict weight regain following weight loss (11); however, Rosenbaum et al. have shown that leptin administration in humans reversed the decline in energy expenditure of a weight-reduced state (35) and increased the work efficiency of skeletal muscle (36), suggesting a role of leptin in weight regain. In our model, both changes in leptin and HOMA-IR from 6 to 12 months were independently associated with weight regain, suggesting that some combination of the two creates a phenotype at risk for weight regain.
It should be noted that a greater exercise stimulus could have resulted in a difference in weight loss and greater change in M between the two groups in the initial 6 months (21). However, our finding that the AEX + WL and WL groups had similar changes in body weight allows, in fact, a better comparison for examining weight regain because both groups started the comparison after the same relative weight loss. Additionally, our results should be evaluated in light of the 34% dropout rate, which may reflect sample bias (i.e., different motivations/goals of those who completed the 6- vs. 12-month follow-up) and limited the sample size available at the 12-month follow-up period.
In summary, these results show that weight loss, whether accompanied by exercise training or not, is associated with comparable weight loss and metabolic improvements that are sustained during ensuing modest weight regain over the subsequent 6 months. Future research could focus on cellular mechanisms for weight regain in postmenopausal women.
Acknowledgments
Our appreciation is extended to the women who participated, the clinical team, and the research assistants.





