Irisin levels before and after physical activity among school-age children with different BMI: A direct relation with leptin
Funding agencies: The Fundación Miguel Alemán A.C. and Fondo Nestlé para la Nutrición supported this study.
Disclosure: The authors declare no conflict of interest.
Author contributions: BPG and BAP conceived and carried out the experiments. FVO, EPO, TS, MAM were responsible for study design and data collection. SRH carried out the data analysis. NM carried out the experiments. All authors were involved in writing the paper and approved the submitted and published versions.
Abstract
Objective
Irisin is a novel myokine that seems to mediate the beneficial effects of exercise. Levels of circulating irisin before and after an 8-month physical activity program (PAP) in school-age children were evaluated.
Methods
Irisin and leptin were measured at baseline and at follow-up among 85 children with different BMI.
Results
Of the 85 children (mean age 8.9; 47% female), 25 children had normal weight, 23 were overweight, and 37 had obesity. We observed no significant difference in irisin serum levels between boys and girls. Irisin was positively associated with BMI before and after the PAP (rbefore = 0.42; rafter = 0.37, P < 0.001), with the highest levels in children with obesity. There was a slight decrease of circulating irisin after PAP, but this decrease was not of statistical significance. We observed a high and positive association between irisin and leptin levels before and after the PAP (rbefore = 0.78; rafter = 0.82, P < 0.001). Moreover, changes in leptin correlated with changes in irisin (r = 0.72, P < 0.001).
Conclusions
Circulating irisin is positively linked to BMI and leptin in school-age children, supporting the notion that that irisin is produced by adipose tissue. As in previous reports, this study failed to observe changes in irisin levels after exercise, likely because higher irisin levels are produced only during exercise.
Introduction
Childhood obesity prevalence has increased greatly during the past three decades, especially in low- to middle-income countries (1). In Mexico, 34.4% of children are overweight or obese (2). Increased adiposity in childhood has become a major challenge, as many overweight children will become adults with obesity, increasing the risk of several co-morbidities (3, 4). While exercise is part of the standard treatment for obesity, benefits other than increased energy expenditure have been reported. Irisin, first described as a myokine produced during exercise in the mouse model, seems to have a beneficial effect on white adipose tissue. Irisin was found to increase the expression of brown adipose tissue markers raising energy expenditure, leading to a healthier metabolic phenotype in mice (5). However, reports on changes in irisin, in response to exercise in humans, have been inconsistent. Some studies report significant increases in FDNC5 (the gene encoding for irisin) expression and circulating levels of irisin (6, 7); while others have failed to observe changes in circulating levels of irisin or FNDC5 mRNA expression in muscle tissue (6, 8-10). Other factors that seem to influence irisin levels are age, BMI, gender, and level of physical activity (6, 8, 11-14). These studies were performed among adults; little is known about the relationship between irisin and exercise in children. The aim of this study was to evaluate circulating levels of irisin before and after implementation of a physical activity program (PAP) among school-age children.
Methods
Subjects
A total of 1888 children aged between 6 and 11 years from middle- to low-income families, attending five urban elementary schools in Toluca (central Mexico), were invited to participate in a PAP for school-age children. For this study, we selected a sample of 85 healthy children (female = 45 and male = 40), aged between 8 and 10 years. Children were selected by their age and weight, in order to have three groups defined by BMI (obese, overweight, and normal weight). The study was performed pursuant to the latest version of the Declaration of Helsinki and was approved by the Internal Review Board of the School of Medicine of the Universidad Nacional Autónoma de México (#043-2012). All parents or legal guardians and children gave written informed consent.
Physical activity program
The program was designed to be simple, low cost, and achievable in low-income communities with the support of physical activity teachers, who supervised all sessions. The PAP consisted of a 5-minute warm-up, followed by 25 minutes of middle-intensity exercise (< 70% Fcmax), 5 days a week for 8 months. Exercise included group walking and running (sprints) and required no special equipment. Parents were instructed to maintain the childreńs usual dietary habits during the study.
Anthropometric and biochemistry analysis
Body weight (kg) and height (cm) were assessed before and after the PAP. BMI was calculated as weight/height squared (kg m−2) and z-scores were derived using the World Health Organization references. Blood pressure was measured three times, placing an automatic inflatable cuff on the nondominant arm in resting position. Fasting blood samples were collected a week before beginning the PAP and after its conclusion. All samples were stored at −80 °C until analysis. Glucose, triglyceride, total cholesterol, LDL-cholesterol, and HDL-cholesterol serum levels were determined by an automated system (Adaltis Spinreact, Spin React, Clinical Diagnostics, Paris, France). Both leptin and irisin serum levels were measured by commercial ELISA kits, following manufacturer instructions (Human Leptin Quantikine, R&D Systems and CUSABIO BIOTECH, respectively). The sensitivity of the irisin assay is 0.78 ng/mL and intra-assay CV is <8%.
Statistical analyses
Normal distribution was assessed by corrected Kolmogorov–Smirnov test. The t test for unpaired groups was used to compare the differences between males and females. Differences between the groups were assessed with one-way ANOVA, followed by Fisher's protected least-square difference test to determine the significance. The differences were considered significant at P < 0.05. The association between variables was evaluated by bivariate correlation (Pearson's) and analysis of covariance, adjusting for BMI, age and gender.
Results
Table 1 shows the baseline anthropometric and biochemical values. No significant differences were observed in glucose or lipid metabolism parameters between males and females or among the groups.
| Normal weight (n = 25) | Overweight (n = 23) | Obese (n = 37) | |
|---|---|---|---|
| Age (years) | 9.0 ± 0.86 | 9.5 ± 0.74 | 8.8 ± 0.86 |
| Female (%) | 60 | 13.3 | 26.7 |
| BMI z-scorea | −0.25 ± 0.67 | 1.27 ± 0.28 | 2.64 ± 0.43 |
| Systolic blood pressure (mm Hg) | 106.0 ± 13.7 | 107.0 ± 10.4 | 103.0 ± 11.7 |
| Diastolic blood pressure (mm Hg) | 62 ± 9.1 | 67.0 ± 10.0 | 63.0 ± 13.1 |
| Glucose (mg/dL) | 95.9 ± 11.8 | 92.2 ± 10.7 | 96.6 ± 10.3 |
| Triglycerides (mg/dL) | 95.5 ± 43.0 | 92.8 ± 60.6 | 114.5 ± 74.8 |
| Total cholesterol (mg/dL) | 142.0 ± 40.4 | 135.0 ± 29.4 | 141.0 ± 25.4 |
| LDL-cholesterol (mg/dL) | 65.0 ± 19.0 | 63.0 ± 15.0 | 70.0 ± 15.7 |
| HDL-cholesterol (mg/dL) | 46.0 ± 11.0 | 45.0 ± 14.3 | 41.0 ± 10.3 |
| Leptin (pg/mL)a | 593.2 ± 132.2 | 1736.6 ± 409.0 | 2926.8 ± 369.8 |
| Irisin (ng/mL)a | 99.7 ± 25.3 | 139.5 ± 22.7 | 251.47 ± 23.3 |
- Mean values ± SD.
- a ANOVA P ≤ 0.001.
BMI z-score significantly decreased from 1.27 to 0.86 (P < 0.0001) in the overweight group and from 2.64 to 2.44 (P < 0.0001) in the obese group, while it remained unchanged in the normal weight group.
Leptin was significantly and positively associated with BMI z-score (rbefore = 0.80, P < 0.0001; rafter = 0.80, P < 0.0001). Leptin decreased only in children with obesity after the PAP (3090.86 ± 372 vs. 1902.69 ± 259, P < 0.01).
Irisin levels increased along with BMI, with the highest level observed in children with obesity (P < 0.001). Moreover, we observed a significant positive correlation between irisin and BMI before and after the PAP (rbefore = 0.42; rafter = 0.37, P < 0.001) (Figure 1A).
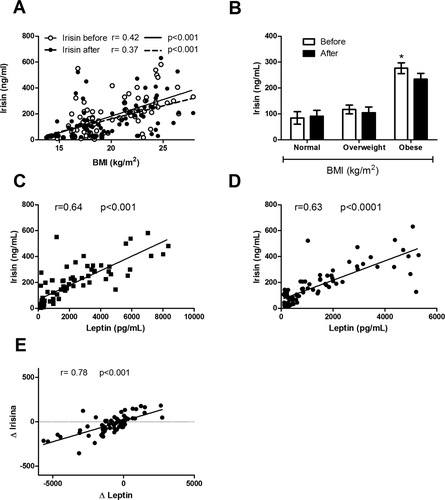
Correlations between circulating levels of irisin with BMI and leptin. (A) Positive correlation between irisin and BMI before and after the physical activity program (PAP); (B) circulating levels of irisin before and after the PAP among school-age children in the different BMI groups; (C) positive correlation between irisin and leptin concentration before the PAP; (D) positive correlation between irisin and leptin concentration after the PAP; and (E) positive correlation between Δ irisin and Δ leptin.
Mean serum irisin levels also decreased after the PAP from 176.55 ± 15.68 to 153.34 ± 15.57 ng/ml in the entire sample, although the difference did not reach statistical significance (P = 0.071). When stratifying by BMI, the tendency was observed only in the obese group, decreasing from 251.47 ± 23.30 to 209.07 ± 25.14 (P = 0.079) (Figure 1B).
Interestingly, we observed a significant positive correlation between irisin and leptin before and after the activity intervention (rbefore = 0.78; rafter = 0.81; P < 0.001) (Figures 1C and D, respectively). This association persisted after adjusting for BMI, age, or gender (ßbefore = 53.75, 95% CI 42.95-64.55; ßafter = 68.72, 95% CI 53.48-83.96). Furthermore, total decrease in leptin (Δleptin) also showed a strong association with total decrease in irisin (Δirisin) (r = 0.72, P < 0.001). Again, this association persisted after adjusting for other variables (ß = 52.52, 95% CI 43.41-61.64) (Figure 1E).
Discussion
School-based PAPs for children are being developed in Mexico and other countries as a means of overcoming obesity among children (2). As exercise has proved to have beneficial effects on weight control and metabolic improvement, in the last few years, research studies have focused on the connection between skeletal muscle and adipose tissue. From these studies, irisin emerged as a possible link between these two tissues (5), although, evidence in humans is still controversial. In this study, circulating irisin levels in school-age children with different BMI were assessed before and after a PAP. We observed a positive correlation of circulating irisin to BMI, with the highest levels among children with obesity, as per previous studies involving adults (6, 15); and a tendency toward a decrease of irisin levels in children with obesity after the PAP, related to a decrease in body weight. The changes in BMI observed suggest that the program, although simple, was effective; and the greatest improvement was seen among children in the overweight and obese BMI categories.
Previous studies have shown that irisin levels decreased as body weight decreased in adults following diet and bariatric surgery (6, 16). Similarly, we observed a tendency toward a decrease in circulating irisin with decreasing BMI. It is possible that larger studies are needed in school-age children to definitely show this association.
Although FNCD5 is most expressed in skeletal muscle, it is also expressed in subcutaneous adipose tissue, and this expression is associated with circulating levels of irisin (15). In our study, a strong relationship between leptin and irisin levels was observed, which also suggests a relationship between adipose tissue and circulating irisin. However, since fat mass was not directly assessed, that relationship needs to be further examined.
Increases in irisin production after chronic exercise in humans have been controversial. Several studies, including ours, failed to show an increase in circulating irisin levels after chronic exercise (6, 8). However, it has been suggested that the timeframe over which irisin is increased after exercise is brief, thus it is possible that delayed sampling has an impact on the ability to detect rises in serum levels (10, 11, 17, 18). This recent evidence suggests that the acute rise in exercise-induced irisin is most likely accounted for skeletal muscle release (11), and basal irisin levels could be accounted for adipose tissue production.
While preparing this manuscript, a study by Bluher and colleagues was published (19). This study, which involved only overweight/obese children at a mean age of 12 years old, showed an increase in circulating levels of irisin after 1 year of supervised exercise. No correlation of irisin with any biomarker of body composition or inflammation was observed. The exercise program was more intense and included the use of gym facilities and supervision by certified trainers. Differences in the intensity of the physical program and the average age of children in both studies could explain the different findings. We did not observe differences in irisin secretion between boys and girls in accordance with Bluher et al., study.
In summary, in this study circulating irisin was positively linked to indirect adiposity measurements among school-age children. The finding, along with others, leads us to believe that most basal irisin is produced by adipose tissue and that skeletal muscle irisin production exceeds this limit only during exercise. Further studies including the identification of the receptor and signaling pathway of irisin are needed for a better understanding of irisin-adipose tissue relations and its function in humans.
Acknowledgments
We are grateful to all the children who participated in this study, as well as to their parents.





