A transition programme to enhance ICU new graduate nurses' professional identity and intention to remain employed: A pre- and postevaluation
Fen Hu and Xin-Bo Ding contributed equally and share the first authorship.
Abstract
Aims
To investigate the effect of a transition programme including cognitive-behaviour-based preceptorship intervention on ICU new graduate nurses' (NGNs)' professional identity and their intention to remain employed.
Design
One-arm pre- and post-test design followed the TREND Statement.
Methods
NGNs' professional identity and intention to remain employed were measured at baseline (T1), postintervention (1 month, T2) and 6-month follow-up (T3).
Results
Fifty-three NGNs completed the programme, and their professional identity score significantly increased postintervention [from 111.5 (SD = 16.72) at T1 to 114.2 (SD = 9.12) at T2, p < 0.05], but decreased at T3 [105.8 (SD = 9.44) compared with T1 and T2, p < 0.05]. There was no significant difference in ICU NGNs' intention of remain employed outcomes at three time points (p > 0.05). The transition programme was effective to improve ICU NGNs' professional identity immediately after the intervention, but the increment did not maintain at the 6-month follow-up.
1 INTRODUCTION
Within the global ageing population and an ageing nursing workforce, significant nursing shortages are affecting healthcare delivery and people's health (Halter et al., 2017). Keeping nurses employed is considered a key factor for high-quality health care (Jiang et al., 2017). Lower professional identity and higher turnover intention were reported as the leading reasons for nursing shortage (Slattery et al., 2016).
In the early stages of career development, inappropriate occupational orientation and different adaptabilities to clinical work among new graduate nurses (NGNs) may affect their professional identity and turnover intention (Kovner et al., 2007). A study reveal that more than 70% of NGNs had turnover intention after only 1 year of work (Zhang et al., 2017). Interventions addressing nurses' professional identity and turnover intention should be started early in their careers.
Professional identity involves an individual's understanding and perceptions of professional practice, personal development and professional value (Mousazadeh et al., 2019). Nurses' professional identity and intention to stay can directly predict their retention behaviour (Brown et al., 2013; Steinmetz et al., 2014). Research has reported that negative professional identity was significantly associated with higher turnover intention (Zhang et al., 2018). Improving professional identity could increase nurses' intention to remain employed, and enhance their satisfaction and work engagement (Liu et al., 2018, 2020).
The level of professional identity and intention to remain employed among nurses working in intensive care units (ICUs) are often lower than those of nurses in other departments due to the heavy workload, high tension and long-term facing with critical patients (Brown et al., 2013; Kovner et al., 2007). Increased exposure to deaths in ICU generates grief among ICU staff, leading to high-level psychological stress, a low level of professional identity and ultimately a high rate of turnover (Kapoor et al., 2018; Shorter & Stayt, 2010). The outbreak of the COVID-19 pandemic negatively impact ICU nurses' professional identification and decreased their intention to remain employed (Hu et al., 2021). Given the context of global ageing, shortage of nursing workforce, and the outbreak of the COVID-19 pandemic, how to increase ICU NGNs' professional identity and intention to remain employed is a challenge for critical care nursing workforce research.
Among interventions targeted at enhancing nurses' professional identity and intention to remain employed, cognitive-behavioural interventions and preceptorship interventions are widely used and effective (Brook et al., 2019), which may also benefit ICU NGNs. Cognitive-behavioural intervention is a systematic process that enables nurses to develop their thinking and skills to cope with problems encountered in their professional work through cognitive restructuring (Batterbee, 2020). Preceptorship is typically described as a formal one-to-one relationship between a nursing student or a newly qualified nurse, and a registered nurse that extends over a pre-determined length of time (Bochenek et al., 2016). Therefore, this study aimed at exploring the effect of a transition programme consisting of cognitive behaviour-based preceptorship interventions on enhancing ICU NGNs' professional identity and intention to remain employed.
2 METHODS
2.1 Study design
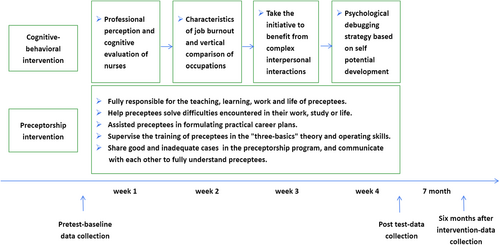
A quasi-experimental with one-arm pre- and postevaluation and a 6-month follow-up design was conducted following the TREND Statement to guide this study (see Appendix S1). Since all the participated nurses were working in the same unit, a randomized controlled design was not used in this study. This study compared professional identity and intention to remain employed among ICU NGNs before (baseline, Time 1), and after (1-month, Time 2) a tailored transition programme (Figure 1). The maintenance of the outcomes 6 months after completion (7-month, Time 3) of the intervention was also examined.
2.2 Ethical considerations
The study was approved by the ethics committee of Wuhan University School of Medicine. Participants were also introduced to the study and informed they could drop out anytime without any disadvantages. Informed consent was obtained from the participants after a detailed explanation of the research purpose, the process of data collection and the right to decline to participate without any consequences and were assured of the confidentiality of the study.
2.3 Settings and participants
This study was conducted in an ICU at an academically affiliated tertiary hospital in Wuhan, Hubei, China. Complex care and life support were provided in this ICU, that is extracorporeal membrane oxygenation (ECMO) and continuous renal replacement therapy (CRRT). NGNs were eligible to participate in the study if they had recently completed the undergraduate or associated nursing programme, passed the national nursing registration examination and did not have any previous clinical nursing experience.
2.4 The transition programme
The transition programme consisted of a cognitive behaviour-based preceptorship intervention. In this phase, the participated NGNs underwent four 90-minute sessions of training with one session per week. In the preceptorship intervention phase, the NGNs received comprehensive guidance on teaching, learning, work, and lifework balance from senior nursing preceptors.
2.4.1 Cognitive-behaviour intervention programme
This cognitive-behaviour intervention programme focussed on nurses' professional identity and professional cognitive assessment. This intervention was designed based on literature review, experts' advice and brainstorming of the research group (Folkman et al., 1987). The contents included a detailed manual, and lectures reviewed by a panel of experts in nursing administration, psychology, healthcare management and education. The cognitive-behaviour intervention programme was simplified to four sessions to overcome the lack of spare time for clinical nurses according to a previous study (Mackenzie et al., 2006). These four-session cognitive-behavioural training consisted of (a) professional perception and cognitive evaluation of nurses (i.e. history of ICU nursing and the value of nursing in ICU), (b) characteristics of job burnout and vertical comparison of occupations (i.e. signs of burnout), (c) taking the initiative to benefit from complex interpersonal interactions (i.e. communication and dealing with conflict) and (d) psychological debugging strategy based on self-potential development (i.e. mediation and deep breath). The training was delivered through in-person seminars including case analysis, experience sharing, group discussion and psychological counselling (one session per week). Each session included 60 minutes of lectures and 30 minutes of discussion. The training was conducted by a group of experts in nursing psychology in four individual sessions within one month.
2.4.2 Preceptorship intervention programme
Experienced nurses working in the same ICU were recruited as preceptors if they had: (a) more than 3 years of working experience in ICU and with excellent annual evaluations; (b) ICU specialist district nurse qualification; (c) bachelor's degree or above; (d) professional title as senior nurse or above; (e) subjective qualities, including an ability to demonstrate responsibility, cooperation, and recognition and inspiration to others. All eligible senior nurses working in this ICU were encouraged to submit a preceptor application and only those nurses were recruited as preceptors for ICU NGNs if their applications were approved by more than two-thirds of all the nurses in this ICU. A total of 70 applications were received and 63 were approved.
These 63 preceptors were trained to take responsibilities of preceptors as follows: (a) fully responsible for teaching, learning, work and life of NGNs; (b) face-to-face communication with NGNs at least once a week to help them solve difficulties encountered, and to listen to NGNs' notions of preceptors' performance; (c) assisting NGNs in formulating practical career plans and supervising their implementation; (d) supervising the training of NGNs in the ‘three-basics (basic theory, basic knowledge, basic skills)’; and (e) attending group conversation of preceptors to share and explore good or inadequate cases in the preceptorship programme. Continuing education hours and performance-related bonuses were awarded to each preceptor.
Each of the preceptors and ICU NGNs gave a 5-minute competitive speech. Then, preceptors and NGNs wrote down their ideal paring candidates and whether they accepted adjustment in case of unsatisfactory pairing. Head nurses matched preceptors and NGNs with their ideal paring candidates and their acceptance of adjustment to paring candidates. Each of the NGNs was assigned a full-time preceptor, and the preceptorship lasted from the beginning of the transition programme to 6 months.
2.5 Measurements
Sociodemographic characteristics of the NGNs were collected at baseline. These variables were age, gender, educational level, primary motivation for choosing a job, average monthly night shifts and future career planning. Outcome measurements, including professional identity and intention to remain employed, were collected at baseline before the initiation of the transition programme (Time 1), immediately after the cognitive-behaviour intervention (Time 2), and 6 months after the completion of the transition programme (Time 3).
2.5.1 Professional identity
Professional identity was assessed using the Chinese version of the Professional Identity Scale for Nurses (Liu et al., 2011). The scale is a 30-item self-reported questionnaire composed of five factors: professional identity evaluation (nine items), professional social skills (six items), professional social support (six items), dealing with professional frustration (six items) and professional self-reflection (three items). Participants are asked to rate how much they agree or disagree with each item on a 5-point Likert scale (1 = very inconsistent to 5 = very consistent) based on their life experience or how they might feel if these events happened to them when they did not experience these events at work. Possible points for the total scale range from 30 to 150. A higher score indicates a higher level of professional identity. The Cronbach's alpha of the scale in this study was 0.938.
2.5.2 Intention to remain employed
The Chinese version of the intention to remain employed (Tao & Wang, 2010) adapted from the Intention to Quit Scale and the Job Search Behaviour Scale (Turnley & Feldman, 1998) was used to measure ICU NGNs' intention to remain employed. This instrument comprises six items and is rated on a 5-point Likert scale (1 = absolutely impossible to 5 = very impossible) with three items reverse scorecard (item 2, 3 and 6). Possible points for the total scale range from 6 to 30. A higher score indicates a greater intention to remain employed. The Cronbach's α value of the scale in this study was 0.766.
2.6 Data analysis
Data were analysed using SPSS 25.0 statistical software. Sociodemographic data were summarized by descriptive analysis. ICU new nurses' professional identity and intention to remain employed scores acquired at a different time of the study were analysed using repeated measures ANOVA after distributional normality was tested and achieved. The per-protocol analysis was applied since the six participants signed the inform consent but did not respond to any intervention component. Two-tailed tests of significance were performed and a p-value of <0.05 was considered significant.
3 RESULTS
3.1 Recruitment and retention
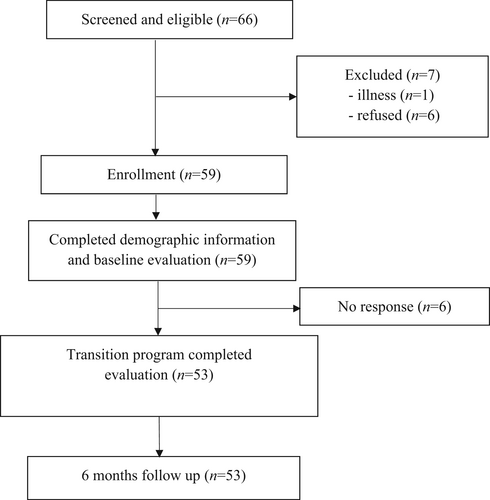
A total of 66 NGNs working in the ICU were invited to participate in the study. Informed consent was obtained from 59 of these NGNs, seven did not participate due to illness or refusal. Six participants dropped out during the cognitive-behavioural intervention. The other 53 NGNs completed the cognitive behaviour intervention, postevaluation at Time 2 and Time 3 (Figure 2). The retention rate was 89.8% for Time 2 and Time 3 evaluations.
3.2 ICU NGNs' sociodemographic characteristics
The sociodemographic characteristics of the 53 participants are presented in Table 1. The mean age of the participants was 22.11 years (SD = 0.88, range = 21–24). Men constituted 22.6% of the total participants. The majority (66%) of them had a nursing education higher than an associated degree. More than 86% of the participants' first volunteer major for college entrance examination was nursing and the majority (62.3%) chose a nursing job for occupational stability. Average monthly night shifts were 6.89 (SD = 1.42, range = 3–10), and the average night shift per month of most participants were between 5 and 9 (92.5%), the night shifts were not significantly different between participants and non-participants in this ICU. 62.3% of the participants' career plans were to become a critical care nursing specialist.
| Variable | n (%) |
|---|---|
| Age (years) | |
| 21 | 13 (24.5) |
| 22 | 26 (49.1) |
| 23 | 9 (17.0) |
| 24 | 5 (9.4) |
| Gender | |
| Male | 12 (22.6) |
| Female | 41 (77.4) |
| Educational level | |
| Associated degree | 18 (34.0) |
| Bachelor's degree | 35 (66.0) |
| First volunteer major for college entrance examination | |
| Clinical medicine | 1 (1.9) |
| Nursing | 46 (86.8) |
| Other | 6 (11.3) |
| Primary motivation for choosing a nursing job | |
| Occupational stability | 33 (62.3) |
| Salary guarantee | 14 (26.4) |
| Professional value | 3 (5.7) |
| Helpful to family health | 3 (5.7) |
| Average monthly night shifts | |
| 0–4 | 3 (5.7) |
| 5–9 | 49 (92.5) |
| ≥10 | 1 (1.9) |
| Career planning | |
| Nurse educator | 6 (11.3) |
| Nursing specialist (ICU) | 33 (62.3) |
| Nurse manager | 14 (26.4) |
3.3 Preceptors' sociodemographic characteristics
The total number of preceptors was 59 since 59 NGNs participated in the study. The mean age of the preceptors was 29.75 years (SD = 2.99, range = 24–35), and the majorly were aged from 26 to 30. The preceptors included more females (76.2%) than males. Most (95.2%) preceptors had a bachelor's degree in nursing, while the other 4.8% had a master's degree. The professional titles of preceptors were senior nurse (82.5%) and nurse in charge (17.5%). The average working experience of the preceptors in the nursing or critical care environment was 7.21 years (SD = 2.60, range = 4–12), and most (50.8%) of them worked 6–10 years in nursing or ICUs.
3.4 NGNs' professional identity outcomes
Table 2 shows the comparisons of professional identity scores among ICU NGNs measured at three time points, as well as the effect sizes for the total scores and scores in each factor of professional identity. The total scores of ICU new nurses' professional identity (F = 6.592, p = 0.004) were significantly different at three time points with a large effect size (Cohen's D = 1.413), so as the factors of professional identity evaluation (F = 3.956, p = 0.026), professional social support (F = 4.492, p = 0.017), dealing with professional frustration (F = 10.872, p < 0.001) and professional self-reflection (F = 9.855, p < 0.001), but no significant changes were observed in professional social skill score (F = 1.986, p = 0.142).
| Score | Time 1 | Time 2 | Time 3 | Wilks' Lamda | F a (p) | p | Effect size (Cohen's d) |
|---|---|---|---|---|---|---|---|
| Professional identity evaluation | 32.3 (5.84) | 32.7 (3.56)† | 30.4 (3.92) ‡# | 0.808 | 3.956 | 0.026 | 0.975 |
| Professional social skill | 20.5 (3.14) | 20.7 (3.96) | 19.5 (2.90) | 0.905 | 1.986 | 0.142 | 0.648 |
| Professional social support | 23.6 (3.81) | 24.2 (2.57)† | 22.5 (2.48) # | 0.806 | 4.492 | 0.017 | 0.981 |
| Dealing with professional frustration | 23.0 (3.30) | 24.3 (2.22)† | 22.0 (2.09) ‡# | 0.604 | 10.872 | <0.001 | 1.619 |
| Professional self-reflection | 11.8 (1.67) | 12.5 (1.30)† | 11.4 (1.26) # | 0.673 | 9.855 | <0.001 | 1.394 |
| Total score of professional identity | 111.5 (16.72) | 114.2 (9.12)† | 105.8 (9.44) ‡# | 0.667 | 6.592 | 0.004 | 1.413 |
- Note: Values are mean (SD).
- †Significant difference (p < 0.05) between Time 1 and Time 2, ‡Significant difference (p < 0.05) between Time 1 and Time 3, #Significant difference (p < 0.05) between Time 2 and Time 3.
- a One-way ANOVA for repeated measures was used to calculate p-values (⁎p < 0.05, ⁎⁎p < 0.01, ⁎⁎⁎p < 0.001).
Pairwise comparisons revealed significant differences between time points for a total score of ICU NGNs' professional identity, with an increase of 2.7 from Time 1 to Time 2 (p < 0.05), a decrease of 8.4 from Time 2 to Time 3 (p < 0.05) and a decrease of 5.7 from Time 1 to Time 3 (p < 0.05). ICU NGNs' scores on professional identity evaluation, professional social support, dealing with professional frustration and professional self-reflection at Time 2 were significantly higher than those at both Time 1 (p < 0.05) and Time 3 (p < 0.05). In addition, their scores on professional identity evaluation and dealing with professional frustration at Time 1 were significantly higher than that at Time 3 (p < 0.05).
3.5 NGNs' intention to remain employed outcomes
Table 3 presents the scores of ICU NGNs' intention to remain employed, at different times during the study process. The mean score of ICU NGNs' intention to remain employed was 22.8 (SD = 3.29), 22.12 (SD = 3.98) and 22.2 (SD = 3.14) at Time 1, Time 2 and Time 3, respectively. One-way ANOVA for repeated measures showed no significant differences among the three time points in the total score of ICU NGNs' intention to remain employed (F = 0.398, p = 0.674) with a small effect size (Cohen's D = 0.247).
| Score | Time 1 | Time 2 | Time 3 | Wilks' Lamda | F a | p | Effect size (Cohen's d) |
|---|---|---|---|---|---|---|---|
| Total score of intention of remain employed | 22.8 (3.29) | 22.2 (3.98) | 22.2 (3.14) | 0.985 | 0.398 | 0.674 | 0.247 |
- Note: Values are mean (SD).
- a One-way ANOVA for repeated measures was used to calculate p-value.
4 DISCUSSION
This study assessed the effect of a transition programme consisting of cognitive behaviour-based preceptorship interventions on ICU NGNs' professional identity and intention to remain employed in ICU by using a one-arm pre- and post-test design. ICU NGRNs reported significant improvements in professional identity immediately after the transition programme. The intervention effect of improvements in professional identity faded at 6 months of follow-up.
The participants reported improvement in professional identity evaluation, an important measure of a nurse's professional identity, immediately after the transition programme. In the cognitive-behaviour intervention programme, ICU NGRNs had a chance to link their work experiences and perceived happiness in clinical work since the cognitive-behavioural intervention emphasizes proper professional perception, guiding NGNs to recognize the value of nursing and evaluate nursing positively. In the cognitive-behaviour intervention programme, ICU new nurses rethought their working experiences and apperceive happiness in clinical work. In addition, the preceptorship intervention programme provides role models to ICU new nurses (Bochenek et al., 2016). Preceptors with excellent personal qualities, as the closest person to NGNs in the ICU, directly affect their cognition and evaluation of nursing as a profession. The one-to-one NGN and preceptor interactions also facilitated a positive professional identity among ICU NGNs.
ICU new nurses had significant improvement in professional social support after the intervention. Nurses are eager to be recognized by patients and to be respected, affirmed and supported by colleagues, doctors, nursing managers, family and friends (Rossiter & Sochos, 2018; Woodhead et al., 2016). Several aspects could explain the improvement in professional social support. In the cognitive-behavioural intervention programme, ICU new nurses were encouraged to notice that it is an important opportunity for the development of nursing science and take initiative to benefit from complex interpersonal interaction with patients, colleagues, and families. In the preceptorship intervention programme, vigorous support was given by preceptors to ICU NGNs' overall life, work and learning. In group activities of the programme, ICU NGNs were linked more closely with colleagues and perceived more support.
The results of this study showed an increase in the domain of dealing with professional frustration and professional self-reflection. In the cognitive-behavioural intervention, the inevitability and risk of professional burnout were introduced to the ICU NGNs, and the ICU NGNs were encouraged to develop their potential and benefit from nursing. The ICU NGNs grow from a difficult position, with confidence and the ability to cope with difficulties. In the transition programme, ICU new nurses constantly reflect using the techniques provided in the in-person seminar during the cognitive-behavioural intervention phase, that is mediation. Moreover, the preceptorship intervention programme requires preceptors to help ICU NGNs deal with the frustrations they met, whatever. ICU NGNs can learn effective methods to deal with problems with help of others (Lafrance, 2018). Owing to preceptors' contribution to NGNs' profession, NGNs sense enthusiasm for the profession which results in reasonable career planning and proper reflection on their profession (Edwards & Connett, 2018).
The results of this intervention programme show no significant improvement in professional social skills. ICU NGNs may not receive enough training regarding professional social skills in this transition programme. The cognitive-behavioural intervention programme focussed on the understanding and perception of nursing but pay less attention to the training of professional social skills. Social courses greatly affected the social skills of nurses (Mousazadeh et al., 2019). On the contrary, preceptors may have limited professional social skills given that they were working in a closet environment in ICU. Studies have shown that ICU nurses have generally poor social skills, even preceptors (Shen et al., 2018). NGNs observed the performance of their preceptors and assimilate it into their professional role as independent care providers, they may benefit less from professional social skills from their preceptors. Further training programmes focussed on professional social skills would be necessary for all ICU nurses, no matter their skill level.
Although the total score of ICU NGNs' professional identity had improved after intervention, it is noticeable that the score declined at the 6-month follow-up. One reason could be that a high level of patients' complexity and stress results in a decrease in professional identity since all the NGNs were supposed to independently take of patients in ICU after three months of training. A study of graduate-entry medical students' early interdisciplinary clinical experience (ICE) programme revealed a decline of professional identity after ICE (Hudson et al., 2016). On the contrary, professional identity may decline over time. A previous survey in Sweden illuminated that self-reported professional identity among baccalaureate degree nurses decreased over time after graduation in a nursing environment (Björkström et al., 2008). These findings might reflect the effects of time and clinical environment on novice medical staff. Qualitative interviews may yield a deeper understanding of the cognitive-behaviour intervention from the NGNs' perspectives. However, qualitative data were not collected in this study, which is one of the limitations. The effect size of the total score comparison was 1.413 (Cohen's d), indicating that the current sample size was large enough to detect the changes in professional identity at different time pinots (Cohen, 1992). Therefore, the results that NGNs' professional identity first increased after the intervention and then decreased after 6 months in the current study illustrated the effect of this intervention programme and the necessity of long-term interventions to assist NGNs in transit to experienced nurses.
There was no significant difference in ICU NGNs' intention of remain employed outcomes at three time points (p > 0.05). A possible reason for this could be that these ICU NGRNs were newly employed and were enthusiastic about their first job. They had a strong intention to continue their jobs and did not consider leaving them before the intervention. Previous studies reported that the mean score of intention to remain employed among nurses was 19.82 (SD = 4.27) (Xiao et al., 2016) and 20.39 (SD = 5.30) (He et al., 2018). However, the score of intention to remain employed among the NGNs in our study measured at pre-intervention, post-intervention, and 6 months of follow-up was 22.8 (SD = 3.29), 22.2 (SD = 3.98), 22.2 (SD = 3.14), respectively. An intervention aimed at improving the relatively high level of intention to remain employed may not yield a detectable interventional effect.
As an investigation in New Zealand, nurses were strongly affected to leave or retain by workload and work-life interference (Moloney et al., 2018). A possible reason for the declined intention to remain employed at 6-month follow-up may be due to a higher level of patients' complexity (i.e. patients with ECMO and/or CRRT) in a teaching hospital in a provincial capital and higher work pressure and strength in the ICU.
Previous studies indicated that NGNs accounted for the highest number of nurses leaving the nursing profession (Al Awaisi et al., 2015; Zhang et al., 2017). Almost 35% to 60% of nurses left their first workplace within the first year of hiring (Flinkman & Salanterä, 2015; Van Camp & Chappy, 2017; Zhang et al., 2017). However, none of the ICU NGNs left their positions within 18 months after the intervention. This may indicate that the intervention programme had certain effects in reducing the leaving or exiting of nurses. The results of no significant improvement prompted that a short-term intervention may not be enough for a remarkable enhancement of the intention to remain employed.
4.1 Limitations
This study has some potential limitations. First, considering the fairness and impartiality of nursing education, all ICU NGNs were encouraged to participate in the transition programme. As a result, no control group, randomization or blind method was included in this study. Second, the sample was from a single ICU of a single hospital, the generalization of findings from this study should be cautious. This study only followed up the NGRNs for six months due to recourse limitations, and the unchanged intention of the remaining employed may be an indicator of the effect of the intervention since the turnout rate was higher in the first year.
5 CONCLUSION
This study demonstrated a positive effect on ICU NGNs' professional identity through a transition programme consisting of cognitive-behaviour-based preceptorship interventions, except for professional social skills. The increase after intervention on overall professional identity failed to maintain at the 6-month follow-up, with different levels of decrease in the long-term period. The transition programme was partially effective in enhancing the professional identity of ICU NGNs immediately after the intervention, but not over the long term. Our findings revealed no significant increase in ICU NGNs' intention to remain employed. Further intervention studies should include the expectation and attitudes of ICU NGNs and preceptors. Longitudinal studies should also be conducted with a larger group of ICU NGNs to determine whether interventions have long-term effects on ICU NGRNs' professional identity and their intention to remain employed.
AUTHOR CONTRIBUTIONS
Study design. FH, XBD, JL and XF: Date collection. FH, XBD, RHZ and RC: Data analysis. FH, XBD, SYL, RHZ, RC, XPZ and JC: Draft of the manuscript. All authors involved in critical review and the final approval of the manuscript. Deidentified data will be available upon reasonable request.
- substantial contributions to conception and design, acquisition of data or analysis and interpretation of data;
- drafting the article or revising it critically for important intellectual content.
ACKNOWLEDGEMENTS
We thank all the nurses who participated in the study. We also wish to thank Doctor Thomas Lawrence Long, Professor-in-Residence at University of Connecticut School of Nursing, for his professional review of this manuscript.
FUNDING INFORMATION
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interests.
Open Research
DATA AVAILABILITY STATEMENT
Deidentified data will be available upon reasonable request.