A modified Delphi consensus on generic indicators for a low- and middle-income country’s quality nursing care measurement
Funding information
This study received a small grant from the Royal Society of Tropical Medicine and Hygiene (RSTMH) with support from National Institute for Health Research (NIHR)
Abstract
Aim
This study aimed to develop generic quality nursing care indicators for a low- and middle-income country’s quality nursing care measurement through a modified Delphi consensus.
Design
A three-round modified Delphi process guided the items' development and acceptance consensus.
Methods
Twenty-four academic and clinical nursing experts from different parts of Nigeria participated in the Delphi rounds. In the first round, 96 items (structure – 31, process – 38, and outcome – 27) were distributed to the panellists through e-mail. The same method guided round 2. In round 3, the panellists reached a consensus on the number and structure of the items.
Results
In round 1, the initial items were reduced to 75 that met the Delphi consensus. In round 2, the items were modified further and reduced to 74. In round 3, the experts reached a consensus on 70 items (structure – 28, process – 32, and outcome – 10).
1 INTRODUCTION
Quality and safe health/nursing care is a sine qua non to a healthy populace of any given race (Liu et al., 2021a, 2021b). Lack of focus on quality health care causes up to 8 million deaths in developing countries and leads to too many avoidable negative health indices like low life expectancy and high maternal and under-5 mortality rate (Adewole & Osungbade, 2016; Kruk et al., 2018; Nair et al., 2015). Quality nursing care is pivotal to quality health care as its optimal practice boosts the healthcare indices of any group of people and checks healthcare mistakes (Burhans & Alligood, 2010). As a country suffering from decades of negative health indices (United States Agency for International Development, 2020), Nigeria is in dire need of quality healthcare improvement (Okoli et al., 2016). Establishing nationwide unique and acceptable general indicators for quality nursing care establishment and measurement is a positive way to meet this need. Such indicators would constantly direct the focus of Nigerian nurses to quality service delivery as they discharge their duties. Thus, the development of distinct generic indicators for assessing the quality of nursing care in Nigeria is critical.
2 BACKGROUND
Borrowing some concepts from the World Health Organization (WHO) (2018), healthcare quality can be described as the extent to which health care rendered to one or more individuals, using the best achievable professional knowledge within a given setting, accomplishes the purpose of the care. Quality nursing care is an integral part of healthcare quality (Oldland et al., 2020) measurable through the quality nursing care indicators (QNCIs) (Gathara et al., 2010). In line with opes Silveira et al. (2015), QNCI is the state of nursing care and its supportive activities quantifiable and measurable for monitoring and evaluation of patient’s/client’s nursing care quality. To successfully use QNCIs to assess the quality of nursing care, it is critical to address specific dimensions such as resource availability for care, how care is delivered, and the outcome of care (Lindgren & Andersson, 2011). The above dimensions are understood better in a developing or low- and middle-income country by correctly identifying QNCIs peculiar to the country and shaping the indicators for ease of quality nursing care establishment and measurement.
Empirically, authorities have made efforts to establish QNCIs across the globe. American Nurses Association led the way by developing ten nursing-sensitive indicators for quality nursing care measurement in 1998 (Gallagher & Rowell, 2003 in Montalvo, 2007; Zhang et al., 2021). Recently, in China, Zhang et al. (2021) developed 38 nursing-sensitive quality indicators specifically for pernicious placenta praevia; Liu et al. (2021a, 2021b) developed a quality nursing care scale and evaluated its psychometrics from the perspectives of the nurses for quality nursing care measurement in Chinese settings; and Liu et al. (2021a, 2021b) constructed indexes for the measurement of quality and safety skills of nursing students through literature, interview, and e-Delphi method. In Kenya, Gathara et al. (2010) established 52 QNCIs. These indicators have made measuring and comparing quality nursing care possible across institutions. However, utilizing any indicators to measure quality nursing care requires further quantification. Uniformity of the quantification across settings and nations, especially in low- and middle-income countries (LMICs), is imperative. QNCIs that considered the above peculiarities are scarce/lacking.
Nevertheless, the need for effective quality nursing care measurement in LMICs has become urgent given the unabating negative healthcare indices in such countries (Ranabhat et al., 2019; WHO, 2019). Africa, of which Nigeria forms a good part, is at the centre of this need given her present low level of quality health care delivery system (Adindu, 2010; Maphumulo & Bhengu, 2019). Why the overseas search for better healthcare has continued among Nigerians/Africans/many citizens of LMICs even in the presence of some level of skilled health workforce may only be attributable to poor focus on the quality of healthcare. Shifting attention to establishing and measuring quality nursing care through a locally shaped nursing care structure, process, and outcome measurement indicators is a redirection attempt to focus on high-quality health outcomes by nurses in LMICs.
None of the available research evidence considered quantifying these QNCIs for ease of comparison and measurement of obtainable quality nursing care, especially in low- and middle-income countries. Also scarce are such QNCIs shaped for ease of QNC measurement developed by African/Nigerian nursing experts. This study initially identified QNCIs, eliminated some of the non-generic indicators considered unsuitable for Nigeria through a modified Delphi process, generated new ones unique to Nigeria, and shaped each of them for ease of usage for QNC establishment and measurement. Precisely, this research answered the question; can generic QNCIs easily utilizable for a low- and middle-income country’s quality nursing care establishment and measurement be developed through a Delphi consensus of Nigerian nursing experts?
3 METHODS
3.1 Design
The study, which lasted for 6 months (October, 2020–April, 2021), utilized a modified Delphi pathway involving three rounds to reach consensus (Eubank et al., 2016; Niederberger & Spranger, 2020). Delphi is recommended for usage in the healthcare industry as a solid technique for achieving consensus on a particular clinical issue (Eubank et al., 2016). Typically, Delphi surveys are conducted in two to three rounds with a carefully selected panel of experts, and numerous modifications to the Delphi approach occurred in recent years (Niederberger & Spranger, 2020). In this study, we modified the Delphi method during the third round, when we asked the experts to accept the items as-is or to recommend ways to improve the emergent items from the second round, without the option of item rejection (having selected the items at a 90 per cent acceptance rate). Process modification usually characterizes many Delphi studies, but no compromise of the research quality should guide such application (Niederberger & Spranger, 2020). Even though two to three rounds of Delphi are frequently utilized (Niederberger & Spranger, 2020), the number of rounds is determined when panellists achieve a solid consensus or when researchers are satisfied with the findings and consider that adding another round would add little value (Fink-Hafner et al., 2019).
3.2 Generation of the first set of items
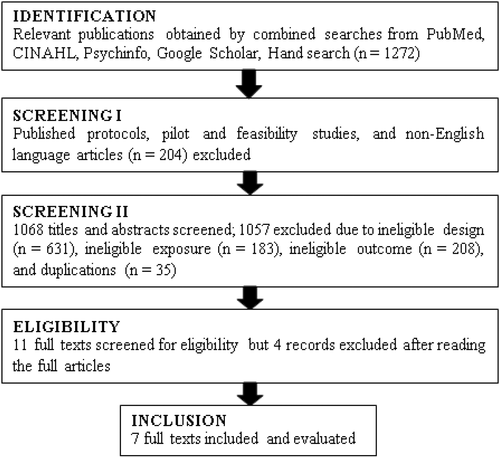
Initially, 96 items (structure – 31, process – 38, and outcome – 27) were developed following a systematic review of relevant literature and authors' contributions. The PECO method was used to define the four major components of the systematic literature search question: P (population) = Nurses; E (Exposure) = Instrumentation; C (comparison) = Not Applicable; O (outcome) = Quality of Nursing Care. We searched PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Psychinfo databases to select applicable works of literature for review. Additionally, we ran a Google and manual search of existing publications' reference lists to identify papers that did not appear in the core repositories. We filtered the publication topics and abstracts yielded by the search technique initially to exclude irrelevant items. We examined the whole text of the remaining articles to determine their eligibility. The research question formed the basis for developing the eligibility criteria for article selection. Only instrumentation studies that aimed to develop or test their psychometric properties published in the English language between 1990 and 2020 were included. However, studies published in books, doctoral dissertations, or reports published in conference proceedings were excluded. Independently, C.O.N. (Reviewer 1) and I.N. (Reviewer 2) initially reviewed the titles and abstracts of the publications obtained by the search method to eliminate irrelevant articles. E.N.D.E. (Reviewer 3), who is more knowledgeable in a systematic review, was consulted whenever there was an irreconcilable difference in the outputs of reviewer 1 and reviewer 2. After the literature search, we further screened the search outputs (1,272 studies) using the eligibility criteria. The summaries of the flow of the literature search are in Table 1 and Figure 1 below.
| Database | Search strategy | Studies |
|---|---|---|
| PubMed | ((“nurse s”[All Fields] OR “nurses”[MeSH Terms] OR “nurses”[All Fields] OR “nurse”[All Fields] OR “nurses s”[All Fields] OR (“nursing”[MeSH Terms] OR “nursing”[All Fields] OR “nursings”[All Fields] OR “nursing”[MeSH Subheading] OR “breast feeding”[MeSH Terms] OR (“breast”[All Fields] AND “feeding”[All Fields]) OR “breast feeding”[All Fields] OR “nursing s”[All Fields])) AND (“instrument*”[All Fields] OR (“develop”[All Fields] OR “develop”[All Fields] OR “developed”[All Fields] OR “developer”[All Fields] OR “developer s”[All Fields] OR “developers”[All Fields] OR “developing”[All Fields] OR “developments”[All Fields] OR “develops”[All Fields] OR “growth and development”[MeSH Subheading] OR (“growth”[All Fields] AND “development”[All Fields]) OR “growth and development”[All Fields] OR “development”[All Fields]) OR (“questionnaire”[All Fields] OR “questionnaire s”[All Fields] OR “surveys and questionnaires”[MeSH Terms] OR (“surveys”[All Fields] AND “questionnaires”[All Fields]) OR “surveys and questionnaires”[All Fields] OR “questionnaire”[All Fields] OR “questionnaires”[All Fields]) OR (“measurability”[All Fields] OR “measurable”[All Fields] OR “measurably”[All Fields] OR “measure s”[All Fields] OR “measureable”[All Fields] OR “measured”[All Fields] OR “measurement”[All Fields] OR “measurement s”[All Fields] OR “measurements”[All Fields] OR “measurer”[All Fields] OR “measurers”[All Fields] OR “measuring”[All Fields] OR “measurings”[All Fields] OR “measurement”[All Fields] OR “measurements”[All Fields] OR “weights and measures”[MeSH Terms] OR (“weights”[All Fields] AND “measures”[All Fields]) OR “weights and measures”[All Fields] OR “measure”[All Fields] OR “measures”[All Fields]) OR (“abstracting and indexing”[MeSH Terms] OR (“abstracting”[All Fields] AND “indexing”[All Fields]) OR “abstracting and indexing”[All Fields] OR “index”[All Fields] OR “indexed”[All Fields] OR “indexes”[All Fields] OR “indexing”[All Fields] OR “indexation”[All Fields] OR “indexations”[All Fields] OR “index”[All Fields] OR “indexer”[All Fields] OR “indexers”[All Fields] OR “indexes”[All Fields]) OR (“benchmarking”[MeSH Terms] OR “benchmarking”[All Fields] OR “metrics”[All Fields] OR “metric s”[All Fields] OR “metronidazole”[MeSH Terms] OR “metronidazole”[All Fields] OR “metric”[All Fields]) OR (“psychometrical”[All Fields] OR “psychometrically”[All Fields] OR “psychometrics”[MeSH Terms] OR “psychometrics”[All Fields] OR “psychometric”[All Fields]) OR (“valid”[All Fields] OR “validate”[All Fields] OR “validated”[All Fields] OR “validates”[All Fields] OR “validating”[All Fields] OR “validation”[All Fields] OR “validational”[All Fields] OR “validations”[All Fields] OR “validator”[All Fields] OR “validators”[All Fields] OR “validities”[All Fields] OR “validity”[All Fields])) AND ((“nursing”[All Fields] AND “care”[All Fields] AND (“indicate”[All Fields] OR “indicated”[All Fields] OR “indicates”[All Fields] OR “indicating”[All Fields] OR “indicative”[All Fields] OR “indicatives”[All Fields] OR “indicators and reagents”[Pharmacological Action] OR “indicators and reagents”[MeSH Terms] OR (“indicators”[All Fields] AND “reagents”[All Fields]) OR “indicators and reagents”[All Fields] OR “indicator”[All Fields] OR “indicators”[All Fields] OR “indices”[All Fields] OR “indices”[All Fields])) OR ((“nursing”[MeSH Terms] OR “nursing”[All Fields] OR “nursing’s”[All Fields] OR “nursing”[MeSH Subheading] OR “breast feeding”[MeSH Terms] OR (“breast”[All Fields] AND “feeding”[All Fields]) OR “breast feeding”[All Fields] OR “nursing s”[All Fields]) AND (“quality of health care”[MeSH Terms] OR (“quality”[All Fields] AND “health”[All Fields] AND “care”[All Fields]) OR “quality of health care”[All Fields] OR (“quality”[All Fields] AND “care”[All Fields]) OR “quality of care”[All Fields])) OR “Quality Nursing Care”[All Fields] OR “Patient satisfaction”[All Fields] OR “Nursing care quality”[All Fields])) AND ((ffrft[Filter]) AND (fha[Filter]) AND (journal article[Filter]) AND (fft[Filter]) AND (humans[Filter]) AND (cam[Filter]) AND (nursing journals[Filter]) AND (1999:2020[pdat]) AND (English[Filter])) | 1,252 |
| CINAHL | Quality nursing instrument development and validation; Quality nursing care indicators; Quality nursing care measurement | 11 |
| Psychinfo | Quality nursing instrument development and validation; Quality nursing care indicators; Quality nursing care measurement | 6 |
| G-Scholar, Hand Search | Nursing, Quality of care, Instrument | 3 |
| Total | 1,272 |
The identification and arrangement of the quality nursing care indicators (QNCIs) were guided by the Donabedian structure, process, and outcome quality model, which postulates that advancement to the care structure should result in advancements to clinical processes, which in turn should result in an improved patient outcome (Moore et al., 2015).
For structure indicators, the concern was on the health facility and its components like enough staff strength, working equipment, safety devices, information system, and the overall organization of activities (El Haj et al., 2013).
The process looked at all the activities going on during healthcare delivery to the clients/patients, the technicality of healthcare delivery, and interpersonal relationship between the provider and the recipient of the care, including observation of rules and standards regulating healthcare practices and appropriateness and skilfulness of actions taken (El Haj et al., 2013; opes Silveira et al., 2015).
Focusing on patient’s health status after delivering care, his safety, his level of satisfaction with the delivered health care (El Haj et al., 2013; Heslop et al., 2019), and the providers’ level of satisfaction with the available structure provided for care guided the development of outcome indicators.
3.3 Participant selection
A Delphi panel might include as few as three members or as many as 80 (Grisham, 2009; Mullen, 2003), but what is critical is to pick individuals who are versed in the subject and are willing to take part in several sessions of inquiries or discussions on the same subject (Grisham, 2009). The selection procedure can be as straightforward or as complicated as necessary, but the objective is to identify professionals in the subject of study and improve the final product’s quality (Ogbeifun et al., 2016). According to Beiderbeck et al. (2021), five essential areas to consider when selecting a Delphi panel are the panel’s size, amount of knowledge, cultural diversity, level of interest, and access to the panel. The authors, however, advised that a minimum of 15–20 experts would suffice for any sub-group of experts.
In this study, twenty-four nurses possessing a minimum of master’s degree in medical-surgical nursing, maternal and child health nursing, nursing administration and management, and education/nursing education who have had up to 10 years of experience in clinical/academic nursing were recruited as the study experts. Ten of the experts possess master’s degree, 14 have Ph.D., and five out of the 14 are professors in their chosen nursing fields.
To have a good nationwide representation, the participants, selected through a snowball, were academic/clinical staff of universities and teaching hospitals, one from each of the six geopolitical zones of Nigeria. The entire recruitment process, done through phone calls and text messages, lasted 6 weeks. Only individuals who accepted to participate after being informed about the study protocols, supplied their e-mail addresses, agreed to receive and reply through the instrument’s soft copies, and agreed to return their replies via their e-mail addresses were included as participants.
3.4 The Delphi rounds
In the first round, the initial 96 Quality Nursing Care Indicators (QNCIs) (structure – 31, process – 38, and outcome – 27) were distributed to the panellists through electronic mail. Follow-up was adequately made through phone calls, text messages, and reminder e-mails until the entire 24 participants responded and sent back the instrument.
The instrument had an introductory part and item generation part, which has three columns of “Accept,” “Reject,” and “Remark,” where the participants, respectively, indicated their acceptance of each item, rejection of each item, and gave reason for their choice or made a suggestion(s) for modification of each item. After each domain of structure, process, and outcome indicators, the instrument had many blank rows for participants' suggestions for additional indicators they felt were lacking in each domain. To accommodate important suggestions for modifying many items, we decided to accept round 1 items at a 75% agreement rate in line with Santaguida et al. (2018).
The exact process above guided round 2 of the study, but one participant could not respond after making every follow-up attempt. However, with a minimum of 10 experts, agreement by at least 80% of the experts is enough to achieve the content validity of items (Eubank et al., 2016; Lynn, 1986). Nevertheless, we increased our item retention decision at a 90% acceptance rate by the experts to ensure a high level of validity.
With no option of item rejection, having selected the items at 90% acceptance rate in round two, the participants responded to two columns of “Accept with no modification” and “Suggestion for modification (if any)” to accept each item with no modification or make a suggestion for modification of each item that emanated from the analyses of responses to the second round. Meanwhile, after exhausting every follow-up attempt, one participant, out of the 24, could not respond, still. Validation of the items was done using the percentage of agreement of the panellists with the items and content validity ratio (CVR) formula of CVR = (Ne-N/2)/(N/2) (where Ne is the proportion of experts who agreed to retain the item; and N is the total number of panellists) (Zamanzadeh et al., 2015).
3.5 Ethical consideration
The Research Ethical Committee of the University of Nigeria Teaching Hospital, Enugu gave ethical approval for this study. Before including them as the study participants, we obtained informed oral consent from the 24 Delphi panellists. We told them that the nature of the study does not portend any physical or emotional harm on any participant, but confidentiality of every information from them was assured. Finally, we assured them that they had the right to withdraw from the study at any of its stages without any threat whatsoever.
3.6 Data analysis
Data from the Delphi rounds were analysed quantitatively using descriptive statistics and qualitatively using qualitative content analysis. The items' acceptance rate or rejection rate was analysed using descriptive statistics of frequencies, percentages, and standard deviation, with the Statistical Package for Social Sciences (SPSS) version 23. Validation of the item contents was estimated using the percentage of agreement of the panellists with the items and content validity ratio (CVR) formula of CVR = (Ne-N/2)/(N/2), where Ne is the number of panellists that agreed to the item retention and N is the total number of panellists (Zamanzadeh et al., 2015).
We performed a qualitative analysis of participant comments and suggestions manually. Comments were coded item-by-item, where similar comments were treated as one and the import was utilized to amend the items as suggested. However, every dissimilar comment emerged as a separate entity which the authors subjected further to manual scrutiny through their opinions. What majority opinion favours after due consideration of the effects of the dissimilar comments on the items determined their reflection on the concerned items. Where the opinion favoured modification of the items in line with the comment, an amendment was made; where it favoured discarding the comment, we made no further change.
4 RESULTS
A systematic literature review and three Delphi rounds with nursing experts were conducted in this study. In the first round, 24 instruments containing the initial 96 items each, sent to the 24 panellists, were all returned – 100% return rate. We reduced the 96 items to 75, which the experts' Delphi consensus supported at a ≥ 75% acceptance rate. In round 2, items were modified and reduced to 74 by 23 (95.83%) out of the 24 panellists representing a CVR of 0.92. Meanwhile, a CVR of 0.78 and above is necessary to consider an item or scale as valid (Frey, 2018). In the final round (round 3), a consensus was reached on 70 items by 23 (95.83%) experts representing a CVR of 0.92. Figure 2 contains a detailed summary of the study processes.
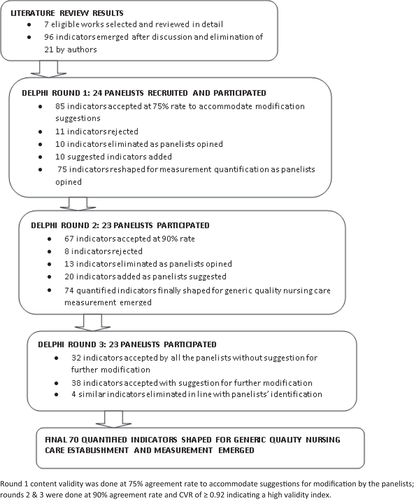
In the final 70 indicators shaped for generic quality nursing care measurement, 28 (40%) items are for quality nursing care structure measurement, 32 (45.71%) items are for quality nursing care process measurement, and 10 (14.29%) are for quality nursing care outcome measurement. The quantified and scalable items are given in Table 2.
| S/N | Quality nursing care indicators |
|---|---|
| Structure indicators | |
| 1 | Presence of mixed skills of general and specialist/experienced nurses (in 70%:30% ± 10% ratio) trained at university and diploma levels in the unit |
| 2 | Minimum of nurse to patient ratio of 1:4 per shift (ward and outpatient) or 1:1 (Intensive Care Unit) |
| 3 | An appropriate number of nurses (a minimum of 1 per shift in a unit) with special information communication training (e.g. managing bad news/prognosis information, counselling, and such likes) |
| 4 | Every nurse in the unit wears the approved uniform with name identity tags on them |
| 5 | Presence of at least a nurse preceptor/educator per shift for in-service training or capacity building of nurses/nurse interns/students in the unit |
| 6 | Presence of a policy that promotes knowledge and skill advancement of nurses through formal training |
| 7 | Presence of intercom facilities connecting relevant sections of the hospital |
| 8 | Visible tools for nurses' documentation of general and specific patient assessment, treatment and monitoring |
| 9 | Adequate number of standard clean and/or sterile unit uniforms (at least 2 clean and/or 2 sterile uniforms per nurse) |
| 10 | Infection-controlled operating room restricted to only users who are properly-dressed in full theatre wears |
| 11 | Functional and standard assessment, monitoring, and treatment instruments such as vital signs equipment, screen, glucometer, forceps, gallipots, and such likes |
| 12 | Neat (no visible hospital wastes, cobweb, dust or stain) and odour-free unit |
| 13 | Comfortable and adequate (1 per patient), well-spaced (≥ 3 feet apart) seat/bed/bed accessories for out/admitted patients |
| 14 | Well-designed (open cubicle(s) with a wide central passage), well-lit and adequately ventilated nurse and patient building |
| 15 | Presence of a nurses' station that allows for monitoring of every patient at a glance |
| 16 | Presence of standard operating procedure for adverse drug effects reporting - availability of adverse reaction reporting tool (e.g. pharmacovigilance form) and line of reporting of incidence |
| 17 | Restricted and per-shift daily stock monitoring record of high-hazard medications (e.g., anticoagulants, narcotics and opiates, insulins, potassium chloride, and sedatives) controlled and administered by the nurses |
| 18 | Visible unit hand hygiene guideline and station with alcohol-based hand rub solution or soap and running water (piped, bucket with a tap, or pour pitcher), and single-use towels/hand drier |
| 19 | Visible adequate (minimum of 1 per 6 patients and 1 per 4 staff members) functional, clean unit toilets/bathrooms |
| 20 | Visible unit’s waste segregation (bins and sharp boxes) |
| 21 | Presence and functional unit’s storage facility for sterile and high-level disinfected items (either a room with limited access or a cabinet that can be closed) |
| 22 | Presence of facility protocol (containing role specifications) for different cadres of nurses |
| 23 | Presence of adequate infection prevention equipment (minimum of 1 set per procedure per nurse or as the concerned unit requires) |
| 24 | Presence of a policy on yearly assessment and improvement of nurses' level of job satisfaction |
| 25 | Presence of a policy for recognizing and rewarding excellence among nurses |
| 26 | Displayed patients' bill of rights (in simple and clear language) readable from every patient’s position in the unit |
| 27 | Presence of unit feedback/suggestion system for nursing services improvement |
| 28 | Presence of effectively functioning nursing services quality assurance committee in charge of the unit |
| Process indicators | |
| 1 | Explains procedure and gains the consent of patient or patient’s representative before commencing the procedure |
| 2 | Does condition-required patient health assessment (e.g. history, head to toe/focused examination, vital signs including other required physiological values, weight/height, and such likes) on admission |
| 3 | Does complete or partly patient health reassessment when the patient’s condition changes |
| 4 | Appropriately and timely documented assessment data |
| 5 | Assesses at-risk patients (identifying the risk nursing diagnoses) for the concerned risk at least once in every shift or six hourly |
| 6 | Makes appropriate nursing diagnosis in line with current NANDA-I on each patient |
| 7 | Formulates and documents nursing care plan to address each diagnosis using appropriate outcome indicators, interventions, timeline and scale in line with NIC and NOC |
| 8 | Involves patient and patient(s) relative(s) (if desired and as chosen by the patient) in the patient’s care decision making |
| 9 | Evaluates and documents care outcome using NOC |
| 10 | Takes decision and action as soon as patient monitoring records indicate a need for that |
| 11 | Complies with hand hygiene guidelines based on established unit/institutional protocols |
| 12 | Wears other infection protective equipment as the concerned unit requires |
| 13 | Works harmoniously (gets along, no squabbles, no open or noisy disagreement, and such likes) with professional colleagues and others working in the hospital |
| 14 | Performs nurses' ward round and documents recommendations appropriately |
| 15 | Assists patients who are unable to perform their activities of daily living to meet these needs as soon as possible |
| 16 | Strictly adheres to the approved/adopted standard/protocol for a given nursing task while performing the task(s) |
| 17 | Performs nursing task(s) timely |
| 18 | Gives health education necessary for the condition in the language the patient(s)/client(s) understands(understand) |
| 19 | Responds to patient’s call promptly |
| 20 | Performs procedures with appropriate improvisation (where imperative) that does not subject the patient and the nurse to risk(s) |
| 21 | Absence of altercation (quarrel, noisy disagreement, and such likes) between the nurse and the patient or patient relative(s) |
| 22 | Maintains good professional rapport/interpersonal communication (e.g. smiling, staying close, active listening, clarification, and the offering of self) with the patient/client or his/her relatives |
| 23 | Provides privacy (when the procedure requires that) and gives a therapeutic touch to the patient (if not culturally forbidden) while rendering care to him/her |
| 24 | Performs holistic nursing care on all the unconscious/critically injured/ill patients |
| 25 | Ensures that each patient on admission wears a correctly-filled armband or has any other unique identifier on him/her |
| 26 | Puts barrier in place for a patient at risk of falling |
| 27 | Monitors/checks (for swollen, soiled, or infiltrated) patients' cannula site and intravenous fluid/treatment progress and initiate action to avert complication if need be |
| 28 | Properly monitors and documents input–output of patients on fluid balance monitoring |
| 29 | Gives and documents patients discharge instructions (education/counselling, follow-up care, return date) |
| 30 | Properly documents every other nursing care given to the patient (e.g., food, drug, observations, and other interventions) |
| 31 | Delegates appropriate tasks to subordinates and supervises them effectively |
| 32 | Recognizes and rewards excellence among followers (i.e. subordinates) by superior |
| Outcome indicators | |
| 1 | Records high rate (≥ 80%) of quick recovery in the unit |
| 2 | Records minimal cases (≤ 2%) of nursing-related avoidable adverse outcomes such as bedsore, nurses' medication error, avoidable inpatient fall, and such likes during patient care in the unit |
| 3 | Satisfactory patient feedback on the attitude of nurses during care through feedback/suggestion system and the result of patient satisfaction survey administered privately during discharge by quality assurance unit |
| 4 | Satisfactory feedback from ≥70% of the patients in the unit on the skills/expertise of the nurses caring for them |
| 5 | Satisfactory feedback from ≥70% of the patients in the unit on the satisfaction they get after each nursing intervention |
| 6 | The patient is knowledgeable (to the extent he/she wants to know) of his/her condition and the care requirement (evidenced in his/her verbalization) |
| 7 | The patient can adhere to his/her independent care requirements (upon discharge) in line with the education received from the nurse |
| 8 | Satisfactory feedback from ≥70% of the nurses (in a shift) in the unit on availability of the needed human, material, and environmental structure for effective service delivery |
| 9 | Absence of hospital-acquired infection(s) – not related to patient’s diagnosed condition during admission |
| 10 | Documented every nursing observation and intervention properly |
5 DISCUSSION
The study developed generic quality nursing care indicators easily utilizable for a low- and middle-income country’s quality nursing care establishment and measurement. The study achieved this aim through a modified Delphi process in which the participating experts reached a consensus on the items after three rounds of participation. Although not fixed at a particular number of rounds, similar studies achieved consensus after three Delphi rounds, and there is the flexibility of the number of rounds to use in Delphi research (Barrett & Heale, 2020; Skulmoski et al., 2007; Vogel et al., 2019). We generated the first set of 96 items through a systematic review of the literature and the researchers’ judgement. Validation of the items was done through a three-round Delphi process by academic and clinical nursing experts recruited from the six geopolitical zones of Nigeria. Percentage of agreement and content validity ratio (CVR) guided the selection/retention of the final 70 items with a high percentage of acceptance and content validity. 80% rate of an agreement by ten or more experts and a CVR of ≥0.78 are appropriate for content validity of items (Eubank et al., 2016; Frey, 2018; Lynn, 1986). The percentage of acceptance of the items in this study was >95%, and the CVR was up to 0.92, hence meeting the content validity criteria.
Adopting the Donabedian structure, process, and outcome framework for quality care measurement (Kunkel et al., 2007; Sharew et al., 2020) helped focus the items on a more holistic dimension to quality nursing care establishment and measurement. For structure indicators, items were developed to help establish and measure the health facility and its other components like enough staff strength, working equipment, safety devices, information system, and the overall organization of healthcare activities (El Haj et al., 2013).
In the developed process indicators, the items were shaped to help focus the nurses' attention on the desired delivery of all the activities going on during healthcare provision to the clients/patients, including the technicality of healthcare delivery, the interpersonal relationship between the provider and the recipient of the care, observation of the rules and standards regulating healthcare practices, and appropriateness and skilfulness of the healthcare actions (El Haj et al., 2013; opes Silveira et al., 2015).
For the outcome indicators, the developed items focused on patients' health status after receiving care, his safety, his level of satisfaction with the delivered healthcare (El Haj et al., 2013; Heslop et al., 2019), and the providers' level of satisfaction with the available structure provided for the care. The nurses' satisfaction is essential because their overall job satisfaction and the quality of care they provide are positively correlated (Aron, 2015).
One can solely use the items under the ‘structure’ to establish and measure the standard required for quality nursing care (QNC) process and outcome. The process items equally provide for sole usage during the nursing care delivery, and strict application of these items can guarantee desired nursing care outcomes. Also, the outcome items provide for broad application in many nursing care settings and can give the required feedback on the quality of nursing care outcomes.
The experts utilized in this study (nurses with a minimum of master’s degree in various specialty areas of nursing) fall within the acceptable standard for a Delphi panel (Avella, 2016; Niederberger & Spranger, 2020). The experts being up to 24 is equally apt for a Delphi study (Staykova, 2019). Recruitment of the experts from different cultures and locations in Nigeria to consider the extent of generalization of the application of the items (Polit & Beck, 2010) was equally a step taken to boost the utilization of these items in many cultures and settings.
The uniqueness and strength of the quality nursing care indicators (QNCIs) developed in this study lie in their ability to quantify the quality indicators so that their usage in low- and middle-income countries (LMICs) will be easy. Considering the World Health Organization (WHO) (2018) recommendation for quality care focus, the experts' holistic nature and vital contributions during the item development phases shaped the items for ease and flexibility of usage in different settings across the globe, especially LMICs. Additionally, the quantified and specific nature of the developed items has made their scaling flexible and easy, and their usage highly possible across the globe, especially the LMICs.
The crux of this study is quality improvement, and assurance in the healthcare delivery system, especially as the belief is that negative health indices in LMICs are associated with insufficient attention to the quality of care (Adindu, 2010; Maphumulo & Bhengu, 2019). The ease with which nurses will likely utilize the items developed in this study for QNC establishment and evaluation has a high propensity to focus their attention on QNC as they discharge their duties. The belief is that nurses' continuous usage of these items, mainly those in LMICs, will change their hitherto lacklustre attitude towards quality of care (Mannava et al., 2015; WHO, 2019) desirously.
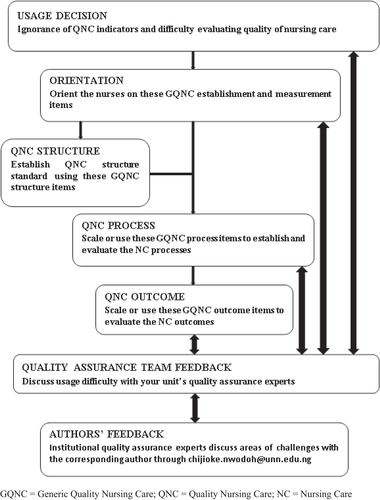
The items' usage is a simple one that starts with the decision to use the items by nurses who may be ignorant of QNC indicators and may not have been measuring the quality of their care against any known standard. Next to this decision is the nurses' orientation on the items developed from this study by the quality assurance team of the unit. With a thorough understanding of the items' function and intended use, the unit’s QNC structure is established and compared to the structure contents of these developed items.
In the next stage, the QNC process items are used to guide the delivery of nursing care by the nurses and maybe scaled and used to measure the QNC being delivered by the nurses through comparing what the nurses do with the standard set in the items. After providing the care, the QNC outcome items are used to assess the extent of compliance of the obtainable outcomes with the expected outcomes exemplified in this study’s QNC outcome items.
At any of the above stages where the nurses encounter items usage difficulty, the quality assurance experts of the unit or the establishment should be consulted for guidance or clarification. The experts can consult this paper’s corresponding author for advice where the solution to the challenges appears elusive. The items’ usage algorithm is contained in Figure 3.
5.1 Limitations
This study took place in Nigeria, and the items were developed through the opinions of Nigeria-based academic and clinical nursing experts from a few universities and university teaching hospitals in the country. Generalizing the study outcome on entire Nigeria would have gained wider acceptability if experts from more institutions in different parts of the country were involved. The opinions of the study panellists cannot also serve as those of other such experts in Nigeria and other low- and middle-income countries (LMICs) without conducting a similar study on them. More comprehensive testing of the items' usability in different parts of Nigeria and other LMICs will determine the generalizability of the study outcome on them. Also, the content validity of the items was done using the percentage of agreement and content validity ratio (CVR) only. Despite the high level of validity recorded with the above two indexes, the validity index of the items would have gained more general acceptability with the use of the item content validity index (I-CVI) measurement.
6 CONCLUSION
This study produced 70 general QNC establishment and measurement items through literature review and experts' opinions in 3 modified Delphi rounds. Because these produced items can guide the establishment of QNC structure standard, its measurement, and measurement of QNC delivery processes and outcomes, the researchers recommend their usage by clinical nurses working in healthcare facilities across the globe, especially in LMICs.
AUTHOR CONTRIBUTIONS
The authors have made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; and were involved in drafting the manuscript or revising it. They gave final approval of the manuscript’s version to be published; take public responsibility for appropriate portions of the content; and agreed to be accountable for all aspects of the work. The contributions of the authors in specific terms include the following: Chijioke O. Nwodoh: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing original draft, Writing review & editing. Ijeoma L. Okoronkwo: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing original draft, Writing review & editing. Ada C. Nwaneri: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing original draft, Writing review & editing. Agnes N. Anarado: Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing original draft, Writing review & editing. Anthonia U. Chinweuba: Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing original draft, Writing review & editing. Ifeoma Ndubuisi: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing original draft, Writing review & editing. Peace Iheanacho: Data curation, Formal analysis, Funding Methodology, Resources, Validation, Visualization, Writing review & editing. Nneka Ubochi: Data curation, Methodology, Project administration, Resources, Visualization, Writing original and review drafts. Echezona N. D. Ekechukwu: Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing original draft, Writing review and editing of the manuscripts.
ACKNOWLEDGEMENT
The researchers are grateful to the Delphi panellists for their active participation in the study.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.