Initial clinical experience with selective bladder denervation for refractory overactive bladder
Abstract
Aims
To report the initial clinical experience with selective bladder denervation (SBD) of the trigone in women with refractory overactive bladder (OAB).
Methods
Females with refractory OAB underwent SBD of the bladder sub-trigone region. Patients were treated using a 10-s voltage-controlled radiofrequency (RF) algorithm (RF10) at study onset. The protocol was modified during the study after which point remaining patients received 60-s temperature-controlled RF (RF60). Patients were followed for 12 weeks and evaluated for adverse events and changes in OAB symptoms. Exploratory analyses on the influence of RF duration were performed.
Results
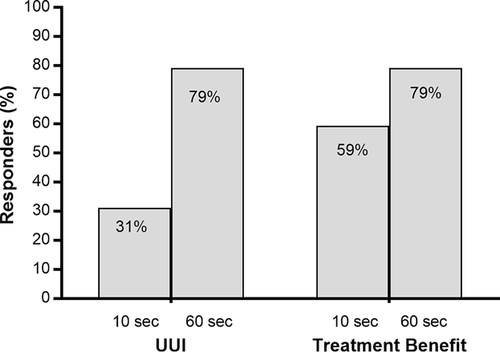
Among 63 patients, SBD resulted in statistically significant and clinically important improvements for most outcomes. Comparing RF10 (n = 34) to RF60 (n = 29), treatment benefit was greater with RF60 including mean reduction in urgency urinary incontinence (−2.5 vs −0.9; P < 0.01), urinary incontinence (−2.6 vs −0.8; P < 0.001), and total urgency and frequency score (−13 vs −7; P = 0.02); and improvements in symptom bother (−33 vs −18; P < 0.01) and quality of life (28 vs 16; P = 0.02) on the OAB questionnaire. The proportion of urgency urinary incontinence treatment responders (≥50% reduction in episodes) was 79% with RF60 and 31% with RF10. The frequency of device- or procedure-related adverse events was comparable in RF10 versus RF60 groups (14.7% vs 17.2%).
Conclusions
This study demonstrated the feasibility of SBD in alleviating symptoms of refractory OAB. A 60-s RF algorithm using deeper ablations of the sub-trigonal tissues was more effective and comparably safe to a 10-s RF algorithm using more superficial ablations.
1 INTRODUCTION
Idiopathic overactive bladder (OAB) is an underdiagnosed and undertreated condition that is defined as urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence (UUI), in the absence of urinary tract infection or other obvious pathology.1 Approximately one in six individuals report symptoms suggestive of OAB, with prevalence increasing with age.2 Symptoms of OAB negatively influence emotional well-being, social interactions, and productivity,3 and affected individuals report decreased health-related quality of life4, 5 and generate more than twice the medical costs of those without symptoms.6, 7
Initial management of OAB generally includes behavioral therapy consisting of bladder re-training, pelvic floor rehabilitation, and/or fluid management strategies. Oral therapies are second-line treatment options if conservative management fails to provide satisfactory symptom relief. Unfortunately, most patients eventually discontinue therapy with antimuscarinics and beta-3 agonists due to dissatisfaction with treatment response or intolerance of side effects.8, 9 In patients whose symptoms are refractory to oral therapy, several third-line treatment options may be considered including botulinum toxin A (BTA) injections, sacral neuromodulation, and percutaneous tibial nerve stimulation (PTNS), all of which provide therapeutic benefit.10 However, each of these treatments are associated with distinct limitations. BTA injections provide symptomatic relief for about 6 months, but side effects include urinary tract infection and urinary retention requiring catheterization. Further, repeat BTA injections result in shorter duration of action with less than 20% of patients remaining on therapy by the seventh cycle.11 Sacral neuromodulation involves surgical placement of a permanent lead and generator that are replaced approximately every 5 years. Patients undergoing sacral neuromodulation may experience pain, electric shock, lead migration, infection, and may require additional interventions to manage these complications.12, 13 Finally, PTNS is a time-consuming procedure, typically involving weekly office visits over a 12-week period followed by less frequent visits and ongoing patient compliance to sustain treatment benefit. Given the shortcomings of available third-line OAB therapies, there is a clinical need for a treatment with at least comparable efficacy, but with longer durability and better tolerability.
The modified Ingelman-Sundberg surgical procedure causes de-afferentation of the nerves from the bladder base as a means of treating OAB.14 In order to achieve a similar therapeutic effect while avoiding risks inherent to surgery, a selective bladder denervation (SBD) procedure was developed that involves radiofrequency (RF) ablation of the bladder sub-trigone region containing afferent sensory nerves. Radiofrequency ablation is the most commonly used percutaneous ablation technique and its safety among numerous clinical applications is well documented.15 While initial safety of this technique was demonstrated in a preclinical study using an ovine model,16 SBD for OAB in humans has not been reported. The primary purpose of this study was to explore the safety and efficacy of SBD to alleviate refractory OAB symptoms in women.
2 MATERIALS AND METHODS
2.1 Study design
This was a prospective, multicenter case series of SBD for treatment of symptomatic idiopathic OAB in women who were unresponsive or intolerant to oral medication. All research procedures performed in this study were in strict accordance with a common, pre-defined protocol that was prospectively registered at ClinicalTrials.gov (NCT02398578). The investigational protocol and informed consent form were approved by the ethics committee of each site, and all study participants gave written informed consent prior to study participation.
2.2 Patient screening
Participants with symptoms of idiopathic OAB underwent a staged screening process with eligibility assessed at each stage to avoid unnecessary testing. Initial screening included medical history assessment, serum creatinine, and urinalysis among all participants, and pregnancy testing in premenopausal women. Patients taking antimuscarinics, beta-3 agonists, or antispasmodics completed a 2-week washout period before screening continued. Patients then underwent cystoscopy and ultrasonography of the urinary tract. Baseline assessments consisted of a 3-day bladder diary, the Overactive Bladder Questionnaire (OAB-q), Kings Health Questionnaire, and measurement of post-void residual urine volume via bladder scan or urethral catheterization. During the study after the inadvertent inclusion of a patient with a congenital abnormality, the screening evaluation was modified to additionally include specific evaluation of trigonal anatomy and confirmation of ureteral patency by observing urine efflux from each ureteric orifice.
Eligible patients were adult females with idiopathic OAB of at least 6 months duration who were unresponsive or intolerant to oral medication, with micturition frequency of at least eight times daily, and post-void residual urine volume of less than 100 mL. Key exclusion criteria were predominant stress or functional incontinence; recent medical therapy for OAB without sufficient washout; BTA injection within 6 months; pelvic electrostimulation treatment in the last 15 days; surgical/interventional procedure involving the pelvic organs; urinary tract infection or history of recurrent infections; anatomical abnormality of the urinary tract; or systemic or neurological causes of OAB symptoms. A complete list of inclusion and exclusion criteria is available elsewhere.17
The first patients enrolled in this study were treated by applying a voltage-controlled RF algorithm for 10 s (RF10). Review of interim efficacy data with the RF10 protocol revealed that symptom improvement was statistically significant but of marginal clinical importance. Based on these data and results of ovine experiments that showed that a 60-s ablation resulted in greater lesion depth which would likely have greater impact on the nerves coursing below the trigone without causing a full thickness ablation,16 it was hypothesized that ablation depth with RF10 was insufficient to fully efface the nerves necessary to disrupt afferent fibers beneath the trigone and that a potentially more effective 60-s RF protocol could be safely implemented. Consequently, the protocol was amended to specify RF ablations using a temperature-controlled algorithm for 60 s (RF60) to achieve a deeper ablation for the remainder of the study. The inclusion criteria were also modified at this time from specifying no minimum UUI frequency in the RF10 group to requiring at least 3 UUI episodes on a 3-day diary in the RF60 group.
2.3 Study device and procedures
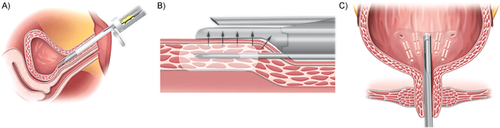
Investigators were experienced in performing female cystoscopies and received training on the study device and procedure prior to patient enrollment. SBD was applied to the urinary bladder trigone using a specialized cystoscopic device that allows direct visualization of the bladder and trigone throughout the procedure. After cystoscopic examination of the bladder, under direct visualization, the thermal delivery probe was placed along the left border of the trigone 5 mm below the ureteric orifice and suction was applied to anchor the device in place (Figure 1A). The electrodes were then advanced 3 mm below and parallel to the urothelium, with RF energy applied to create a suburothelial ablation (Figure 1B). The procedure was repeated on the right border of the trigone and the number of subsequent ablations created between the two initial ablations was determined by the size of the trigone to ensure coverage of the entire area (Figure 1C). At completion of each procedure, the bladder was drained of residual urine and filled with 200 mL of saline or water prior to removal of the cystoscope. Patients were discharged after demonstrating spontaneous voiding.
2.4 Patient follow-up
Structured telephone follow-up assessments were conducted at 2 weeks to determine the occurrence of adverse events. Patients returned for follow-up visits at 4 and 12 weeks, with assessments consisting of a 3-day bladder diary, bladder scan, or catheterization to measure post-void residual urine volume, completion of questionnaires, and review of medications and adverse events. Treatment with oral medications or other third-line therapies was not allowed during the 12-week follow-up period. Patient follow-up in this study is ongoing for 2 years.
2.5 Outcomes
Key outcomes of this study included bladder diary variables, bladder health questionnaires, and adverse events. Urgency urinary incontinence responders were defined as patients with ≥50% reduction in daily UUI episodes. The total urgency and frequency score (TUFS)18 was calculated by adding patient perception of intensity of urgency scale scores of each void on the bladder diary and dividing the sum by the number of days of diary data. Bladder health questionnaires included the OAB-q, Kings Health Questionnaire, and the Treatment Benefit Scale. Treatment Benefit Scale responders were defined as patients reporting that OAB symptoms were “Greatly Improved” or “Improved”. Adverse events were categorized by seriousness and relationship to the procedure or study device. All adverse events were adjudicated by an independent clinical events committee.
2.6 Data analysis
A priori power analysis was not performed since this was a feasibility study of the initial human experience with SBD. Continuous data were reported as mean and standard deviation or median and interquartile range. Categorical data were reported as counts and percentages. Exploratory comparison of baseline characteristics in patients treated with RF10 or RF60 was performed using an independent samples t-test or Fisher's exact test. Longitudinal changes in patient outcomes were analyzed with repeated-measures analysis of variance. Change from baseline in outcomes was compared in the RF10 and RF60 groups using analysis of covariance where the pretreatment value was used as a covariate to control for baseline group differences. Univariate logistic regression was used to identify predictors of UUI responders. Data were analyzed using SAS version 9.4 (SAS Institute, Cary, NC).
3 RESULTS
3.1 Participants
A total of 63 females with refractory OAB were enrolled between March 2015 and April 2017—34 treated with the RF10 protocol and 29 treated with the RF60 protocol. Mean patient age was 67 ± 10 years and median OAB symptom duration was 7 years. Nearly half (47.6%) of the patients required a 2-week washout from oral medications. Prior attempts with third-line therapies included sacral neuromodulation (15.9%), BTA injection (12.7%), and PTNS (1.6%). Baseline patient characteristics included 3.6 ± 2.5 daily UUI; 8.1 ± 3.5 daily urgency episodes; mean OAB symptom bother of 72 ± 18 (0-100 scale), and 94% OAB wet (incontinent) based on the 3-day diary. Comparing patient demographics and medical history of the RF10 versus RF60 groups, age (mean 67 vs 66 years), parity (82% vs 86%), and symptom duration (median 7 years in each group) were comparable although patients in the RF60 group presented with higher body mass index (mean 29 vs 32 kg/m2), lower frequency of smoking history (62% vs 31%), and a lower rate of exposure to third-line OAB treatments. Baseline symptom severity was greater in the RF60 group for daily UUI (4.6 vs 2.8), daily UI (4.6 vs 2.9), and daily urgency episodes (9.1 vs 7.3) (Table 1). With patients under conscious sedation (78%) or general anesthesia (22%), an average of 4 (range: 3-6) RF ablations were performed per procedure. Follow-up data at 12 weeks were available for 61 (96.8%) patients—two patients in the RF10 group withdrew due to lack of efficacy.
| Radiofrequency duration | ||||
|---|---|---|---|---|
| Variable | Total (n = 63) | 10 s (n = 34) | 60 s (n = 29) | Between group P-value |
| Female sex | 63 (100) | 34 (100) | 29 (100) | >0.99 |
| Age, years | 66.9 ± 9.7 | 67.3 ± 10.1 | 66.4 ± 9.3 | 0.69 |
| Body mass index, kg/m2 | 30.1 ± 5.1 | 28.8 ± 4.4 | 31.6 ± 5.5 | 0.03 |
| Smoking history | 30 (47.6) | 21 (61.8) | 9 (31.0) | 0.01 |
| Parity | 0.62 | |||
| 0 | 10 (15.9) | 6 (17.6) | 4 (13.8) | |
| 1 | 10 (15.9) | 5 (14.7) | 5 (17.2) | |
| ≥2 | 43 (68.3) | 23 (67.6) | 20 (69.0) | |
| Recent medical therapyb | 30 (47.6) | 11 (32.4) | 19 (65.5) | <0.01 |
| Prior sacral neuromodulation | 10 (15.9) | 9 (26.5) | 1 (3.4) | 0.02 |
| Prior BTA injection | 8 (12.7) | 6 (17.6) | 2 (6.9) | 0.27 |
| Prior PTNS | 1 (1.6) | 0 | 1 (3.4) | 0.46 |
| Symptom duration, yearsc | 7 (4-14) | 7 (3-13) | 7 (5-15) | 0.60 |
| OAB wet | 59 (93.7) | 30 (88.2) | 29 (100) | 0.12 |
| Daily UUI episodes | 3.6 ± 2.5 | 2.8 ± 2.4 | 4.6 ± 2.4 | <0.01 |
| Daily UI episodes | 3.7 ± 2.6 | 2.9 ± 2.6 | 4.6 ± 2.4 | <0.01 |
| Daily urgency episodes | 8.1 ± 3.5 | 7.3 ± 3.7 | 9.1 ± 2.9 | 0.04 |
| Daily voids | 12.7 ± 3.3 | 12.9 ± 3.6 | 12.5 ± 2.9 | 0.63 |
| TUFSd | 35.7 ± 9.4 | 33.7 ± 10.2 | 38.2 ± 7.9 | 0.06 |
| Nightly nocturia episodes | 2.3 ± 1.9 | 2.5 ± 2.3 | 2.1 ± 1.4 | 0.36 |
- BTA, botulinum toxin A; OAB, overactive bladder; PTNS, percutaneous tibial nerve stimulation; TUFS, total urgency and frequency score; UI, urinary incontinence; UUI, urgency urinary incontinence.
- a Values are mean ± standard deviation or count (percentage) unless noted otherwise.
- b All enrolled patients were previously unresponsive or intolerant to oral medication. Recent medical therapy is defined as oral medication use within 2 weeks of patient screening that necessitated a washout period at least 2 weeks duration before study enrollment.
- c Values are median (interquartile range).
- d Calculated as sum of Patient Perception of Intensity of Urgency Scale score for every void on bladder diary divided by number of days of diary capture.
3.2 Efficacy outcomes
Among all patients, statistically significant improvements from baseline were identified in daily mean episodes of UUI (−1.6), UI (−1.6), urgency (−3.4), and urinary micturition frequency (−1.5). Further, mean reduction in TUFS was 10 points, which mitigates against the possibility of defensive voiding resulting in a reduction of urgency and UUI episodes. On the OAB-q, symptom bother was reduced and quality of life increased (both P-values <0.001). Comparing RF10 to RF60 groups using analysis of covariance that controls for baseline group differences, patients in the RF60 group reported greater improvements in UUI (−2.5 vs −0.9; P < 0.001), UI (−2.6 vs −0.8; P < 0.01), TUFS (−13 vs −7; P = 0.02), symptom bother (−33 vs −18; P < 0.01) and quality of life (28 vs 16; P = 0.02) (Table 2). There were no statistically significant changes in mean post-void residual urine volume with RF10 (−9 mL) or RF60 (+7 mL) compared to baseline. The proportion of UUI treatment responders was 79% with RF60 and 31% with RF10. The frequency of Treatment Benefit Scale responders (reporting “Greatly Improved” or “Improved”) was higher with RF60 vs. RF10 (79% vs 59%) (Figure 2).
| Radiofrequency durationb | ||||
|---|---|---|---|---|
| Variable | Totala (n = 63) | 10 s (n = 34) | 60 s (n = 29) | Between group P-value |
| Daily UUI episodes | −1.6c | −0.9c | −2.5c | <0.01 |
| Daily UI episodes | −1.6c | −0.8c | −2.6c | <0.001 |
| Daily urgency episodes | −3.4c | −2.6c | −4.3c | 0.07 |
| Daily voids | −1.5c | −1.5c | −1.4c | 0.82 |
| TUFSd | −10c | −7c | −13c | 0.02 |
| Nightly nocturia episodes | −0.3 | −0.1 | −0.5 | 0.28 |
| Urinary volume per void, cc | +4 | +5 | +4 | 0.96 |
| KHQ: Incontinence Impact (0-100 scale) | −32c | −25c | −39c | 0.08 |
| OAB-q: Symptom bother (0-100 scale) | −25c | −18c | −33c | <0.01 |
| OAB-q: HRQL total (0-100 scale) | 21c | 16c | 28c | 0.02 |
- HRQL, health-related quality of life; KHQ, King's Health Questionnaire; OAB-q, overactive bladder questionnaire; TUFS, total urgency and frequency score; UI, urinary incontinence; UUI, urgency urinary incontinence.
- a Values are mean change from baseline.
- b Values are least-squares mean change from repeated measures analysis of covariance controlling for baseline value.
- c Statistically significant change from baseline to 12 weeks.
- d Calculated as sum of Patient Perception of Intensity of Urgency Scale score for every void on bladder diary divided by number of days of diary capture.
3.3 Predictors of treatment response
A univariate logistic regression model was developed to determine the independent association of baseline patient characteristics and RF duration with the odds of UUI treatment response. In this analysis, RF duration (RF60 vs RF10) was the strongest predictor of UUI treatment responders (odds ratio = 8.4, 95%CI: 2.6-27, P < 0.001). Patients with no prior history of smoking were also more likely to achieve UUI treatment response (odds ratio = 5.8, 95%CI: 1.9-17, P < 0.01). No other baseline patient characteristic or the number of RF ablations applied was associated with UUI treatment response (Table 3).
| Variable | Comparison | Odds ratio | 95%CI | P-value |
|---|---|---|---|---|
| Radiofrequency duration | 60 vs 10 s | 8.4 | 2.6, 27 | <0.001 |
| Smoking history | No vs yes | 5.8 | 1.9, 17 | 0.002 |
| Recent medical therapyb | Yes vs no | 2.8 | 1.0, 7.9 | 0.06 |
| Parity | No vs yes | 4.2 | 0.8, 20 | 0.09 |
| Prior sacral neuromodulation | No vs yes | 3.3 | 0.8, 14 | 0.11 |
| Symptom duration | Per 1 year decrease | 1.1 | 1.0, 1.1 | 0.14 |
| Body mass index | Per 1 kg/m2 increase | 1.1 | 1.0, 1.2 | 0.22 |
| Number of ablations performed | 5 or 6 vs 3 or 4 | 1.4 | 0.4, 4.5 | 0.60 |
| Age | Per 1 year decrease | 1.0 | 1.0, 1.1 | 0.79 |
| Prior BTA injection | No vs yes | 1.2 | 0.3, 5.4 | 0.80 |
- BTA, botulinum toxin A; CI, confidence interval; OAB, overactive bladder.
- a Treatment response defined as ≥50% reduction in urgency urinary incontinence episodes.
- b All enrolled patients were previously unresponsive or intolerant to oral medication. Recent medical therapy is defined as oral medication use within 2 weeks of patient screening that necessitated a washout period at least 2 weeks duration before study enrollment.
3.4 Postprocedural pain and adverse events
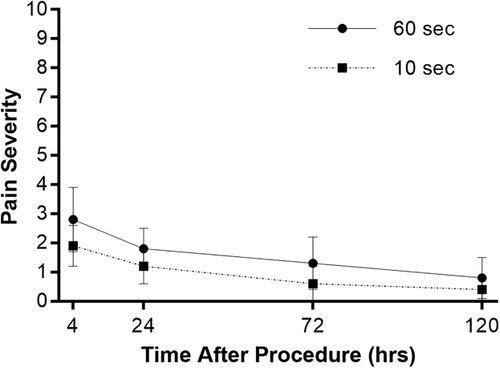
Postprocedural pain assessed over a 5-day period was minimal with SBD. Among all patients, mean pain scores on a 0-10 scale were 2.3 ± 2.6 at 4 h postprocedure and declined steadily to 0.5 ± 1.5 at 5 days. No differences in postprocedural pain were noted between RF10 and RF60 groups (Figure 3).
Of the 63 women enrolled in the study, 1 (1.6%) experienced a serious adverse event. The first patient enrolled in the RF60 group developed an obstruction of the left ureter resulting in pyelonephritis and hydronephrosis, which presented 8 days after the procedure. This event was attributable to RF ablation in association with an ipsilateral undiagnosed congenital ureterocele, which was later identified on magnetic resonance imaging. A ureteral stent was placed and symptoms resolved within 90 days of the procedure. Following this event which prompted the subsequent implementation of more thorough screening procedures, no enrolled patient presented with anatomical abnormalities of the urinary tract and no further serious adverse events occurred. Adverse events attributable to the study device or procedure were reported in 10 (15.9%) patients—most commonly urinary tract infection (reported in 9.5% of patients). There were no statistically significant or clinically important differences between RF10 and RF60 groups for any adverse event (Table 4). There were no occurrences of fistula, perforation, significant bleeding, or urinary retention requiring intermittent catheterization.
| Radiofrequency duration | ||||
|---|---|---|---|---|
| Variable | Total (n = 63) | 10 s (n = 34) | 60 s (n = 29) | Between group P-value |
| Any serious AE | 1 (1.6) | 0 | 1 (3.4) | 0.46 |
| Any device- or procedure-related AE | 10 (15.9) | 5 (14.7) | 5 (17.2) | >0.99 |
| Any AE | 12 (19.0) | 6 (17.6) | 6 (20.7) | >0.99 |
| Urinary tract infection | 6 (9.5) | 4 (11.8) | 2 (6.9) | 0.68 |
| Burning sensation | 1 (1.6) | 0 | 1 (3.4) | 0.47 |
| Dermatitis | 1 (1.6) | 1 (2.9) | 0 | >0.99 |
| Lower urinary tract symptoms | 1 (1.6) | 1 (2.9) | 0 | >0.99 |
| Pain | 1 (1.6) | 0 | 1 (3.4) | 0.47 |
| Ureteral obstruction | 1 (1.6) | 0 | 1 (3.4)a | 0.47 |
| Urethral bulge | 1 (1.6) | 0 | 1 (3.4) | 0.47 |
| Vaginitis | 1 (1.6) | 0 | 1 (3.4) | 0.47 |
| Urinary retentionb | 0 | 0 | 0 | >0.99 |
- AE, adverse event.
- a Classified as a serious adverse event due to hospitalization with ureteral stent placement.
- b Defined as retention sufficient to require intermittent catheterization.
4 DISCUSSION
This is the first study to evaluate a strategy of SBD for treatment of refractory OAB. The approach was found to be not only feasible but also safe in the absence of anatomical abnormality and effective in resolving long-standing refractory OAB symptoms. The study also demonstrated that a 60-s RF algorithm using deeper RF ablations was more effective and comparably safe to a 10-s RF algorithm using more superficial ablations.
A considerable number of patients with OAB fail to respond to conservative therapy due to unsatisfactory response or intolerability. Historically, augmentation cystoplasty and urinary diversion were mainstay treatments for refractory cases, but patient unwillingness to undergo surgery and increased surgical risk due to existing comorbidities limit their utility. Minimally invasive OAB therapies have recently gained traction with primary goals of higher patient willingness, sustained efficacy, and low complication risk. While the underlying causes of idiopathic OAB remain uncertain, the prevailing theories involve neurogenic and/or myogenic mechanisms. The afferent C-fiber type trigonal nerves that are densely located within the submucosa, detrusor muscle, and adventitia are up-regulated in OAB, which alters luminal sensing and results in urgency and uncontrollable detrusor contractions.19 Consequently, the trigone has become a therapeutic target for minimally invasive third-line OAB treatments. Initial results of this study provide support for a neurogenic etiology and indicate that SBD of the trigone may be a valuable addition to the urological armamentarium to treat refractory OAB symptoms.
Efficacy through 12 weeks in the RF60 group was comparable to that of other minimally invasive third-line OAB treatments. The proportion of treatment responders with SBD at 12 weeks was 79%. This compares favorably with treatment success rates of 61% with BTA injections,20 50% with sacral neuromodulation (accounting for 20% who complete test stimulation but do not receive the full implant),21 and 55-80% with PTNS22 over the same period. There is no current consensus regarding the optimal third-line treatment for refractory OAB symptoms and no single therapy is consistently preferred by patients.23, 24 Ultimately, while each of these therapies is associated with a distinct risk to benefit profile, a therapeutic gap remains for a minimally invasive treatment with durable efficacy and low risk of complications. Relative to other third-line therapies, potential advantages of SBD include avoidance of common complications requiring additional interventions (vs sacral neuromodulation), multiple treatments (vs PTNS), and considerable risk of urinary retention requiring intermittent catheterization (vs BTA injections). A disadvantage of SBD is that most cases were performed with intravenous sedation and, less commonly, general anesthesia. In contrast, BTA, sacral neuromodulation, and PTNS are performed with local anesthesia in some cases. There are no theoretical reasons to believe that SBD could not be carried out under local anesthesia and a study is planned to test this. An interesting observation with SBD was a lower success rate in women with a history of smoking. Smoking is associated with greater OAB severity25 and, therefore, it is plausible that the benefit derived from SBD may be partially offset by the deleterious effects of smoking. The independent association of smoking with SBD efficacy warrants additional investigation in future studies.
The safety profile of SBD was favorable through 12 weeks, with most complications of minimal or moderate severity that resolved without clinical sequalae. Urinary tract infection was the most common adverse event, reported in 6.9% of RF60 patients. There were no cases of urinary retention requiring intermittent catheterization in the current study, which compares favorably to rates of 5% to 35% reported with BTA injections.20, 26 Supportive evidence for the safety of 60-s RF ablation was derived from a preclinical ovine study where healing was assessed periodically over 90 days.16 In this study, complete nerve necrosis was observed within the target tissue, neither the urothelium nor the vaginal mucosa was affected, and no complications such as ureteral/urethral alterations or vesico-vaginal fistulas were identified. Overall, preliminary results suggest that SBD is safe for use in female OAB patients.
There were several limitations of this study that warrant further discussion. First, notwithstanding the strong association of increased RF duration with improvements in clinical efficacy, this was a nonrandomized first-in-human feasibility study and, therefore, the consequent risk of bias and confounding must be acknowledged. Second, the conclusions of this study are limited to 12 weeks follow-up. Longer term results from this study are eagerly awaited and would help to clarify whether SBD results in durable clinical efficacy. Third, the limited sample size may have been insufficient to detect rare adverse events. Finally, this study did not utilize a control group and, therefore, data comparisons with SBD to other OAB therapies should be interpreted cautiously. Larger controlled studies with longer term follow-up are warranted to confirm these initial favorable efficacy and safety results with SBD in the treatment of refractory OAB. The observation of superior efficacy of the RF60 group relative to the RF10 group with no increased safety concerns has prompted consideration of future controlled studies in patients with refractory OAB.
5 CONCLUSION
SBD of the trigone shows promising results in alleviating symptoms of refractory OAB in women through 12 weeks follow-up. These results also suggest that a 60-s RF algorithm using deeper contiguous ablations is more effective and comparably safe to a 10-s RF algorithm using more superficial ablations.