Upper airway stimulation for Obstructive Sleep Apnoea (OSA): A new paradigm of treatment
Abstract
Obstructive Sleep Apnoea (OSA) is a chronic condition, caused by anatomical factors associated with a progressive loss of muscular tone of the tongue and pharyngeal walls, producing upper airways collapse with oxygen desaturation during sleep. Hypoglossal nerve stimulation (HNS) is an innovative and physiological technique, with validated positive effects, to treat patients with OSA who have failed or refused continuous positive airway (cPAP) standard therapy. HNS is a mixed medical and surgical procedure consisting of an electrical stimulation of the medial branches of the hypoglossal nerve—activating the genioglossus muscle (GM) that is the primary protrusor muscle of the tongue—by an implanted cuff electrode connected to a pulse generator and to a respiratory-sensing lead. The purpose of HNS is to increase the neuromuscular activity and the tone of the tongue during sleep in order to avoid upper airway collapse and improve airflow. Compared to traditional surgical procedures, HNS is more conservative and produces a titratable and potentially reversible activation of upper airway dilatators muscles, without definitive anatomical modifications. A strict multidisciplinar approach, from patient clinical evaluation to neurostimulator programming and follow-up, is of crucial importance to achieve a successful implantation. Limitations of HNS are the uncertainty about the long-term adherence and effectiveness and high costs of the device. Further clinical studies are needed to improve the technological features of the current devices and to optimize patients selection criteria in order to identify best responders and to achieve higher cure rates.
1 INTRODUCTION
Obstructive sleep apnoea (OSA) is a multifactorial syndrome characterized by intermittent and repetitive collapse of the upper airway during sleep that causes sleep fragmentation and oxygen desaturation (Strollo & Rogers, 1996). Untreated OSA is significantly associated with cardiac and cerebrovascular diseases, metabolic disorders and adverse events, for example, road accidents due to excessive daytime sleepiness.
From a physiopathological point of view, this clinical condition depends on anatomical and neuromuscular factors causing progressive loss of muscular tone in the tongue and pharyngeal walls resulting in partial or complete collapse of upper airways during sleep. The genioglossus muscle (GM), one of the largest extrinsic muscles of the tongue responsible for its protruding, dilates the pharyngeal space and plays a crucial role in maintaining upper airway patency during sleep (Oliven et al., 1996). Hypoglossal nerve (HN) phasically activates the GM during inspiration to contrast pharyngeal collapsibility during sleep. Inadequate pharyngeal muscles responsiveness to negative intraluminal airway pressure and impaired neuromuscular feedback loop with a reduced neural drive to dilators muscles during sleep, combined with anatomo-morphological abnormalities, contribute to the development of OSA (Ramirez et al., 2013; Zaidi et al., 2013).
Continuous positive airway pressure (cPAP) is currently considered the standard first-line therapy for the treatment of OSA. Although cPAP is effective in the treatment of OSA, patient acceptance and adherence in the long time period are often poor and highly variable ranging from 30% to 85%, as reported in literature (Morrone et al., 2020). Surgery may be considered as a primary treatment option in selected patients with OSA when upper airway obstructive sites are clearly identifiable and amendable (e.g., obstructive tonsils) or as a second line or ‘salvage’ therapy in patients who have failed or refused cPAP therapy. A wide array of surgical procedures and approaches can be employed to treat OSA. Traditional Otorhinolaryngologic surgical procedures for OSA aim to increase upper airway patency by removing obtruding tissues (tonsillectomy, tongue base reduction) and/or remodelling collapsible muscular structures (pharyngoplasty, hyoid bone suspension), either with endoscopic or open approaches. Although surgical techniques have been evolved over time becoming less invasive and reducing side effects and morbidity, alternative more conservative procedures were proposed and advocated in recent times (Kezirian et al., 2010).
Over the years, electrical neurostimulation therapy has been successfully applied to many anatomical sites and neural systems. Vagus nerve stimulation (VNS) was the first system approved for drug-refractory epilepsy and depression (Howland, 2014). Recently, stimulation of the hypoglossal nerve (HNS) was introduced as a innovative surgical technique consisting of an implantable and titratable medical device, electrically stimulating muscles of the tongue in order to improve overall tone and increase pharyngeal airway space (Soose & Gillespie, 2016; Soose et al., 2016). This mixed surgical and medical procedure experienced a rapid development over the last years with promising results in the treatment of appropriately selected adult patients with moderate to severe OSA (Certal et al., 2015; Dedhia et al., 2015; Green & Woodson, 2016; Heiser et al., 2018; Whelan & Soose, 2020). The purpose of targeted stimulation of HN is to increase neuromuscular activity and tone of the tongue during sleep in order to avoid upper airway collapse and improve airflow.
This review paper explores the clinical role of HNS in OSA therapy in the light of recent evidence in literature and technological advances.
2 EXPERIMENTAL EVIDENCES AND CLINICAL APPLICATION
After animal studies have confirmed that GM is the primary tongue protrusor muscle, preliminary human studies demonstrated that electrical stimulation of the GM resulted in anterior displacement of the tongue with subsequent enlargement and stabilization of the retrolingual space (Schwarz et al., 1996; Oliven et al., 2007). The neurostimulator surgically implanted activates the GM by delivering electrical impulses to the hypoglossal nerve without causing arousals. Protrusion of the tongue also produces, to a lesser degree, a retropalatal airway enlargement through a coupling mechanism with the muscles of the soft palate. Therefore, this novel therapeutic approach combines a surgical procedure with a programmable medical device. After preliminary studies with electrical intramuscular stimulation, Schwartz in 2001 reported the first human pilot trial on the neurostimulation of HN in few OSA patients.
Several clinical studies recently proved the safety and effectiveness of HNS in treating OSA patients with significant improvement in the AHI (Apnoea–Hypopnea Index) severity and in the sleep-specific quality-of-life outcomes. A randomized trial demonstrated that the withdrawal of tongue neurostimulation in OSA patients cancels the positive effects of treatment that, vice versa, can be restored by reactivating the device (Strollo et al., 2014; Woodson et al., 2014). A 12-month prospective study on 126 patients showed that median AHI and oxygen desaturation events decreased 68% and 70%, respectively, with improvement in secondary quality-of-life endpoints (Woodson et al., 2016).
2.1 Patient selection criteria
Hypoglossal nerve stimulation is a novel technique that was found to be effective in treating selected OSA patients who have failed or refused continuous positive airway (cPAP) standard therapy.
The clinical variables making a patient an optimal candidate for HNS are considered a predominant anterior–posterior retrolingual collapse identified at endoscopic examination and a body mass index (BMI) <32 kg/m2 (Costantino et al., 2020). OSA severity, baseline BMI, younger age <65 years and upper airway pattern of collapse evaluated at drug-induced sleep endoscopy (DISE) are the main factors predictive of response to HNS (Vanderveken et al., 2013; Wray & Thaler, 2016). DISE, a dynamic endoscopic evaluation of upper airways during sedation mimicking sleep in operating room, is currently recommended as pre-operative diagnostic tool to better select OSA patients for surgical treatment and for implanted HN neurostimulation. Over the time, the eligibility criteria to be implanted with a HN neurostimulator were updated and extended to other patient groups (Sarber et al., 2020; Withrow et al., 2019). However, optimal candidates to HNS may be identified in the future according to better knowledge of OSA pathophysiology and larger prospective clinical trials.
2.2 Hypoglossal nerve stimulation technology and implantation procedure
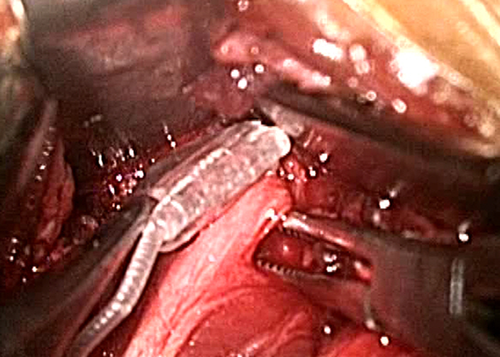
The hypoglossal nerve stimulation systems consist of at least two surgically implantable components: a titratable and adjustable—pacemaker-sized—pulse generator (containing a battery) inserted in a subcutaneous pocket in the right upper chest and a stimulating cuff electrode placed on the HN in the submandibular region (Friedman et al., 2016; Heiser, Hofauer et al., 2016; Heiser, Thaler et al., 2016). In a targeted strategy of selective HN neurostimulation, an intraoperative neuromonitoring with a bipolar probe and a nerve integrity monitoring (NIM) system are crucial to properly identify the protrusion branches of the nerve in order to optimize the upper airway enlargement (Strollo et al., 2014). Therefore, in this HNS methodology the key point is the selective identification by surgical micro-dissection of the medial branches of the hypoglossal nerve (innervating the protruding muscles genioglossus and geniohyoid) where the stimulation lead must be placed (Figure 1). Intraoperative neuromonitoring allows to directly visualize the muscle contractions and the tongue protrusion by electrically stimulating specific neural fibres (Heiser, Hofauer et al., 2016; Heiser, Thaler et al., 2016).
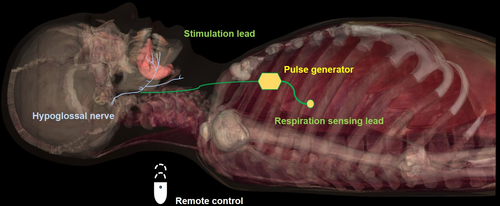
In one of the HN stimulation systems currently available, the stimulation modality is intermittent and synchronized with a respiration-sensing lead implanted in a intercostal space facing the pleura. A piezoelectric sensor detects the respiratory pressure variations and converts them into electric signals. Both stimulating and sensing leads are connected to the pulse generator through a subcutaneous surgical tunnelling (Van de Heyning, 2012). The pulse generator processes the breathing signals received and generates electrical pulses to the hypoglossal nerve via the stimulation lead (Figure 2). A physician's programming system allows to settle the optimal stimulus parameters by telemetry (Vanderveken et al., 2017).
In another neurostimulation system, a multi-electrode cuff is placed proximally around the hypoglossal nerve, stimulating both protrusors and retractors muscles, in order to achieve an increased overall tone of the tongue and prevent upper airways collapse (Friedman et al., 2016).
Direct HN stimulation is usually well tolerated by patients without local discomfort or arousals during sleep. Unlike other OSA common surgical techniques such as pharyngoplasty or robotic surgery of the base of tongue, HN neurostimulation can be considered a functional and multilevel surgical procedure with a physiologic approach since it increases both the retropalatal and retrolingual areas without dissection and/or ablation of pharyngeal or tongue tissues.
2.3 Device activation and titration
After about 1 month from surgical implantation, the device (pulse generator) can be activated and then titrated in several parameters in order to achieve the optimal stimulation setting and patient satisfaction. The electrode configuration and the suitable voltage range of the device are established by an overnight sleep study, which allows a synchronization between stimulation and inspiratory phase of the breathing cycle. A well-regulated respiratory-sensing significantly contributes to successful HNS (Steffen et al., 2020). The majority of selective stimulation systems are programmed in a bipolar configuration that creates a strictly local current loop preventing wider stimulation of adjacent neural structures. The stimulation amplitude should be regulated not too high in order to avoid side effects such as sleep arousals or tissue injuries (Vanderveken et al., 2017). Another advantage of HNS is the opportunity for patients to interact with the device by their self through a remote control adjusting the stimulation parameters according with personal preferences. The remote control is also used to switch on/off the device at the beginning and the end of time in bed, therefore introducing the theme of patient's adherence. Patients need to be instructed to regularly activate the device during sleep in order to achieve optimal treatment efficacy.
Prospective clinical studies showed significantly improved both subjective and objective outcomes, also in the long-term period, and low morbidity of HN neurostimulation in carefully selected OSA patients (Gillespie et al., 2017; Kezirian et al., 2014; Pietzsch et al., 2015; Soose & Gillespie, 2016; Soose et al., 2016; Woodson et al., 2018). Recent studies showed that stimulation intensity and thresholds of the hypoglossal nerve remain stable over years in implanted patients (Zhu et al., 2020). The adverse events reported for this surgical procedure are uncommon and mostly transient. Authors described mild incision-site pain and swelling in submandibular region, temporary tongue weakness and minor discomfort associated with stimulation, often resolved in few days with conservative management or device reprogramming. Severe complications requiring revision surgery and repositioning of the stimulating electrode rarely occur (Certal et al., 2015).
2.4 Limitations and advantages of HNS therapy
Limitations of HNS are the need of surgical implantation under general anaesthesia, MRI incompatibility of the current devices and the unknown factor concerning the long-term adherence and effectiveness of this innovative surgical device that need to be established. Another problem is the high cost of the device that could considerably limit its application in some healthcare systems. Further advancement of this innovative surgical approach will be possible improving technological components of the device, investigating optimal stimulus parameters and applying more specific inclusion criteria for implantation, that is: identification of best responders based on the profile of flow curves during overnight sleep studies (Genta et al., 2017; Mann et al., 2019). Moreover, a standardization of outcome data reported in clinical studies is mandatory to improve future device applications (Dedhia & Woodson, 2018). Further research is needed to carefully assess the long-term performance of the device and patient tolerance.
Compared to other accepted surgical procedures, the main advantage of HNS technique is that it allows the functionally adjustable and potentially reversible activation of upper airway dilatators muscles, without tissue ablation and anatomical definitive modifications, with the possibility of a long-term modulation of the device according to the individual needs and tolerance. Fulfilling strict inclusion criteria HNS can provide a multilevel upper airway improvement in a subset of properly selected OSA patients. Moreover, HNS can be considered as a rescue treatment after previous unsuccessful surgical procedures (Strohl et al., 2016).
An optimal treatment approach for OSA should ideally restore neuromuscular tone of collapsible upper airways sites preserving as much as possible their anatomic structures and sensory-motor functions. Most of traditional surgical procedures imply tissue demolition and/or irreversible anatomic modifications of upper airways involved sites. Another problem of these surgical excisional techniques is the unknown about long-term effectiveness, considering the unavoidable anatomical remodelling overtime especially when soft tissues are operated on.
Most importantly, we must keep in mind that UAS therapy requires a strict multidisciplinary approach from patient evaluation and selection to device programming and follow-up (Doghramji & Boon, 2016). An aspect to take into account is the need to provide to patients and general practitioners an accurate multi-specialist counselling information concerning the strict eligibility criteria to be complied, the requirement of a surgical procedure under general anaesthesia and the potential complications. The multidisciplinary team should also establish an educational program about the expected results, the pre-implantation diagnostic steps and the need of post-operative fitting and training of the device. Since body weight is a crucial issue for the effectiveness of this treatment, it is important to include a close monitoring of this variable.
3 CONCLUSIONS AND FUTURE PERSPECTIVES
Hypoglossal neurostimulation is an innovative and promising surgical technique to treat OSA. The effectiveness and safety of this emerging treatment option have been reported in recent clinical trials. Proper patient selection through a comprehensive multidisciplinary evaluation is crucial to predict a successful implantation. Critical points of HNS are possible damage or malfunctioning of the device requiring surgical replacement, the need to optimize patients selection identifying most appropriate OSA phenotypes to treat and economic sustainability of the procedure. Further advancements should concern technological improvements of the device and adoption of minimally invasive surgical techniques that may further expand the range of clinical application in OSA.
ACKNOWLEDGEMENT
The Authors would like to thank Professor Francesca Boccafoschi, Ph.D and Loredana Marchese of the Laboratory of Human Anatomy, Department of Health Sciences, University of Eastern Piedmont for their valuable contribution in supplying anatomic images.
CONFLICT OF INTEREST
The authors declare no conflict of interest.




