A score model for the continuous grading of early allograft dysfunction severity
We read with great interest the study of Pareja et al.1 that reported a new score characterizing severity of early allograft dysfunction (EAD), the so-called model of early allograft function (MEAF) score. This interesting score, which is calculated from bilirubin, international normalized ratio, and alanine aminotransferase levels observed within the first 3 postoperative days (PODs), is a continuous score from 0 to 10 that reflects the graft function, whereas most of the previous scores, including the definition of EAD reported by Olthoff et al.,2 are only binary. In order to validate the proposed model, we calculated the MEAF score in our population according to the reported formula. Between 2002 and 2014, 1297 liver transplantations were performed in our center with a median follow-up of 41.4 months. Thirty-two (2.5%) patients were retransplanted or died within the first 2 PODs and were therefore excluded from the analysis. Of the 1265 remaining patients, the MEAF score could be calculated in 785 (62.0%) patients.
The median MEAF score value was 4.6, and a significant correlation with graft survival was observed (Fig. 1A). Notwithstanding, the capacity of a MEAF score ≥8 to predict 3-month graft survival was inferior to the presence of EAD (as reported by Olthoff et al.2), as shown by the receiver operating characteristic (ROC) curve (Fig. 1B).
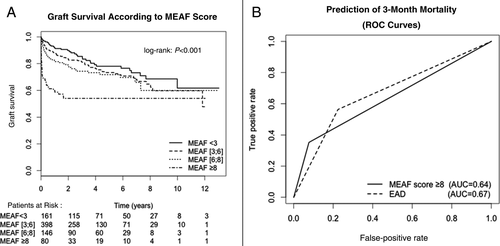
Therefore, our data support the effectiveness of the MEAF score as a grading system of the severity of graft dysfunction. However, it is our opinion that this score has some limitations. First, it cannot be calculated in cases of graft or patient death within the first 2 PODs. This major limitation prevents comparison or analysis of liver transplantation efficiency between subgroups or populations because most patients with primary nonfunction who required early retransplantation were excluded. We suggest that patients for whom the MEAF score could not be calculated because of retransplantation or death should be attributed, by default, the maximum score (ie, 10). Moreover, its formula required a calculator and, therefore, limits its utility in clinical practice. A more simple method of calculation, which could be easily used by physicians, may be useful.
-
Michel Rayar, M.D.1,2,3
-
Giovanni Battista Levi Sandri, M.D.1
-
Caterina Cusumano, M.D.1
-
Nicolas Lombard, M.D.1
-
Mohamed Lakehal, M.D.1
-
Veronique Desfourneaux, M.D.1
-
Bernard Meunier, M.D., Ph.D.1,3
-
Laurent Sulpice, M.D., Ph.D.1,3
-
Karim Boudjema, M.D., Ph.D.1,3
-
1Service de Chirurgie Hépatobiliaire et Digestive
-
Centre Hospitalier Universitaire de Rennes
-
Rennes, France
-
2Centre d'Investigation Clinique
-
U1414
-
INSERM
-
Rennes, France
-
3Faculté de Medicine
-
Université Rennes 1
-
Rennes, France