Effect of angiotensin II and bradykinin inhibition in rat reduced-size liver transplantation
Abstract
This study examined whether angiotensin II (Ang II) blockers [Ang II type I receptor antagonist, Ang II type II receptor antagonist, and angiotensin converting enzyme (ACE) inhibitor] could reduce hepatic injury and improve regeneration in reduced-size orthotopic liver transplantation (ROLT) and whether the beneficial effects of ischemic preconditioning (PC) in ROLT could be explained by changes in Ang II. We show that small liver grafts generated Ang II after ROLT and that this was associated with increased angiotensinogen and ACE messenger RNA expression. Furthermore, inhibition of Ang II did not contribute to PC-induced protection in ROLT. All Ang II blockers reduced hepatic injury, but none of them promoted liver regeneration. Bradykinin (BK) receptor antagonist improved liver regeneration but did not reduce hepatic injury in ROLT. Finally, the combination of Ang II blockers and BK receptor antagonists in ROLT reduced hepatic injury and improved liver regeneration. In conclusion, treatments with either Ang II blockers or BK receptor antagonists cannot, on their own, improve the outcome of ROLT. Although Ang II blockers can reduce hepatic ischemia-reperfusion injury and BK receptor antagonists can promote liver regeneration, neither confers both benefits at the same time. Consequently, it may be of clinical interest to apply both treatments simultaneously. Liver Transpl 15:313–320, 2009. © 2009 AASLD.
Living-related liver transplantation has developed rapidly in recent years in order to alleviate the mortality resulting from the scarcity of suitable deceased donors.1-3 The main limitation of living-related liver transplantation is graft size disparity because reduced-size liver grafts must regenerate rapidly to ensure normal function and patient survival.4-6 Ischemia-reperfusion (I/R), which is inevitable in liver transplantation, reduces liver regeneration after hepatectomy.7-10 Little is known about the mechanisms underlying the dysfunction and failure of reduced-size liver grafts.11
Angiotensin II (Ang II), which is produced via angiotensin converting enzyme (ACE) from angiotensin I, is the main effector of the renin-angiotensin system. It exerts its biological action through its receptor subtypes: Ang II type I receptor (AT1R) and Ang II type II receptor (AT2R).12 Previous studies reported that ACE inhibitors or AT1R antagonists protect against warm hepatic I/R injury12, 13 and that ACE inhibitors show beneficial effects on injury in liver transplantation from non–reduced-size grafts,14 thus suggesting a detrimental role of Ang II in hepatic I/R. ACE inhibitors enhance liver regeneration after partial hepatectomy.15, 16 These observations suggest that Ang II blockers might exert their beneficial effects in situations that require both I/R and liver regeneration, such as reduced-size liver transplantation. ACE inhibitors not only inhibit Ang II generation but also increase bradykinin (BK) levels.17 For instance, the beneficial effects of ACE inhibitors on I/R injury were attributed to BK in an experimental model of I/R without partial hepatectomy,17 and ACE inhibitors increased liver regeneration after partial hepatectomy through activation of BK2 receptors.16 We therefore hypothesized that BK is responsible for the potentially beneficial effects of ACE inhibitors in surgical situations that require both I/R and hepatectomy. Ischemic preconditioning (PC), that is, a short period of ischemia followed by a brief period of reperfusion before a sustained ischemic insult, protected the liver against I/R injury and improved hepatic regeneration in an experimental model of reduced-size liver transplantation,18 but the mechanisms of protection are not well established. A recent study by our group indicated a differential effect of PC on Ang II in an experimental model of warm ischemia, depending on the liver type.19
The aims of the present study were to evaluate the effect of Ang II blockers on hepatic I/R injury and liver regeneration in reduced-size liver transplantation and to determine the effect of PC on Ang II. This could contribute to the development of pharmacological treatments based on modulating Ang II action to improve the quality of the reduced-size liver grafts.
Abbreviations
ACE, angiotensin converting enzyme; ALT, alanine aminotransferase; Ang II, angiotensin II; AST, aspartate aminotransferase; AT1R, angiotensin II type I receptor; AT2R, angiotensin II type II receptor; BK, bradykinin; HGF, hepatocyte growth factor; I/R, ischemia-reperfusion; mRNA, messenger RNA; PC, preconditioning; PCNA, proliferating cell nuclear antigen; PCR, polymerase chain reaction; ROLT, reduced-size orthotopic liver transplantation; TGFβ, transforming growth factor β.
MATERIALS AND METHODS
Experimental Animals
Male Sprague-Dawley rats (200-250 g) were anesthetized with isoflurane. Research procedures complied with European Union regulations for animal experiments (EU guideline 86/609/EEC).
Experimental Design
Protocol 1. Effect of Ang II Blockers on Hepatic I/R Injury and Liver Regeneration in Reduced-Size Orthotopic Liver Transplantation (ROLT) 24 Hours After Transplantation
- 1
Sham (n = 6): Silk ligatures in the right suprarenal vein and hepatic artery.
- 2
ROLT (n = 12, 6 transplants): The liver was reduced by removal of the left lateral lobe and the 2 caudate lobes and was preserved with cold University of Wisconsin solution for 1 hour. ROLT was performed according to Kamada's cuff technique.7 Animals were killed 24 hours after transplantation for sample collection.
- 3
PC (n = 12, 6 transplants): To induce PC, the blood flow of the donor liver was interrupted by placing a clamp at the portal vein and hepatic artery for 10 minutes, and this was followed by reflow for 10 minutes. Livers then underwent ROLT, as described in group 2.7
- 4
ROLT + AT1R antagonist (n = 12, 6 transplants): This was performed just as for group 2, but an AT1R antagonist (losartan) was orally administered (5 mg/kg) 24 hours and 1 hour before the surgical procedure to both the donor and the recipient, respectively.13
- 5
ROLT + AT2R antagonist (n = 12, 6 transplants): This was performed just as for group 2, but an AT2R antagonist (PD123319) was intravenously administered (30 mg/kg) to the donor 25 minutes before excision and to the recipient just after the transplant.19
- 6
ROLT + ACE inhibitor (n = 12, 6 transplants): This was performed just as for group 2, but an ACE inhibitor (captopril) was orally administered (100 mg/kg) 24 hours and 1 hour before the surgical procedure to both the donor and the recipient.13
Protocol 2. Role of BK in the Effects of Ang II Blockers on Hepatic I/R Injury and Liver Regeneration in ROLT 24 Hours After Transplantation
- 7
ROLT + ACE inhibitor + BK receptor antagonist (n = 12, 6 transplants): This was performed just as for group 2, but an ACE inhibitor (captopril) was orally administered (100 mg/kg) 24 hours and 1 hour before the surgical procedure to both the donor and the recipient,13 and a BK2 receptor antagonist (HOE140) was subcutaneously administered (0.5 mg/kg) 1 hour before and during the surgical procedure to the recipient alone.19
- 8
ROLT + BK receptor antagonist (n = 12, 6 transplants): This was performed just as for group 2, but a BK2 receptor antagonist (HOE140) was subcutaneously administered (0.5 mg/kg) 1 hour before and during the surgical procedure to the recipient alone.19
- 9
ROLT + AT1R antagonist + AT2R antagonist + BK receptor antagonist (n = 12, 6 transplants): This was performed just as for group 4, but an AT2R antagonist (PD123319) was intravenously administered (30 mg/kg) to the donor 25 minutes before excision and to the recipient just after the transplant,19 and a BK2 receptor antagonist (HOE140) was subcutaneously administered (0.5 mg/kg) 1 hour before and during the surgical procedure to the recipient alone.19
Control experiments using the vehicle (saline solution) were carried out for each drug.
Sample Collection and Processing
All samples were collected 24 hours after completion of the surgical procedure. Samples for biochemical and molecular biology testing were frozen with dry ice, and samples for histological studies were placed in paraformaldehyde.
Biochemical Determinations
Ang II, BK, transaminase, hepatocyte growth factor (HGF), and transforming growth factor β (TGFβ; total TGFβ and active TGFβ) levels were measured with the same protocol described elsewhere.7, 18, 19 Note that TGFβ is stored in the cells in the latent form, which consists of the mature TGFβ, the TGFβ binding protein, and the latency-associated peptide. When required, the latent form is processed, and the mature TGFβ is released. The mature TGFβ alone is called active TGFβ. Therefore, when we mention total TGFβ, we are referring to the latent and active forms, and when we mention active TGFβ, we are referring to the mature form alone.20
Quantitative Real-Time Polymerase Chain Reaction (PCR) for Angiotensinogen and ACE Messenger RNA (mRNA)
Quantitative real-time PCR analysis was performed with premade Assays-on-Demand TaqMan probes (Rn00593114_m1 for angiotensinogen, Rn00561094_m1 for ACE, and Rn00667869_ml for β-actin; Applied Biosystems). The TaqMan gene expression assay was performed according to the manufacturer's protocol (Applied Biosystems).
Histology and Proliferating Cell Nuclear Antigen (PCNA) Labeling Index
To quantify the severity of hepatic injury, hematoxylin and eosin–stained sections were evaluated by a point-counting method on an ordinal scale.7 Hepatic proliferation was assessed in liver biopsies with immunohistochemistry as previously described.7 Data are expressed as the percentage of mitotic hepatocytes and PCNA-stained hepatocytes (brown nuclei) per total number of hepatocytes in 30 high-power fields. PCNA-positive hepatocytes are those with brown-stained nuclei, and those that have blue-stained nuclei are PCNA-negative hepatocytes.
Statistics
Data are expressed as mean ± standard error. Statistical comparison was performed by variance analysis, and this was followed by the Student-Newman-Keuls test. P < 0.05 was considered significant.
RESULTS
Effect of Ang II Blockers on Hepatic I/R Injury and Liver Regeneration in ROLT 24 Hours After Transplantation
Ang II, Angiotensinogen, and ACE Inhibitors in ROLT 24 Hours After Transplantation
ROLT increased Ang II levels in the liver in comparison with the sham group (Fig. 1A). This increase in hepatic Ang II levels may be due to an increase in angiotensinogen and/or ACE mRNA expression (Fig. 1B). PC did not modify Ang II, angiotensinogen, or ACE levels in comparison with the ROLT group (Fig. 1A,B).
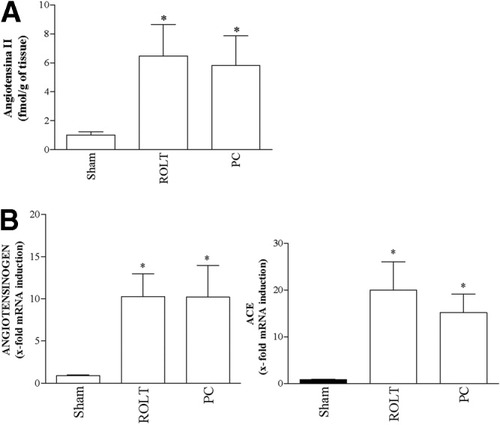
Activation of RAS in ROLT 24 hours after transplantation. (A) Angiotensin II levels and (B) angiotensinogen and ACE mRNA expression were measured in livers from the experimental groups shown in the graph (n = 12 for each group, 6 transplants). All subjects in all groups were included in each measurement. PCR fluorescent signals for angiotensinogen and ACE were standardized to PCR fluorescent signals obtained from an endogenous reference (β-actin). Comparative and relative quantifications of angiotensinogen and ACE gene products normalized to β-actin and a control sham group were calculated with the 2−ΔΔCT method. *P < 0.05 versus sham; +P < 0.05 versus ROLT. Abbreviations: ACE, angiotensin converting enzyme; mRNA, messenger RNA; PC, preconditioning; PCR, polymerase chain reaction; ROLT, reduced-size orthotopic liver transplantation.
Hepatic Injury and Liver Regeneration in ROLT 24 Hours After Reperfusion
All Ang II blockers protected against hepatic injury. As shown in Fig. 2, ROLT + AT1R antagonist, ROLT + AT2R antagonist, and ROLT + ACE inhibitor reduced transaminase levels (Fig. 2A) and grade 3 necrosis (Fig. 2B) in comparison with the ROLT group.
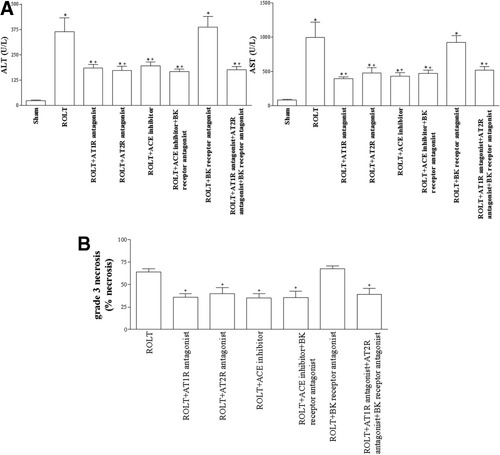
Angiotensin II and BK in hepatic injury associated with ROLT 24 hours after transplantation. (A) Transaminases (ALT and AST) and (B) grade 3 necrosis were analyzed in plasma and livers, respectively, from the experimental groups shown in the graph (n = 12 for each group, 6 transplants). All subjects of all groups were included in each measurement. *P < 0.05 versus sham; +P < 0.05 versus ROLT; °P < 0.05 versus ROLT + ACE inhibitor. Abbreviations: ACE, angiotensin converting enzyme; ALT, alanine aminotransferase; AST, aspartate aminotransferase; AT1R, angiotensin II type I receptor; AT2R, angiotensin II type II receptor; BK, bradykinin; ROLT, reduced-size orthotopic liver transplantation.
None of these Ang II blockers had beneficial effects on liver regeneration. As shown in Fig. 3A, ROLT + AT1R antagonist, ROLT + AT2R antagonist, and ROLT + ACE inhibitor did not significantly affect the PCNA proliferation index in the liver in comparison with the ROLT group. It is well known that hepatocyte proliferation is controlled by both growth-promoting and growth-inhibiting factors, such as HGF and TGFβ, respectively.21, 22 As the PCNA results show, ROLT + AT1R antagonist, ROLT + AT2R antagonist, and ROLT + ACE inhibitor resulted in HGF and active TGFβ levels that were similar to those of the ROLT group (Fig. 3B). Total hepatic TGFβ (latent + active) levels were similar in all groups (data not shown).
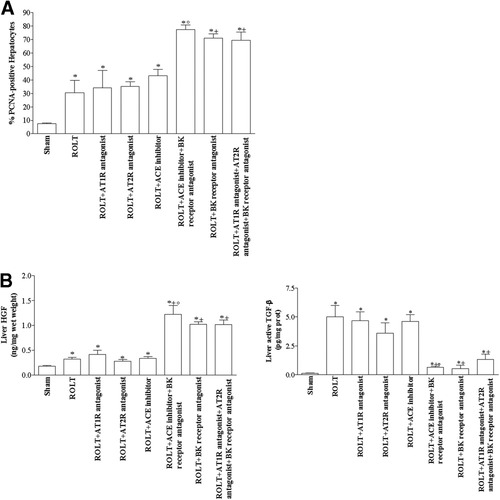
Angiotensin II and BK in hepatic regeneration in ROLT 24 hours after transplantation. (A) The percentage of PCNA-positive hepatocytes and (B) HGF and active TGFβ levels were analyzed in livers from the experimental groups shown in the graph (n = 12 for each group, 6 transplants). All subjects in all groups were included in each measurement. *P < 0.05 versus sham; +P < 0.05 versus ROLT; °P < 0.05 versus ROLT + ACE inhibitor. Abbreviations: ACE, angiotensin converting enzyme; AT1R, angiotensin II type I receptor; AT2R, angiotensin II type II receptor; BK, bradykinin; HGF, hepatocyte growth factor; PCNA, proliferating cell nuclear antigen; ROLT, reduced-size orthotopic liver transplantation; TGFβ, transforming growth factor β.
Role of BK in the Beneficial Effects of ACE Inhibitors on Liver I/R Injury and Hepatic Regeneration in ROLT 24 Hours After Transplantation
Investigations were carried out to determine whether the beneficial effects of the ACE inhibitor on hepatic injury were due to the reduction in Ang II generation or increased BK levels. As expected, ROLT + ACE inhibitor and ROLT + ACE inhibitor + BK receptor antagonist increased BK levels in comparison with the ROLT group, whereas BK levels in the other treatments were unmodified (Fig. 4). As shown in Fig. 2, ROLT + ACE inhibitor + BK receptor antagonist resulted in hepatic injury parameters that were similar to those of the ROLT + ACE inhibitor group. Moreover, the histological study of the liver in the ROLT group revealed multifocal areas of coagulative necrosis randomly distributed throughout the hepatic parenchyma (Fig. 5A). In contrast, fewer and smaller areas of hepatocyte necrosis were observed in the ROLT + ACE inhibitor and ROLT + ACE inhibitor + BK receptor antagonist groups (Fig. 5B,C, respectively). However, ROLT + ACE inhibitor + BK receptor antagonist increased the proliferation index (Fig. 3) and the number of PCNA-positive hepatocytes (Figs. 5E,F) in comparison with the ROLT + ACE inhibitor group. This was associated with increased HGF levels and reduced TGFβ levels (Fig. 3). These results indicate that BK does not play a role in hepatic injury but is involved in liver regeneration. Moreover, ROLT + BK receptor antagonist resulted in parameters of hepatic injury that were similar to those of the ROLT group (Fig. 2) but improved liver regeneration. In other words, ROLT + BK receptor antagonist increased the PCNA index and HGF levels and reduced TGFβ levels in comparison with the ROLT group (Fig. 3). Finally, as we have previously shown, Ang II receptor antagonists improved only hepatic injury, but ROLT + AT1R antagonist + AT2R antagonist + BK receptor antagonist resulted in both a reduction of hepatic injury and an improvement of liver regeneration (Figs. 2 and 3).
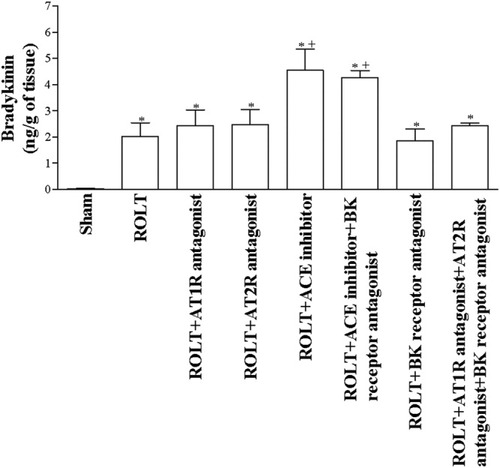
BK levels in ROLT 24 hours after transplantation. BK levels were analyzed in livers from the experimental groups shown in the graph (n = 12 for each group, 6 transplants). All subjects in all groups were included in each measurement. *P < 0.05 versus sham; +P < 0.05 versus ROLT; °P < 0.05 versus ROLT + ACE inhibitor. Abbreviations: ACE, angiotensin converting enzyme; AT1R, angiotensin II type I receptor; AT2R, angiotensin II type II receptor; BK, bradykinin; ROLT, reduced-size orthotopic liver transplantation.
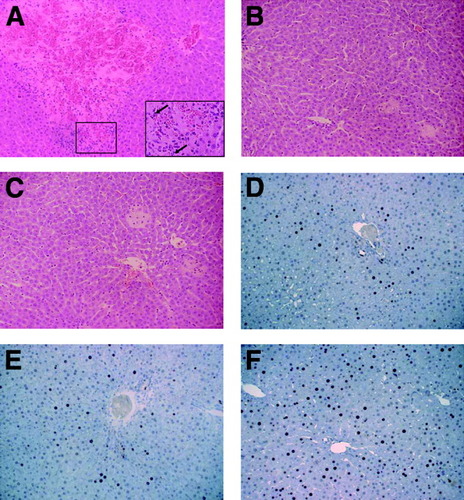
Histological analysis of the liver. (A-C) Histological lesions and (D-F) immunocytochemical staining of proliferating cell nuclear antigen–positive hepatocytes. (A) ROLT: extensive and multifocal areas of coagulative necrosis of hepatocytes with hemorrhage and neutrophil infiltration. (B) ROLT + ACE inhibitor and (C) ROLT + ACE inhibitor + BK receptor antagonist: focal and small areas of hepatocyte necrosis with neutrophil infiltration [hematoxylin and eosin; original magnification, ×240 (original magnification, ×720, for the inset in part A)]. (D) ROLT and (E) ROLT + ACE inhibitor: lower positive cell number versus (F) ROLT + ACE inhibitor + BK receptor antagonist (original magnification, ×500). Abbreviations: ACE, angiotensin converting enzyme; BK, bradykinin; ROLT, reduced-size orthotopic liver transplantation.
DISCUSSION
Ang II is believed to be involved in the pathogenesis of end-organ damage, including stroke, renal disease, and myocardial infarction, in both clinical and experimental situations.23-26 Studies of the heart have indicated that AT1R and AT2R generate opposite effects,27 but this does not appear to occur in the liver. In fact, the beneficial effects of AT1R and AT2R on hepatic I/R injury have been reported in models of warm I/R and liver transplantation of non–reduced-size grafts.12-14 Here we show Ang II generation in ROLT, which was associated with increased angiotensinogen and ACE mRNA expression. In addition, our results indicated that the use of Ang II blockers, such as AT1R antagonists, AT2R antagonists, and ACE inhibitors, could be a promising strategy for reducing hepatic injury associated with ROLT. The current study strongly suggests that Ang II blockers reduce hepatic injury. Further studies will be required to elucidate the mechanisms by which Ang II blockers improve hepatic injury after ROLT. One of the mechanisms through which Ang II blockers diminish hepatic injury after ROLT may be alteration of the hepatic microcirculation. Indeed, we know from the literature that the inhibition of AT1R improves hepatic microcirculation in a model of warm I/R in dogs.12 Moreover, in a model of human hypertension, Ang II blockers ameliorated cardiac microcirculation.28
Different results have been reported for the effect of PC on Ang II.19, 29-31 Some studies of the heart indicate that PC inhibits the biological actions of Ang II,29 whereas others studies show that Ang II contributes to the benefits of PC.30, 31 A recent study by our group indicated a differential effect of PC on Ang II in an experimental model of warm ischemia, depending on the liver type: PC reduced Ang II generation in steatotic livers but not in nonsteatotic ones.19 Previous studies by our group demonstrated that PC exerted beneficial effects on I/R injury and liver regeneration in ROLT.7 Our results in the present study indicated that PC did not modify the expression of enzymes or precursors capable of generating Ang II. However, the lack of changes of expression of the RAS components does not rule out posttranscriptional regulation. However, what we have seen in the present study is that the beneficial effects of PC are not due to differences in Ang II generation.
The beneficial effects of ACE inhibitors on liver regeneration after partial hepatectomy have been described previously.15, 16 Studies have reported that ACE inhibitors increase renal HGF mRNA and cardiac HGF concentrations in experimentally hypertensive rats32 and that Ang II down-regulates HGF production in mesangial cells in a cultured model.33 HGF and TGFβ are the most common markers of liver regeneration used in models of rat liver regeneration.18 HGF is the most potent of liver mitogens.34 On the other hand, TGFβ inhibits hepatocellular DNA synthesis both in culture35, 36 and in vivo.37 It has been suggested that TGFβ may be the principal counter regulator of hepatocyte proliferation during regeneration.38 Our results indicated that neither ACE inhibitors nor other Ang II blockers were capable of inducing hepatic regeneration in ROLT; ACE inhibitors did not modify either the PCNA or growth factor (HGF and TGFβ) results observed in the ROLT group without any treatment.
Here we have shown that BK does not play a role in hepatic injury associated with ROLT because ROLT + BK receptor antagonist did not reduce hepatic injury. It did, however, improve liver regeneration in comparison with the results recorded for the ROLT group. This improvement correlates with the increase in PCNA-positive hepatocytes, the increase in HGF levels, and the decrease in TGFβ levels observed in this group in comparison with the ROLT group without any treatment. On the other hand, all Ang II blockers had beneficial effects on hepatic injury but not on liver regeneration. ROLT + ACE inhibitor, ROLT + AT1R antagonist, and ROLT + AT2R antagonist all reduced the biochemical and histological parameters of hepatic injury but did not affect the hepatic regeneration parameters. Thus, the concomitant inhibition of BK and Ang II action could help to reduce hepatic injury and promote liver regeneration in ROLT because our results indicated that the combination of Ang II blockers and BK receptor antagonists had beneficial effects on both. In terms of good clinical outcomes, treatment with either Ang II blockers or BK2 receptors antagonists alone cannot sufficiently improve the outcome of reduced-size liver transplantation because although Ang II blockers can reduce hepatic I/R injury and BK receptor antagonists can promote liver regeneration, neither one does both at the same time. Consequently, it may be of clinical interest to administer both the Ang II blockers and the BK receptor antagonists together.
ACE inhibitors are widely used in clinical practice.39, 40 However, hepatotoxicity and cholestatic liver diseases have been reported under ACE inhibition.41, 42 Taking these observations into account, along with the fact that AT1R antagonists and AT2R antagonists were as effective as ACE inhibitors in terms of hepatic injury, we propose that the most suitable strategy to be applied in ROLT to reduce hepatic injury and increase liver regeneration is the combination of Ang II receptor antagonists together with BK receptor antagonists.
Acknowledgements
We are grateful to Robin Rycroft at the Language Advisory Service of the University of Barcelona for revising the English text. The authors thank Emma Puig-Oriol and Llorenç Quintó (Epidemiology and Biostatistics Unit, University of Barcelona) for their help with the statistical analyses. Carmen Peralta participates in the Programa de Esatabilització d'Investigadors de la Direcció d'Estratègia i Coordinació del Departament de Salut de la Generalitat de Catalunya.




