Biliary reconstruction for infantile living donor liver transplantation: Roux-en-Y hepaticojejunostomy or duct-to-duct choledochocholedochostomy?
Abstract
Hepaticojejunostomy is a standard biliary reconstruction method for infantile living donor liver transplantation (LDLT), but choledochocholedochostomy for infants is not generally accepted yet. Ten pediatric recipients weighing no more than 10 kg underwent duct-to-duct choledochocholedochostomy (DD) for biliary reconstruction for LDLT. Patients were followed up for a median period of 26.8 months (range: 4.0–79.0 months). The incidence of posttransplant biliary complications for DD was compared with that for Roux-en-Y hepaticojejunostomy (RY). No DD patients and 1 RY patient (5%) developed biliary leakage (P > 0.05), and biliary stricture occurred in 1 DD patient (10%) and none of the RY patients (P > 0.05); none of the DD patients and 5 RY patients (25%) suffered from uncomplicated cholangitis after LDLT (P > 0.05), and 1 DD patient (10%) and 2 RY patients (10%) died of causes unrelated to biliary complications. In conclusion, both hepaticojejunostomy and choledochocholedochostomy resulted in satisfactory outcome in terms of biliary complications, including leakage and stricture, for recipients weighing no more than 10 kg. Liver Transpl 14:1761–1765, 2008. © 2008 AASLD.
Liver transplantation is an established curative therapy for children with end-stage chronic liver disease or acute liver failure. Outcomes following liver transplantation for children have significantly improved over the past 2 decades because of advances in surgical procedures, preservation technology, immunosuppressants, and perioperative management.1
However, despite refinements in surgical techniques for living donor liver transplantation (LDLT), biliary complications are still associated with significant morbidity and mortality.2 Duct-to-duct choledochocholedochostomy (DD) and Roux-en-Y hepaticojejunostomy (RY) are now generally accepted procedures for biliary reconstruction in adult-to-adult LDLT.3, 4 However, RY has remained the standard method for pediatric LDLT because of the dominance of biliary atresia and technical difficulties related to the size and fragility of recipients' bile ducts. Only a few reports can be found in the literature on pediatric LDLT using DD,5, 6 and to the best of our knowledge, there have been no studies focused on DD for infantile LDLT. This is therefore the first report to investigate the viability of DD in LDLT for infants weighing no more than 10 kg.
Abbreviations
CIT, cold ischemic time; DD, duct-to-duct choledochocholedochostomy; GRWR, graft-to-recipient weight ratio; LDLT, living donor liver transplantation; RY, Roux-en-Y hepaticojejunostomy; WIT, warm ischemic time.
PATIENTS AND METHODS
Patients
Between February 2001 and January 2008, 57 pediatric patients (less than 15 years old) underwent 60 LDLTs at Kumamoto University Hospital. Thirty-four of these pediatric recipients (59.6%) weighed no more than 10 kg at the time of LDLT. Ten of them who were treated with DD and survived more than 1 month after LDLT were included in this study. Their demographic data are shown in Table 1. The subjects were followed up until May 2008 for a median period of 26.8 months (range: 4.0–79.0 months). Three ABO-incompatible transplants were included in this group.
| DD (n = 10) | |
|---|---|
| Age (months) | 12.2 ± 9.9 (3–33) |
| Sex (male/female) | 7/3 |
| Body weight (kg) | 7.3 ± 2.4 (3.3–10) |
| Diagnosis | |
| Fulminant hepatic failure | 4 |
| Byler | 2 |
| Methylmalonic acidemia | 2 |
| Cryptogenic cirrhosis | 1 |
| Hepatoblastoma | 1 |
| Blood combination | |
| Identical | 7 |
| Compatible | 0 |
| Incompatible | 3 |
| Follow-up (months) | 26.8 ± 27.5 (4.0–79.0) |
- Abbreviation: DD, duct-to-duct choledochocholedochostomy.
Operations
Operative details are summarized in Table 2. All patients received grafts from either their mother or father. In principle, the left-lateral segment was used as the graft, and the reduction of this graft was considered when the graft-to-recipient weight ratio estimated by preoperative computed tomography volumetry was larger than 4%.
| DD (n = 10) | |
|---|---|
| Operation time (minutes) | 494.2 ± 71.8 (401–600) |
| CIT (minutes) | 56.3 ± 40.5 (19–147) |
| WIT (minutes) | 40.0 ± 6.7 (33–52) |
| Blood loss (g) | 250.6 ± 259.9 (35–915) |
| Graft type | |
| Lateral | 5 |
| Monosegment | 2 |
| Reduced monosegment | 3 |
| Graft weight (g) | 221.8 ± 46.4 (115–265) |
| GRWR (%) | 3.2 ± 0.9 (2.2–5.2) |
- Abbreviations: CIT, cold ischemic time; DD, duct-to-duct choledochocholedochostomy; GRWR, graft-to-recipient weight ratio; WIT, warm ischemic time.
Every donor candidate underwent preoperative drip infusion cholecystocholangiography/computed tomography. Intraoperative cholangiography was performed throughout the hilar dissection for better visualization of the biliary anatomy. Two small vascular clips were placed on the left hepatic duct around 5 mm distant from the bifurcation to facilitate identification of the optimal site for transection of the left hepatic duct. The left hepatic duct was sharply transected at the planned site after it was determined that there were no right posterior branches originating from the more proximal left hepatic duct. Hepatic resection of the donor was performed with an ultrasonic dissector and bipolar electrical cautery without inflow occlusion. One of the left-lateral segments, the monosegment or the reduced monosegment, was used as the graft; the size was chosen according to the graft-to-recipient weight ratio estimation. The graft liver was removed after vascular clamping, and this was followed by in situ perfusion with University of Wisconsin solution (ViaSpan, Bristol-Myers Squibb Co., New York, NY) or histidine-tryptophan-ketoglutarate solution (Custodiol, Odyssey Pharmaceuticals, Inc., East Hanover, NJ) through the left portal vein.
In recipients with an intact extrahepatic biliary tract, the bile duct was usually divided above the bifurcation. Pericholangic connective tissue was preserved as much as possible to maintain an adequate blood supply to the bile duct. However, adequate mobilization was also performed to reduce the tension at the anastomotic site. The liver graft was implanted in an orthotopic manner following total hepatectomy, with the inferior vena cava in the recipient being preserved. The hepatic artery was then anastomosed with a microsurgical technique. Before biliary reconstruction, the blood supply of the stump of the recipient's bile duct was confirmed by monitoring of the bleeding at the stump. Minute interrupted suturing was performed with 6-0 absorbable sutures (polydioxanone; Ethicon, Somerville, NJ). After completion of the suture of the posterior row, an external transanastomotic stent tube (4-French pancreatic duct tube; Sumitomo Bakelite, Tokyo, Japan) was placed and anchored with an absorbable stitch at the edge of the anterior wall of the graft hepatic duct. The tube was then passed through the remnant cystic duct or the common bile duct. After completion of the anterior wall, surrounding tissue of the recipient's bile duct wall was anchored to the hilar plate of the graft liver with 4 to 6 absorbable stitches in order to reduce the tension of the anastomosis (Fig. 1).
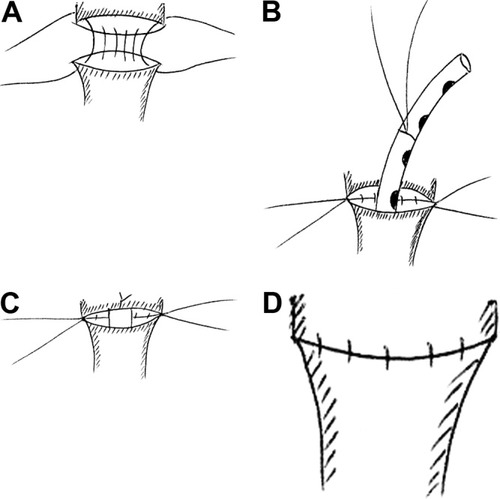
(A) A stay suture was placed at both ends of the anastomotic orifice. Minute interrupted suturing of the posterior row was performed. (B) An external transanastomotic stent tube was then passed through the remnant cystic duct or the common bile duct. (C) The stent was inserted into the intrahepatic duct and anchored with an absorbable stitch at the anterior wall of the stump of the graft hepatic duct. (D) Finally, the interrupted suture of the anterior wall was completed.
Immunosuppression
Immunosuppression was performed with tacrolimus and low-dose steroids. Target trough levels of tacrolimus were 12 to 15 ng/mL for the first 2 weeks, approximately 10 to 12 ng/mL for the following 2 weeks, and 5 to 10 ng/mL thereafter. Steroid treatment was initiated with an injection of 10 mg/kg methylprednisolone prior to graft reperfusion during surgery, and it was usually tapered off until complete withdrawal around 3 to 6 months after the transplant.
Study Design and Outcome Parameters
Medical records of the LDLTs of the 10 patients who weighed no more than 10 kg and were treated with DD were reviewed, and the perioperative characteristics and the method of biliary reconstruction were examined. Posttransplant biliary complications in the DD recipients were compared with those in the 20 recipients who weighed no more than 10 kg and were treated with RY.
Biliary leakage was diagnosed by cholangiography using the external stent tube when a yellowish discharge with a higher bilirubin level than that in serum was obtained from the abdominal drain. Postoperative cholangiography using the external stent tube was routinely carried out for an early diagnosis of any biliary complication 1 month after LDLT. When liver function test results suggested biliary stricture and/or ultrasonography and computed tomography scanning showed a dilated bile duct, either percutaneous transhepatic cholangiography or endoscopic retrograde cholangiopancreatography was conducted. Posttransplant uncomplicated cholangitis was defined as fever accompanied by an elevation of the serum level of C reactive protein and/or leukocytosis in addition to the liver function test showing a cholestatic pattern without echographic evidence of biliary tract dilatation.7
Statistics
Data were expressed as means ± standard deviation. Fisher's exact test, unpaired t tests, and the log-rank test were used for statistical analysis. P values less than 0.05 were regarded as significant.
RESULTS
There were no multiple bile ducts of the graft liver. Figure 2 shows the biliary reconstruction in DD. Three different types of orifices of the recipient's bile duct were used. Branch corresponded to the anastomosis of the graft hepatic duct to the bifurcation of the right and left branches of the recipient's hepatic duct; it was most frequently employed to reconstruct the biliary tract in small infants. Common hepatic duct (CHD) involved the end-to-end anastomosis between the graft hepatic duct and the recipient common hepatic duct, and left hepatic duct (LHD) was the anastomosis between the graft hepatic duct and the recipient left hepatic duct. CHD was used in 4 recipients, and LHD was used in only 1 recipient.
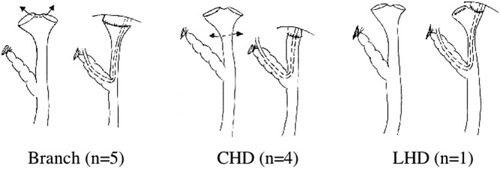
Three types of orifices of the bile duct were prepared for the duct-to-duct choledochocholedochostomy recipients. Branch was used in 5 cases, CHD was used in 4 cases, and LHD was used in 1 case.
The biliary stent tube was left in place for a median period of 121.8 (94–155) days even if the postoperative cholangiogram showed no evidence of biliary leakage or stricture during postoperative month 1. Meanwhile, the stent tube in the RY group was pulled out on mean postoperative day 114.5 (86–175; versus DD, P > 0.05).
The occurrence of biliary complications is shown in Table 3. Leakage developed in only 1 RY patient, who produced a peritoneal discharge with a high amylase level (11,392 U/L) and a high total bilirubin level (49.4 mg/dL) on postoperative day 15, and a diversion enterostomy of the Roux-en-Y limb was made to isolate the biliary anastomosis from the regurgitation of intestinal juice. Biliary stricture occurred in only 1 DD patient. A cholangiogram performed in postoperative month 6 showed complete obstruction of the graft bile duct proximal to the biliary anastomosis, and the patient underwent revision of hepaticojejunostomy 250 days after LDLT following percutaneous transhepatic cholangiodrainage. The area of fibrotic obstruction of the graft hepatic duct was located proximally to the anastomosis in the graft liver, and it seemed to be caused by poor blood supply to the graft hepatic duct. This patient is doing well 1.3 years after LDLT. Five of the RY patients suffered 10 episodes of uncomplicated cholangitis lasting from 4 to 27 months after LDLT, but none of the DD patients did (P > 0.05). The 5 RY cases were all successfully treated with antibiotics, but 2 of them suffered such episodes more than twice.
| DD (n = 10) | RY (n = 20) | P | |
|---|---|---|---|
| Leakage | 0 | 1 (5%) | 0.472 |
| Stricture | 1 (10%) | 0 | 0.1503 |
| Uncomplicated cholangitis | 0 | 5 (25%) | 0.0833 |
- Abbreviations: DD, duct-to-duct choledochocholedochostomy; RY, Roux-en-Y hepaticojcjunostomy.
One DD patient died of recurrence of hepatoblastoma, and 2 RY patients died of respiratory failure following severe pneumonia. Biliary complications were not related to the mortality of the infants weighing no more than 10 kg in this series.
DISCUSSION
We employed DD for biliary reconstruction, even for pediatric LDLT in principle, when the recipient's common bile duct was available. We have previously reported the results of duct-to-duct reconstruction for LDLT for pediatric patients, including infants.8 The present report is a small (but so far the largest) retrospective study of the viability of the duct-to-duct technique for infantile LDLT. Our findings demonstrate that DD can produce a satisfactory outcome comparable to that for hepaticojejunostomy in biliary reconstruction.
We employed 3 DD types for small infants. We believe that using the bifurcation of the right and left branches of the recipient's hepatic duct for biliary anastomosis is the best method to facilitate acceptance of the larger graft bile duct of the adult donor. The common hepatic duct was chosen as the anastomotic orifice when the caliber of the graft left hepatic duct was relatively small. When the graft hepatic duct was smaller and/or the anastomosis to the recipient's common hepatic duct might generate much tension, the left hepatic duct was chosen as the recipient's anastomotic site. The small caliber of the pediatric bile duct did not interfere with our performance of duct-to-duct anastomosis.
An external biliary stent tube was placed in all pediatric recipients enrolled in this study. Use of the anastomotic stent is somewhat controversial. Marcos et al.9 reported that biliary complications occurred in 33% of patients without stents versus 4% of those with stents for adult-to-adult LDLT with RY. Furthermore, the incidence of biliary complications in duct-to-duct anastomosis has also been reported to be significantly lower with a stent tube used as a splint for the anastomosis than with only a drainage tube without stenting.10 On the other hand, Lin et al.11 reported that whether or not a T-tube was used for choledochocholedochostomy after liver transplantation had no effect on biliary complications. Because the stent tube sometimes occupies the small lumen of the infant hepatic duct, some infants who underwent DD suffered from acholic stool until the tube was pulled out. However, liver function test results for every case in our series showed excellent recovery from LDLT (data not shown).
The reported incidence of biliary complications, including leakage and stricture, varies from 14% to 38% for pediatric liver transplantation.12-14 Biliary reconstruction procedures employed by us produced a good outcome for infantile LDLT, with an incidence of biliary complications of 10%. The low incidence of anastomotic leakage may be partially due to anchoring the recipient's bile duct to the graft hilar plate to reduce the tension on the anastomosis. The extrahepatic ducts are surrounded by a vascular plexus, which is composed of branches arising directly from the right and left hepatic arteries.15 ABO-incompatible liver transplantation has an increased risk of hepatic artery thrombosis and diffuse biliary stricture caused by a primary antibody-mediated injury to the bile duct epithelium or ischemia following endothelial injury of the hepatic artery.16 Three infants received ABO-incompatible grafts in the present study. However, LDLT can be carried out with relative safety during infancy before the onset of isohemagglutinin production.17 None of the recipients in our study weighing no more than 10 kg developed hepatic artery complications. Also, postoperative cholangiogram using the external stent tube showed no abnormal findings such as diffuse biliary strictures in the infantile recipients, although it was not after a long term. A stricture of the graft hepatic duct localized proximally to the anastomotic site developed in only 1 DD patient who had received an ABO-identical graft because shortening of the donor extrahepatic duct segment seemed to improve circulatory status around the biliary anastomosis. Moreover, a special feature of our technique, that is, harvesting the lateral segment graft while leaving as much peribiliary tissue as possible on the stump of the graft hepatic duct, may have contributed to the low incidence of biliary complications for infantile LDLT using not only hepaticojejunostomy but also DD. However, additional and longer follow-up is needed to evaluate late biliary complications, including biliary stricture, in DD.
Cholangitis is a common complication in the early period following liver transplantation and sometimes recurs even years after surgery.18, 19 In the case of hepaticojejunostomy, the sphincteric mechanism that prevents reflux of intestinal contents is bypassed, and the reflux of intestinal contents is an important pathogenic mechanism.20, 21 In fact, posttransplant cholangitis was usual in our RY cases, although it was successfully treated with antibiotics. On the other hand, there were no episodes of cholangitis for DD with the sphincteric mechanism kept intact.
In conclusion, our surgical technique using DD in recipients weighing no more than 10 kg produced excellent outcomes with a low incidence of biliary complications, including leakage and stricture. DD may become the standard method for biliary reconstruction even in infantile LDLT in the future if the recipient's common bile duct is available.




