Quality of life up to 30 years following liver transplantation†
See Editorial on Page 1404
Abstract
Liver transplantation provides a return to a satisfactory quality of life (QOL) for the majority of patients in the short to medium term (first 5 years), but there is very little information on the QOL in the longer term and the factors influencing it. We therefore undertook a single-center cross-sectional analysis to determine QOL in patients 10 or more years after liver transplantation. All liver transplant recipients who were followed up at the Cambridge Transplant Unit for 10 or more years (transplanted between 1968 and 1994) and resident in the United Kingdom were asked to complete by post the Short Form 36 version 2 and the Ferrans and Powers questionnaires to evaluate their QOL. Univariate and multivariate analysis were performed to assess the relationship between a range of clinical parameters and QOL. One hundred two patients were invited to participate, and 61 (59.8%) responded. Overall, the patients reported a satisfactory QOL. On the Ferrans and Powers questionnaire, the patients had a mean Quality of Life Index score of 24.5. Factors associated with reduced physical functioning were age > 50 years at transplantation, female gender, and recurrence of the primary liver disease. On the Short Form 36 version 2 questionnaire, recipients had reduced physical functioning but normal mental health parameters in comparison with the normal population. Age > 60 years at the time of survey, female gender, and posttransplant complications were associated with reduced physical functioning. In conclusion, patients 10 or more years after liver transplantation generally have a good QOL, although physical functioning is reduced. Addressing issues such as recurrent disease and posttransplant problems such as osteoporosis may help to improve long-term QOL. Liver Transpl 14:1473–1479, 2008. © 2008 AASLD.
Liver transplantation is now a well-established treatment for selected patients with end-stage liver disease, and the reported 5-year survival rates are in the region of 73%.1 Nevertheless, liver transplantation remains a major operative procedure carrying a perioperative mortality rate of around 8% and commonly gives rise to postoperative complications requiring further hospitalization.1 Many patients requiring liver transplantation suffer a long period of progressive ill health prior to transplantation, and most are very unwell at the time of transplant. Full recovery from the transplant procedure and associated complications may take several months, and all liver transplant recipients require lifelong treatment with immunosuppressive agents and regular follow-up to detect and manage long-term health problems.
Over the past decade, as outcome following liver transplantation in terms of patient and graft survival has steadily improved, attention has focused increasingly on the importance of restoring quality of life (QOL) in transplant recipients. Studies on short-term QOL following liver transplantation have reported gratifying results, and most but not all patients show an improvement in QOL compared to that prior to transplantation.1-4 There is, however, little information on the long-term QOL in patients after liver transplantation. This report presents the findings of a single-center cross-sectional study of QOL in patients more than 10 years after successful liver transplantation. Our aim was to determine the QOL in long-term liver transplant recipients and to identify potential factors that might be associated with impaired QOL.
Abbreviations
BP, bodily pain; CMV, cytomegalovirus; CNI, calcineurin inhibitor; FAMSUB, family subclass; GH, general health; HF, health functioning; HFSUB, health functioning subclass; MCS, mental cumulative score; MH, mental health; NBS, norm-based score; NODAT, new onset diabetes after transplantation; NS, not significant; PCS, physical cumulative score; PF, physical functioning; PSPSUB, psychological/spiritual subclass; QLI, Quality of Life Index; QOL, quality of life; RE, role emotional; RP, role physical; SF, social functioning; SF 36v2, Short Form 36 version 2; SOCSUB, social subclass; VT, vitality.
PATIENTS AND METHODS
All patients who are currently alive and were followed up for more than 10 years after a liver transplant carried out between April 1968 and March 1994 in Cambridge were selected for inclusion in the study. These included both primary transplants and retransplants. Patients not resident in the United Kingdom and those lost to follow-up were excluded. The study was conducted with the approval of the Cambridge Local Research Ethics Committee, and informed consent was obtained from all those who participated in the study.
The Ferrans and Powers questionnaire,5 developed specifically for evaluating liver transplant recipients, and the UK version of Short Form 36 version 2 (SF 36v2) were used. The questionnaires were sent by post. Scoring of the completed responses was carried out as described by Ferrans and Powers in the documentation accompanying the questionnaire and as described in the manuals for SF 36v2. The UK population norms used were those described by Jenkinson et al.6 Nonresponders to the initial approach were followed up with a single reminder letter. Encryption of data, anonymous questionnaires, destruction of sensitive information after analysis, and secure storage of records were used to ensure appropriate data protection.
Relevant clinical data were collected retrospectively from a review of case records. This included demographic details, clinical indications for transplantation, time since transplantation, reoperation, retransplantation, donor age, pretransplant creatinine, day 1 creatinine, creatinine at last follow-up, cytomegalovirus (CMV) mismatch, CMV reactivation, pretransplant hepatitis B surface antigen status, hepatitis C virus status, type and duration of immunosuppression, calcineurin toxicity, and the cumulative steroid index (defined as the time taken to achieve a steroid dose of 5 mg in months multiplied by 5). In addition, information regarding posttransplant vascular complications, biliary complications, early acute rejection, number of episodes of acute rejection, steroid-resistant rejection, chronic rejection, posttransplant malignancy, inferior vena caval stenosis, presence of severe osteoporosis, new onset diabetes after transplantation,7 posttransplant hyperlipidemia, and recurrent liver disease were also collected. The study did not include data on Child-Pugh or Model for End-Stage Liver Disease scoring at the time of listing or transplantation. Severe osteoporosis was defined as severe bone pain (with or without associated bone fractures) and treatment for osteoporosis.8 As this was a retrospective study spanning several decades, information on T/Z values and bone densitometry was not uniformly available throughout the entire study period.
Nephrotoxicity was defined as documented evidence of raised or rising serum creatinine together with treatment [reduction of calcineurin inhibitors (CNIs) or conversion to an alternative agent] for nephrotoxicity or was confirmed on renal histology. CMV reactivation was defined as proven CMV disease or detected CMV viral counts for which antiviral therapy had been initiated. (A standard cutoff value for polymerase chain reaction viral titers was not used because of the high variability in repeated cycles of the same sample due to the inherent technical issue of amplification and because it was not uniformly available throughout the whole study period).
CNI toxicity has been defined as nephrotoxicity presumed to be due to CNI confirmed by histology or responding to substitution by alternative immunosuppressive agents. These regimens have been azathioprine-prednisolone in the initial experience and azathioprine-prednisolone, mycophenolate mofetil–prednisolone, or sirolimus in the later period. This group of drugs was considered one entity again to prevent chance effects due to a relatively small sample size with inadequate power to demonstrate a difference between mycophenolate mofetil, sirolimus, or azathioprine-prednisolone. Recurrent disease was defined as recurrence of symptoms of pretransplant disease with histological evidence of recurrent disease with or without the requirement of retransplantation. Vascular complications included the following 5 subgroups: arterial thrombosis, venous thrombosis, arterial stenosis requiring revision or dilatation, venous stenosis requiring intervention, and arterial aneurysms demonstrated on angiography. Although the clinical presentation of these could greatly vary because of the very small numbers, all of the above were combined together as a single group for the purpose of statistical analysis. Biliary complications were deemed to be present when patients were confirmed to have biliary leaks or strictures on imaging (endoscopic retrograde cholangiopancreatography or magnetic resonance cholangiopancreatography), intra-abdominal collections containing bile, or a biliary leak at laparotomy. Chronic rejection was deemed to be present only when ductopenic rejection was confirmed on histology. All posttransplant malignancies (including skin cancers, colonic cancers, and posttransplant lymphoproliferative disease), with the exception of recurrent hepatocellular cancer, have been included in the study. De novo posttransplant diabetes requiring initiation of antidiabetic drugs in a patient not known previously to be glucose-intolerant was thought to represent diabetes (new onset diabetes after transplantation).
An exploratory univariate analysis was initially performed to assess the possible impact of various clinical factors on QOL and QOL subclasses. The factors tested were age > 60 years at last follow-up, age > 50 years at transplantation, gender, posttransplant complications, severe osteoporosis, rejection, malignancy, cause of liver disease, recidivism, retransplantation, hepatic artery thrombosis, reoperations, CMV reactivation, rejection episodes, use of CNIs, CNI toxicity, use of steroids, and reoperations. Age thresholds were determined with scatter plots.
On the basis of findings from the initial univariate analysis, a principal component analysis was then undertaken with binary logistic regression to evaluate the impact on physical functioning of gender, age more than or less than 60 years, reoperation, recurrent disease, posttransplant complications, and severe osteoporosis.
Statistical Analysis
The Mann-Whitney U Test and the Kruskall-Wallis test were used to assess nonparametric data, and Fisher's exact test was performed with the Statistical Package for Social Sciences version 12 (SPSS, Inc., Chicago, IL.) to test the effects of various clinical variables. Spearman's correlation was used to test the correlation between the 2 questionnaires for the study population. Binary logistic regression was undertaken after data transformation. Statistical significance was at the 95% confidence interval, and all tests of significance were 2-tailed unless stated otherwise. A P value of <0.05 was used to determine statistical significance.
RESULTS
Some 683 patients underwent a liver transplant procedure (either primary or retransplant) between April 1968 and March 1994 in Cambridge; of these patients, all currently alive more than 10 years following liver transplantation were selected for inclusion in the study. Thus, a total of 102 patients were invited to participate and sent QOL questionnaires. An overall response of 59.8% (n = 61) was achieved. Two individuals who responded did not wish to participate in the study, one of whom had severe memory loss. Two responses were discarded because of incomplete documentation. The final study group therefore consisted of 57 (55.8%) liver transplant recipients from the 102 patients invited. The responders comprised 21 males and 36 females with a mean age at transplantation of 36.9 years (range, 1-63 years) and at analysis of 51 years (range, 12-76 years). The mean posttransplant follow-up period was 14.2 years (range, 10-30 years). Table 1 shows the indications for liver transplantation.
| Diagnosis | n = 57 (%) |
|---|---|
| Primary biliary cirrhosis | 14 (25%) |
| Biliary atresia | 7 (12%) |
| Autoimmune cirrhosis | 6 (11%) |
| Metabolic indication | 6 (11%) |
| Alcoholic liver disease | 5 (9%) |
| Primary sclerosing cholangitis | 5 (9%) |
| Budd-Chiari syndrome | 4 (7%) |
| Fulminant hepatic failures | 4 (7%) |
| Tumor | 2 (3%) |
| Alagille's syndrome | 1 (2%) |
| Cryptogenic cirrhosis | 1 (2%) |
| Viral cirrhosis | 1 (2%) |
| Secondary biliary cirrhosis | 1 (2%) |
Thirty of the 57 (52%) patients experienced early acute rejection, and 8 (14%) experienced late acute rejection. Immunosuppression at last follow-up was variable with 41 (71.9%) patients on CNI-based immunosuppression. Thirty patients had suffered from CNI toxicity at some point in their follow-up and had been converted to non–CNI-based immunosuppression or continued on reduced CNI-based immunosuppression. The major posttransplant complications recorded in the 57 responders are summarized in Table 2.
| Complication | Number of Patients (%) with the Complication |
|---|---|
| Biliary complications | 18 (31.5%) |
| Recurrent disease | 12 (21%) |
| Malignancies | 12 (21%) |
| CMV reactivation | 6 (10.5%) |
| Vascular complications | 6 (10.5%) |
| Osteoporosis | 18 (31.5%) |
| Metabolic complications | 24 (42%) |
| NODAT | 5 (9%) |
| Hyperlipidemia | 19 (33%) |
| Reoperations | 20 (35%) |
| Retransplantation | 10 (17.5%) |
- Abbreviations: CMV, cytomegalovirus; NODAT, new onset diabetes after transplantation.
The demographics of the 45 individuals who did not respond or participate in the study were similar to those of the study participants. There were 25 males and 20 females, with a mean age of 41.6 years (range, 16-80 years) and a mean posttransplant duration of 14.0 years (range, 11-19 years). Five (11%) had recurrent disease, and 15 (33.3%) had posttransplant complications. Thirty-eight (84.4%) were on CNI-based immunosuppression, and 5 had been transferred to non–CNI-based immunosuppression because of CNI toxicity. There were no statistically significant differences between the responders and nonresponders for any of the variables studied (Table 3).
| Parameter | Responders (n = 57) | Nonresponders (n = 45) | P |
|---|---|---|---|
| Gender | 21 males, 36 females | 25 males, 20 females | NS |
| Mean age at transplant | 36.9 years (range, 1-63 years) | 41.64 years (range, 16-80 years) | NS |
| Mean age at analysis | 51 years (range, 12-76 years) | Not applicable | Not applicable |
| Mean posttransplant follow-up | 14.2 years (range, 10-30 years) | 14.04 years (range, 11-19 years) | NS |
| Immunosuppression | CNI: 41 Non-CNI: 14 None: 2 | CNI: 38 Non-CNI: 5 No information: 2 | NS NS NS |
| Recurrent disease | 12 | 5 | NS |
- Abbreviations: CNI, calcineurin inhibitor; NS, not significant.
QOL Indices
A box plot analysis of the SF 36v2 data (Fig. 1) was used to show those parameters with sample means more than 2 standard deviations below the mean for the UK general population based on the data of Jenkinson et al.6 There was a significant restriction in physical functioning and role physical of patients after liver transplantation, but there were no significant differences between the patients and the population mean for bodily pain, general health, mental health, role emotional, and vitality.
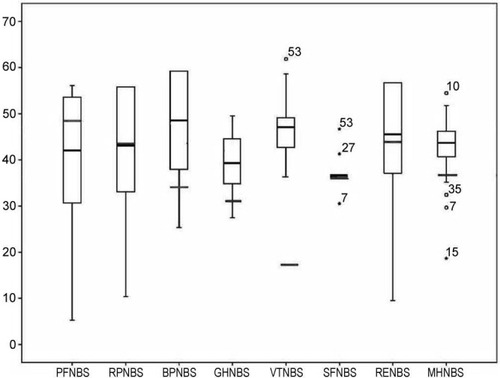
Box plot of individual Short Form 36 version 2 scores showing sample mean scores (black lines), population means (red lines), and ranges with outliers. Abbreviations: BP, bodily pain; GH, general health; MH, mental health; NBS, norm-based score; PF, physical functioning; RE, role emotional; RP, role physical; SF, social functioning; VT, vitality.
The results of the Ferrans and Powers analysis are shown as box plots in Fig. 2. Although the patients' perception of their QOL was generally good, a small number of older individuals reported a poorer QOL. The results obtained with the Ferrans and Powers and SF 36v2 questionnaires showed a significant correlation between the 2 scoring proformas for comparable parameters (Table 4).
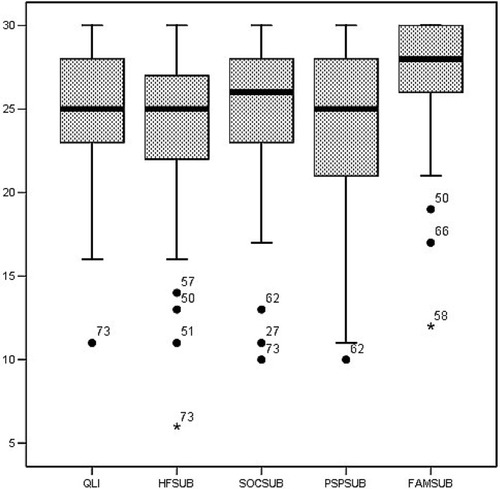
Distribution of measured values in the Ferrans and Powers questionnaire against a scale with a highest obtainable value of 30. The means are shown as thick, black lines, and the outliers are shown as circles and stars. Labels adjacent to outlier values show the age of the individual, thus demonstrating age to be the most important determinant for these outlier values. Abbreviations: FAMSUB, family subclass; HFSUB, health functioning subclass; PSPSUB, psychological/spiritual subclass; QLI, Quality of Life Index; SOCSUB, social subclass.
| Ferrans and Powers Parameter | Significant Correlation | |
|---|---|---|
| 99% Confidence Interval | 95% Confidence Interval | |
| QLI | PF-NBS, RP-NBS, GH-NBS, and RE-NBS | BP-NBS, MH-NBS, PCS, and MCS |
| Health functioning subclass | PF-NBS, RP-NBS, BP-NBS, GH-NBS, RE-NBS, and PCS | PF-NBS, RP-NBS, BP-NBS, GH-NBS, RE-NBS, and PCS |
| Social subclass | RE-NBS | PF-NBS |
| Psychological/spiritual subclass | RE-NBS and MCS | RE-NBS and MCS |
| Family subclass | RE-NBS | MH-NBS and MCS |
- Abbreviations: BP, bodily pain; GH, general health; MCS, mental cumulative score; MH, mental health; NBS, norm-based score; PCS, physical cumulative score; PF, physical functioning; QLI, Quality of Life Index; RE, role emotional; RP, role physical.
The results of univariate analysis used to determine the demographic and clinical factors associated with the QOL parameters are shown in Table 5. Age at analysis > 60 years, age at transplantation > 50 years, female gender, and the development of posttransplant complications were all associated with reduced QOL parameters. Alcohol as the cause of liver disease, recidivism, retransplantation, hepatic artery thrombosis, reoperation, CMV reactivation, acute rejection, the use of CNI agents, steroid usage, reoperations, and biliary complications had no influence on the QOL parameters.
| Factor | PF | BP | RP | GH | MH | RE | VT | SF | HF | PCS | MCS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age > 60 | * | * | * | * | |||||||
| Age > 50 at transplantation | * | * | * | * | |||||||
| Female sex | * | * | * | ||||||||
| Posttransplant complications | * | * | * | * | |||||||
| Osteoporosis | * | * | * | * | |||||||
| Chronic rejection | * | * | |||||||||
| Malignancy | * | * | * | ||||||||
| Calcineurin toxicity | * | * |
- Abbreviations: BP, bodily pain; HF, health functioning; GH, general health; MCS, mental cumulative score; MH, mental health; PCS, physical cumulative score; PF, physical functioning; RE, role emotional; RP, role physical; SF, social functioning; VT, vitality.
- * Significant (P < 0.05).
Multivariate Analysis
Binary logistic regression showed that recipient age more than 60 years, female gender, and posttransplant complications were the most important factors associated with decreased physical functioning. Severe osteoporosis was also found to correlate with reduced physical functioning when gender and age were excluded from the analysis. As expected, gender and age were important predictors for the presence of severe osteoporosis.
Recurrence of the original liver disease showed a significant association with the Quality of Life Index and the health functioning subclass in the Ferrans and Power questionnaire but did not show any relationship in the SF 36v2 indices. Age was identified as a significant factor that negatively influenced the QOL of liver transplant recipients in both of the questionnaires used.
DISCUSSION
The results of this single-center cross-sectional analysis reveal that patients 10 or more years after undergoing orthotopic liver transplantation generally have an overall good QOL but display a reduction in their ability to carry out physical activity (physical function) in comparison with the general population. The response rate to the survey of ∼60% is somewhat lower than reported in shorter term studies of QOL in liver transplant patients.9 However, the nonresponders in our study did not differ significantly from the responders in terms of their demographic and clinical details. The reasons for the low response rate are not clear, although it may be of relevance that approved ethical practice in the United Kingdom allows only a single follow-up to the initial postal invitation and does not encourage telephone or further postal reminders. Over the past decade, there has been an increasing realization that the benefits of liver transplantation are not fully reflected by morbidity and mortality alone and that there is a need for information on QOL. The perception of health by an individual is dependent on his or her personality, educational background, and economic status. There is a poor correlation between QOL reported by health professionals and relatives and that reported by patients.10
Several studies have assessed QOL during the first few years after liver transplantation and have shown gratifying results with improvement in QOL over that prior to transplantation.3 These studies show that return to work and good mental health are key to achieving a good QOL. However, to our knowledge, there is only 1 previous study that has evaluated QOL on patients in the longer term (>10 years) following liver transplantation.9 The previous study9 assessed patients from 3 centers using the French version of the National Institute of Diabetes and Digestive and Kidney Diseases instrument and addressed the issue of comparative QOL among kidney, liver, and heart recipients. The authors reported reduced physical functioning in liver transplant recipients, with the QOL approaching that of the general population at 1 to 2 years but then plateauing. The physical functioning of patients in the present study was significantly lower than that of the general population, and in contrast to Karam et al.'s study,9 we sought to correlate reduced QOL (physical function) with a range of clinical variables.9-16
Age, female gender, and osteoporosis showed the best correlation with reduced physical functioning and bodily pain. Age greater than 60 years tends to restrict personal functioning in the immediate posttransplant period4, 17 and is associated with increased mortality at 5 and 10 years after transplantation18; the cause of death is often unrelated to the original liver disease or transplantation procedure.17 However, the QOL in older recipients is similar to that of younger recipients 1 year after transplantation.4, 17 We found in the longer term a restriction of physical parameters when the age at transplant is more than 50 years or the age at follow-up is more than 60 years.
In the present study, reduced physical functioning, as assessed by the SF 36v2, was associated with older age (60 years) and female gender (both of which predispose to osteoporosis) along with posttransplant complications. In previous studies of QOL after liver transplantation,19 females had poorer physical functioning. Some have attributed this association to the nurturant (carer) social role adopted by women in our society, with resulting inability to adopt the sick role,19 and others have attributed this is to higher morbidity in females after liver transplantation.19 Our data suggest that osteoporosis negatively influences physical functioning and impairs QOL in woman after liver transplantation.
Patients with poor bodily pain scores tended to be female and osteoporotic and have evidence of calcineurin toxicity. It has been shown previously that limb and back pain has a high correlation with reduced bone density, tiredness, and depressive anxiety.20 In this study, we found that the mental health parameters were not significantly different from those of the general population, and this suggests that osteoporosis has a significant bearing on bodily pain after transplantation. There are many reasons why osteoporosis develops after liver transplantation,8 but the use of bisphosphonates early in the course of liver disease and steroid-sparing regimens may be useful strategies in reducing osteoporosis.
Our study shows that CNI toxicity and especially nephrotoxicity are associated with a reduced perception of good health, thereby highlighting the impact of renal dysfunction on QOL. In the present study, the results from the Ferrans and Powers questionnaire were not influenced by most of the factors that affected the norm-based score. Norm-based scores compare a given test group with the general population and therefore are useful in reflecting what effects procedures or diseases have on individuals in comparison with the general population.12 The Ferrans and Powers questionnaire, an importance-based questionnaire, weighs each response on the basis of the individual's perceived importance of that particular issue. Therefore, it may reflect more accurately the individuals' perception of QOL. In norm-based scoring, we found transplant patients to be physically worse off in comparison with the general population. This finding is consistent with that of other studies with shorter follow-up.16
The only factors in the present study that influenced the indices measured by the Ferrans and Powers questionnaire (an importance-based questionnaire) were recurrent liver disease and age > 50 years at transplantation. This suggests that recurrence of primary disease is perceived as important by the affected individual. Individuals after transplantation experience immense joy at freedom from a disease that made their life so miserable, and the recurrence of their liver disease brings with it all their previous fears. Fear influences the perceived importance of physical, emotional, and other parameters measured by the questionnaire, resulting in a poorer QOL index and health functioning.
Retransplants and reoperations, although addressing the problems faced by the patient, appear to have little influence on long-term QOL, probably because the patient appreciates the improvement in his or her condition due to these procedures and ascribes no importance to them. As this study included transplants that spanned several decades, the severity of the disease as denoted by the Child-Pugh or Model for End-Stage Liver Disease score was not retrospectively calculated. This might be an area of interest for future studies. The other limitation of this study is the disproportionately high percentage of patients with primary biliary cirrhosis. This could be due to the evolving indications for liver transplantation over the years or the relatively higher long-term mortality in patients with hepatitis, malignancies, and alcoholic liver disease. Caution should be exercised in generalizing the results of this study for cohorts of patients with markedly different indication profiles.
It is inevitable that long-term follow-up studies such as this will reflect the outcome of previous clinical practice rather than current practice. Future studies are required on this subject to demonstrate the influence of current practice and protocols. In conclusion, patients 10 or more years after liver transplantation generally have a good QOL, although physical functioning is reduced. Efforts should be directed toward the effective treatment of conditions such as osteoporosis that have an adverse impact on physical functioning after transplantation.
Acknowledgements
We thank our colleagues at UK Transplant for assistance with obtaining information. We thank Claire Jenkins, Ingela Oberg, Esther Moore, and Sarah Bowler of the Cambridge Medical Statistics Unit and Professor Mark Haggard of the MRC Brain Sciences Unit for all their help.




