Cruveilhier-Baumgarten disease in a patient with turner syndrome: Case report of a rare indication for liver transplantation
Abstract
Some chromosomal alterations can be associated with vascular abnormalities. For instance, Turner syndrome can be complicated by agenesis or hypoplasia of the portal venous system causing presinusoidal portal hypertension. Liver transplantation to treat this condition overcomes portal hypertension and reconstitutes the diminished hepatic function due to severe atrophy of the portal venous inflow. Liver Transpl 14:299–302, 2008. © 2008 AASLD.
Cruveilhier-Baumgarten disease is a rare congenital condition producing portal hypertension in association with patent umbilical or paraumbilical veins, hypoplasia of the intrahepatic portal system, and liver atrophy with minimal or no fibrosis. Patients with this condition experience classical features of portal hypertension such as gastrointestinal bleeding, ascites, and encephalopathy. Pronounced caput medusa and a venous hum over the region of the xiphoid process due to the presence of large umbilical and paraumbilical veins are frequent clinical findings. Surgical portosystemic shunting and splenectomy have been employed to alleviate portal hypertension in these patients, although this therapeutic approach does not reestablish normal liver function because of persistent severe hepatic atrophy.1 Herein, liver replacement in a patient with Cruveilhier-Baumgarten disease is reported. To the best of our knowledge, this is the first report of liver transplantation (LT) in a patient with this rare entity.
CASE REPORT
A 52-year-old female with Turner syndrome (a disorder of gonadal differentiation) and cryptogenic liver dysfunction underwent cadaveric LT. Manifestations of her liver disease included encephalopathy, gastrointestinal bleeding, refractory ascites, right hydrothorax, and hepatorenal syndrome requiring dialysis. Because of the patient's small size (4′ 10″ and 114 lbs) and infrequent blood type (AB+), she spent 6 months on the transplant waiting list. At the time of transplant, her Model for End-Stage Liver Disease score was 33.
During her surgery, the patient was found to have significant hepatic atrophy with no cirrhosis. Portal hypertension with large recanalized umbilical and periumbilical veins was observed along with an aneurysm of the portal vein containing a large intraluminal thrombus. These findings had been previously suggested in pretransplant computed tomography scans (Figs. 1 and 2).

Hepatic atrophy. Absence of intrahepatic portal vein branches. Patent umbilical vein (arrow).
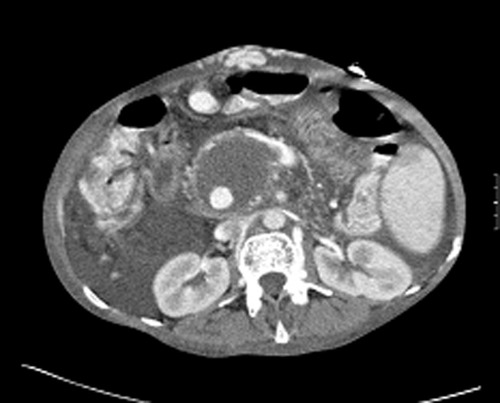
Varicose dilatation of portal vein with intraluminal thrombus (arrow).
On pathologic analysis, the explanted liver was remarkably atrophic (weight: 610 g) with absence of cirrhosis. A portal vein aneurysm with a thrombus and a recanalized umbilical vein were observed (Fig. 3).

Explanted liver. Patent umbilical vein (white arrow). Portal vein aneurysm with intraluminal thrombus (arrow).
Histologic examination revealed small portal vein branches and no fibrosis (Fig. 4). To confirm that the portal veins were indeed smaller than normal, interlobular portal tract areas and portal vein areas of 26 portal tracts from a normal liver (control) (Fig. 5) were measured and compared with 52 portal tracts from this patient's diseased liver. Multiple digital images of the two specimens were taken with a digital camera (Spot Insight QE, Diagnostic Instruments, Sterling Heights, MI) and a 10× objective. Measurements and analysis were performed with ImageProPlus software version 6.1 (Media Cybernetics, Silver Spring, MD) and Microsoft Office Excel 2003 (Microsoft Corp., Redmond, WA). The mean ratio of the portal vein area to portal tract area for the diseased liver was 0.01021 (standard deviation = 0.034936) versus 0.251556 (standard deviation = 0.100353) for the normal liver.
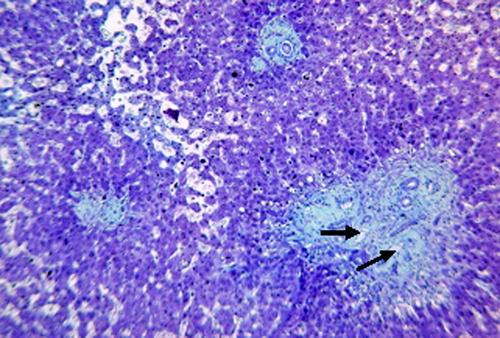
Diseased liver. Small intrahepatic portal vein caliber (arrows).
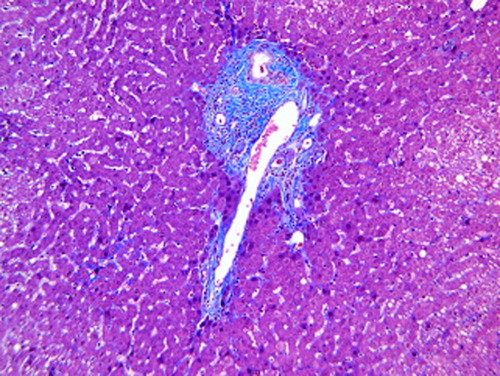
Normal liver. Normal size intrahepatic portal vein (arrow).
This patient's postoperative course was complicated by intrathoracic bleeding after right chest tube placement to treat a large hemothorax; thoracotomy was necessary to control the hemorrhage. In addition, she developed Candida albicans sepsis, which was successfully treated with antifungal agents. After a 2-month stay in the intensive care unit, the patient was transferred directly to a rehabilitation facility with preserved graft function. A month later, the patient required readmission to the hospital and died from respiratory failure and fungal urosepsis. Her liver graft function at that point was normal.
Abbreviation
LT, liver transplantation.
DISCUSSION
In 1833, Pegot first observed the combination of portal hypertension, hepatic atrophy with absence of cirrhosis, and patent umbilical vein in a patient with caput medusa and a venous murmur at the umbilicus. In 1852, Cruveilhier confirmed these findings in the patient's autopsy. In 1908, Baumgarten reported similar autopsy findings in a patient who died from massive gastrointestinal bleeding and suggested that this condition was induced by congenital hypoplasia of the portal system. A similar clinical condition in association with cirrhosis was termed Cruveilhier-Baumgarten syndrome. Since then, the term “syndrome” has been applied when cirrhosis is present, and the term “disease” has been applied to describe the condition associated with congenital portal venous system hypoplasia.1, 2
The patient that we describe had Turner syndrome caused by a complete or partial absence of one X chromosome.3 This is one of the most frequent chromosomal abnormalities, affecting 1 in 2000 live female births. It is characterized by ovarian dysgenesis, short stature, and lymphatic, renal, and cardiovascular abnormalities.4 Although 20% of patients with Turner syndrome have some degree of liver dysfunction, architectural changes in the liver have been reported only rarely.5 These include steatosis, steatohepatitis, portal vein agenesis, portal fibrosis, periductal fibrosis, nodular regenerative hyperplasia, multifocal nodular hyperplasia, and cryptogenic cirrhosis. It has been postulated that most of these architectural changes result from intrahepatic microcirculatory disturbances attributed to the congenital vascular abnormalities associated with this condition.6-11
Ours is the first report of Cruveilhier-Baumgarten disease in a patient with Turner syndrome undergoing LT.
An interesting facet of Cruveilhier-Baumgarten disease is the development of the collateral circulation. Embryologically, the umbilical and vitelline veins are paired vessels that empty into the forerunner of the right atrium, the sinus venosus. With the development of the liver, the left umbilical vein and the vitelline veins develop vascular channels that will later form the hepatic sinusoids. Although these channels develop between the sinus venosus and the original vessels in the umbilical stalk, a direct shunt from the umbilical veins to the embryonic heart is maintained by the ductus venosum. Although the right umbilical vein will disappear, the left umbilical vein, which drains into the left portal vein and into the right atrium via the ductus venosum, remains patent until birth. After birth, the ductus venosum closes, forming the ligamentum venosum, and the left umbilical vein atrophies to form the ligamentum teres in the falciform ligament. A small portion of the umbilical vein at its junction with the left portal vein may remain patent as the “restkanal” of Baumgarten. With closure of the ductus venosum in the presence of portal hypoplasia, presinusoidal portal hypertension develops after birth.
Although portosystemic shunting and splenectomy have been implemented in the past to treat this condition, LT becomes the treatment of choice by reestablishing physiologic portal circulation and appropriate organ function.
Unfortunately, because of her small size and infrequent blood type, the patient discussed herein underwent LT after a prolonged waiting time with a deteriorated general condition and increased risk for postoperative complications.
In conclusion, portal hypertension can be due to congenital hypoplasia of the intrahepatic portal vein system known as Cruveilhier-Baumgarten disease. In the absence of cirrhosis, severe parenchymal atrophy can induce marginal liver function. As described herein, delayed LT will have a similar negative impact as in the patient with cirrhosis, with an increased risk for septic complications and failure to thrive. LT successfully restores splanchnic venous drainage through the liver and provides renewed synthetic organ capability.




