Minimal anhepatic technique for living donor liver transplantation using right liver graft
The most critical moment in liver transplantation is graft reperfusion after an anhepatic period in which there is a chance of great hemodynamic instability that may lead to significant graft dysfunction in the postoperative period.1 During the anhepatic period, splanchnic congestion secondary to portal clamping occurs invariably without any liver function. Early persistent ionic hypocalcemia and late olyguric renal failure are the most constant and prominent complications during the anhepatic period.2
The usual anhepatic period in living donor liver transplantation (LDLT) does not appear to cause any detrimental effects, but the anhepatic period is a threat to patients and should be reduced as much as possible especially in hemodynamically unstable recipients with limited hepatic reserve.
Previous studies have shown that a temporary portocaval shunt to reduce splanchnic congestion improves hemodynamic status, reduces intraoperative transfusion requirements, and preserves renal function during and after orthotopic liver transplantation.3-6 This technique is particularly useful for patients with hepatocellular carcinoma (HCC) or fulminant hepatitis who lack adequate portosystemic collaterals in the splanchnic area. Nevertheless, it is an artificial shunt that is extraanatomic and not physiologic, requires some unwanted time, and does not avoid or reduce the entire anhepatic period.
We introduce a simple and effective technique to eliminate or minimize the seemingly inevitable anhepatic period for LDLT using right liver graft to address the 2 main problems of the anhepatic period: splanchnic congestion and no liver function.
SURGICAL TECHNIQUE
The abdomen is explored through a J-shaped incision with left extension. The whole liver is completely mobilized and freed from the inferior vena cava. The right hepatic artery, portal vein, hepatic vein are divided, and the right and left hepatic ducts are left open after division near the hilar plate. The recipient liver is attached only to the left portal vein, the left hepatic artery, and the common trunk of middle and left hepatic vein. At this point, the liver can be easily rotated and retracted to the left side without any compromise of the vascular flow of the left liver. The prepared right live graft was placed orthotopically after side-clamping of the inferior vena cava (IVC) to maintain blood flow. The right hepatic vein is anastomosed to the recipient IVC (Fig. 1A,B). The right portal vein of the graft is anastomosed to the right portal vein of the recipient. Before reperfusion of the graft, the left hepatic artery and portal vein of the recipient are ligated and divided, and the common trunk of the middle and left hepatic vein is stapled with a vascular stapler or divided between vascular clamps and oversewn. If the right portal vein of the graft is anastomosed to the main portal vein of the recipient due to the problems such as size discrepancy and redundancy, only an anastomosis between the right portal vein of the graft and the main portal vein of the recipient is performed under the anhepatic period. Thereafter, hepatic artery anastomosis is performed under operating microscope before biliary reconstruction.
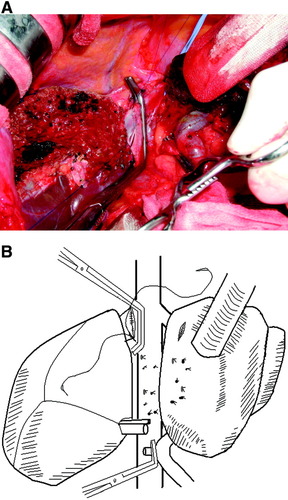
(A) Operative and (B) schematic views of the minimal anhepatic technique for living donor liver transplantation using right liver graft. An end-to-side anastomosis is being performed between the right hepatic vein of the graft and the side-clamped IVC of the recipient with the recipient liver fully mobilized, attached only to the left portal vein, the left hepatic artery, and the common trunk of middle and left hepatic vein, and rotated to be retracted to the left side.
Abbreviations
HCC, hepatocellular carcinoma; IVC, inferior vena cava; LDLT, living donor liver transplantation.
RESULTS
During January 2007, this technique was used in 2 patients with HCC associated with hepatitis B virus-related cirrhosis. There was no anhepatic period in one recipient. The other had an anhepatic period of 7 minutes during which only the right portal vein of the graft was anastomosed to the main portal vein of the recipient due to size mismatch and redundancy.
The hemodynamic stability with a urine output of 0.5-1 mL/kg/hour or greater was maintained without any vasopressor or diuretic given, and no blood transfusion was required during operation. The intraoperative fluid administration guided by hemodynamic monitoring and urine output was kept uniformly throughout the whole operation. Both patients were extubated following the transplant procedure. Each operative time was 570,732 minutes and each implantation time was 120,195 minutes. Both patients had no postoperative complications related to this technique and showed an uneventful postoperative course except that one patient developed acute rejection which was treated by steroid pulse therapy.
DISCUSSION
The advantages of this minimal anhepatic technique are avoidance of mesenteric stasis and bowel edema, subsequent development and release of anaerobic metabolism products into the general circulation, and bacterial translocation, and reduction of blood loss due to decompression of the portal circulation, minimizing transfusion and volume requirements. In addition, the liver functions including the coagulation profiles, if not good in patients with end-stage liver disease but nearly normal in unresectable HCC patients with good liver function, can work longer.
The usual J-shaped incision with left extension or bilateral subcostal incision with upper midline incision provides wide exposure to secure sufficient space to retract the diseased liver to the left side without any compromise of the vascular flow of the left liver and to place the right liver graft for implantation in the peritoneal cavity. Especially the diseased small cirrhotic liver can be more easily retracted. There was not enough kinking or twisting of the remaining left portal vein and the common trunk of middle and left hepatic veins to impede the blood flow of the left liver, which could be confirmed by Doppler ultrasonography.
This technique may have a limitation in applying to a large diseased liver with such as polycstic liver disease or large tumors, in which the liver may be difficult to retract to the left side even after a large abdominal incision. Otherwise, the liver can be easily rotated and retracted to the left side once the recipient liver is fully mobilized and attached only to the inflow and outflow vessels of the left liver.
If the middle hepatic vein requires reimplantation, the common orifice of the right and middle hepatic veins or the venous conduit draining prominent segment V and VIII hepatic veins of a graft formed on the back table procedure can be anastomosed to the recipient IVC.
This minimal anhepatic technique can maintain the portal flow through the “natural shunt” of left liver of the recipient to the IVC until the moment of reperfusion and can replace the temporary portocaval shunt required in hemodynamically unstable patients.
To reduce anhepatic period hitherto, the operator have no choice but to make rapid anastomoses of hepatic and portal veins under the pressure that the longer the anastomoses, the worse the outcome of the graft and the recipient. However, using this technique, even the novice can have enough time to keep one's composure to do the anastmoses.
Although we are not yet experienced in LDLT using left liver graft, this technique may be applied to it if the recipient liver is fully mobilized, attached only to the right portal vein, the right hepatic artery, and the right hepatic vein, and rotated to be retracted to the right side after the left hepatic artery, portal vein, hepatic duct, and the common trunk of the middle and left hepatic vein are divided.
In conclusion, this technique has the advantages of less splanchnic congestion and longer use of liver function of the native liver. Therefore, this technique may be recommended as a preferred technique for minimizing the anhepatic period in the graft implantation of LDLT.
Acknowledgements
We express our gratitude to all anesthesiologists and all surgery nurses of the Center for Liver Cancer for their help and patience to perform this operation.