The role of 18F-FDG-PET imaging for the selection of liver transplantation candidates among hepatocellular carcinoma patients
Abstract
Positron emission tomography (PET) using F-18 fluoro-2-deoxy-d-glucose (18F-FDG) is now well established as a noninvasive diagnostic tool for the detection of a variety of malignant tumors. However, in the case of hepatocellular carcinoma (HCC), several investigators have reported controversial conclusions and an inadequate sensitivity for PET (50-55%). Nevertheless, a high positive rate of 18F-FDG accumulation has been reported in patients with high-grade HCC and in those with markedly elevated alpha-fetoprotein (AFP) levels. Here, we retrospectively reviewed 38 HCC cases that received liver transplantation (LT) at our center between November 2000 and July 2004 and underwent whole-body PET imaging. 18F-FDG uptake was assessed in the liver, and its prognostic significance was investigated. Of 38 patients enrolled, 13 patients had positive PET scans for a liver tumor. When we analyzed the association between tumor factors and PET+ (greater PET lesion uptake) in the liver, preoperative AFP level and vascular invasion were found to be significantly associated with PET+ (P = 0.003 and P < 0.001, respectively). However, the association between histological grade and PET+ findings did not reach statistical significant difference (P = 0.074). Moreover, the 2-year recurrence-free survival rate of PET− patients was significantly higher than that of PET+ patients (85.1% vs. 46.1%) (P = 0.0005). Of 6 PET+ patients who met the Milan criteria, 4 patients (66.7%) had recurrence, but all 20 PET− patients who met the Milan criteria were recurrence free. Thus, PET imaging could be a good preoperative tool for estimating the post-LT risk of tumor recurrence, because histological grade and vascular invasion cannot be determined preoperatively. Importantly, our results indicate that tumor recurrence can be highly anticipated for PET-imaging-positive HCC patients who satisfy the Milan criteria. We advise that PET+ HCC patients be selected cautiously for LT. Liver Transpl, 2006. © 2006 AASLD.
F-18 fluoro-2-deoxy-d-glucose (18F-FDG) uptake allows the cellular glucose metabolism to be estimated by positron emission tomography (PET). The normal liver contains a relative abundance of glucose-6-phosphatase and lower levels of hexokinase, whereas tumor cells tend to have increased hexokinase but little, if any, glucose-6-phosphatase activity.1-4 This difference in metabolism results in an increased accumulation of 18F-FDG in hepatocellular carcinoma (HCC) and metastatic liver tumors, and it potentially allows normal and tumor tissues to be differentiated on PET scans.
PET using 18F-FDG (18F-FDG-PET) is now well established as a noninvasive diagnostic tool for the detection of a variety of malignant tumors, such as, brain, head and neck, lung, pancreatic, and colon tumors.5, 6 PET imaging has established itself as a useful diagnostic method for metastatic liver tumors because it can detect these lesions with high sensitivity.5-8 In the case of HCC, however, several investigators have reported controversial results.7-12 The most common view seems to be that the sensitivity of PET imaging is not sufficiently high (50-55%).10, 13, 14 Extrahepatic metastases from HCC are not uncommon,15-17 and the incidence of extrahepatic HCC has been reported to be 37%, with the detection for the lung, lymph nodes, and bone.18 The detection rate of PET imaging for extrahepatic metastases larger than 1 cm in greatest diameter has been reported to be 83%, which suggests that PET imaging has potential as a diagnostic tool for the identification of extrahepatic HCCs larger than 1 cm.19
In patients with cirrhosis and complicated HCC, liver transplantation (LT) offers the only hope for cure. It has been reported that long-term survival can be achieved by LT in patients with a solitary HCC of 5 cm or smaller in diameter or up to 3 nodules of 3 cm or smaller in diameter.20 In that study, morphological information was provided by ultrasound, computed tomography, magnetic resonance imaging, and angiography. However, when LT selection criteria for HCC are applied, other parameters (vascular invasion, histological grade, etc.) should also be considered. Cillo et al. reported that histological grading using such new parameters could further increase the prognostic precision of estimating the post-LT risk of tumor recurrence, because tumor differentiation may accurately reflect tumor aggressiveness and consequent posttransplant risk of recurrence.21
By the past reports, the PET findings by the accumulation of 18F-FDG in a primary HCC lesion are different according to the degree of HCC differentiation.7, 22 Moreover, PET imaging can provide metabolic information and reflect an aggressive tumor nature, and metabolic changes may precede morphological changes in tumors.
Recently, PET has been routinely applied for the detection of extrahepatic metastases in HCC before LT at our center. In the present study, we assessed 18F-FDG uptake in liver and investigated retrospectively the role of PET in the evaluation of tumor recurrence after LT for HCC as well as its prognostic significance.
Abbreviations
18F-FDG, F-18 fluoro-2-deoxy-d-glucose; PET, positron emission tomography; HCC, hepatocellular carcinoma; LT, liver transplantation; AFP, alpha-fetoprotein; 18F-FDG-PET, PET using 18F-FDG. Supported in part by a grant from 21C Frontier Functional Human Genome Project of Korean Ministry of Science and Technology.
PATIENTS AND METHODS
In this study, we retrospectively reviewed 38 HCC patients who received LT at Seoul National University Hospital between November 2000 and July 2004. All 38 patients were diagnosed as having HCC by conventional radiologic imaging and underwent a whole-body PET scan for the detection of extrahepatic metastases. Data collected included gender, age, viral status, Child-Turcotte-Pugh classification, recurrence, date of recurrence, PET imaging findings, tumor stage, tumor size, tumor number, histological grade, preoperative alpha-fetoprotein (AFP) levels, and the presence of vascular invasion. If a PET scan identified any extrahepatic metastases before LT, after it was confirmed by the biopsy or other imaging studies, these patients were excluded from the candidates of LT at our center. A PET+ finding was defined as an observed greater uptake of 18F-FDG in a primary HCC lesion than in a normal liver. Primary HCC lesions were reviewed on the basis of pathologic report issued after LT. Vascular invasion was identified by the histological examination of the explanted livers, while the patients with grossly major vascular invasion by the preoperative imaging studies were excluded from the candidates of LT. Tumor differentiation was graded according to the Edmonson and Steiner grading system, and tumor node metastases staging was performed according to sixth edition of the American Joint Committee on Cancer/International Union Against Cancer.
The mean age of the 38 adult recipients was 54±8 years (range, 38-77), and 26 patients were males (76.76%). Viral infection was associated with liver disease in 37 (97.4%) patients (hepatitis B, n = 32 [84.2%]; hepatitis C, n = 3 [7.9%]; both hepatitis B and C, n = 2 [5.3%]; neither hepatitis B nor C, n = 1 [2.6%]). Demographic information and tumor characteristics are summarized in Tables 1 and 2. One patient (2.6%) received a cadaveric liver graft, and 37 patients (97.4%) received a living donor partial graft.
| Characteristics | Number of patients (Total = 38) | |
|---|---|---|
| Mean age (years) | 54 ± 8 (range, 38-77) | |
| Mean follow-up period (months) | 19 (range, 5-40) | |
| Gender | Male | 29 (76.7%) |
| Female | 9 (23.3%) | |
| Donor | Cadaveric | 1 (2.6%) |
| Living | 37 (97.4%) | |
| Child-Turcotte-Pugh class | A | 7 (18.4%) |
| B | 9 (23.7%) | |
| C | 22 (57.9%) | |
| Etiology | HBV | 32 (84.2%) |
| HCV | 3 (7.9%) | |
| Both HBV and HCV | 2 (5.3%) | |
| Neither HBV nor HCV | 1 (2.6%) | |
| TNM stage* | T1 | 15 (39.5%) |
| T2 | 20 (52.6%) | |
| T3 | 2 (5.3%) | |
| T4 | 0 | |
| Milan criteria | Meet | 26 (68.4%) |
| Exceed | 12 (31.6%) | |
| 18F-FDG-PET | + | 13 (34.2%) |
| − | 25 (65.8%) | |
| Tumor recurrence | Recurred | 11 (28.9%) |
| Not recurred | 27 (71.1%) | |
- Abbreviations: HBV, hepatitis B virus; HCV, hepatitis C virus; TNM, tumor node metastases.
- * One patient was excluded due to total necrosis resulting from transarterial chemoembolization.
| Tumor Factors | PET*− (n = 25) | PET+ (n = 13) | P Value† |
|---|---|---|---|
| Vascular invasion | 0.003 | ||
| − | 23 | 6 | |
| + | 2 | 7 | |
| Histologic grade‡ | 0.074 | ||
| I, II | 12 | 2 | |
| III, IV | 12 | 11 | |
| Preoperative AFP level | <0.001 | ||
| ≤200 ng/mL | 23 | 4 | |
| >200 ng/mL | 2 | 9 | |
| Number of tumors | 1 | ||
| ≤3 nodules | 21 | 11 | |
| >3 nodules | 4 | 2 | |
| Tumor size | 0.315 | ||
| ≤5 cm | 23 | 10 | |
| >5 cm | 2 | 3 |
- * 18F-FDG-PET.
- † By Fisher exact test.
- ‡ One patient was excluded due to total necrosis resulting from transarterial chemoembolization.
Statistical analysis of data was performed using SPSS version 11.5 for Windows (SPSS Inc., Chicago, IL). We analyzed for associations between tumor factors and PET imaging findings for a relation between tumor recurrence and PET imaging. Tumor recurrence rates and recurrence-free survival rates were analyzed according to PET findings. Recurrence-free survival was considered from the day of surgery to the day of recurrence and was calculated by considering any patient dead or living with recurrence as an event. Patient deaths unrelated to HCC recurrence were censored during the statistical analysis of HCC recurrence. Differences of P < 0.05 were considered to be statistically significant.
RESULTS
Associations Between Tumor Factors and 18F-FDG-PET Findings
Thirteen patients (34.2%) had PET scans that were positive, while 25 (65.8%) patients had negative scans. Of 9 vascular invasion (+) patients, 7 patients (77.8%) had a PET+ finding, and of 11 patients with a preoperative AFP level of >200 ng/mL, 9 patients (81.8%) had a PET+ finding. When we analyzed for the association between tumor factors and PET findings, preoperative AFP and vascular invasion were found to be significantly associated with PET findings (P = 0.003 and P < 0.001, respectively). In this study, 14% of low-grade tumors were PET+ findings, while 48% of high-grade tumors were PET+ findings, but this difference did not reach statistical significance (P= 0.074). Also, tumor size and number were not significantly associated with PET+ (P > 0.05) (Table 2).
Association Between HCC Recurrence and 18F-FDG-PET Findings
Of 13 PET+ patients, 8 (61.5%) suffered recurrence. The association between tumor recurrence and PET+ was significant (P = 0.003), and PET+ HCC patients had an overall greater risk of tumor recurrence than PET− patients (odds ratio = 7.6; 95% confidence interval (CI),1.990-28.997) (Table 3).
- Abbreviation: CI, confidence interval.
- * Fisher exact test.
- † Univariate analysis using a Cox proportional hazard model.
- ‡ 18F-FDG-PET.
According to PET imaging, the 1-year recurrence-free predictive value (negative predictive value for recurrence at 1 year in the PET− patients) was 92.0%, and 1-year recurrence predictive value (positive predictive value for recurrence at 1 year in the PET+ patients) was 53.8% (Table 4).
| Tumor Recurrence at 1 Year | 1-Year Recurrence Predictive Value* | 1-Year Recurrence-Free Predictive Value† | ||
|---|---|---|---|---|
| + | − | |||
| PET | ||||
| + | 7 | 6 | 53.8% | 92.0% |
| − | 2 | 23 | ||
- * Positive predictive value for recurrence at 1 year in the PET+ patients.
- † Negative predictive value for recurrence at 1 year in the PET− patients.
The 2-year recurrence-free survival rate for the 38 HCC patients was 71.5%, and 11 (28.9%) patients experienced recurrence (Fig. 1). The 2-year recurrence-free survival rate of PET− patients was 85.1%, and this was significantly higher than that of PET+ patients (46.1%) (P = 0.0005) (Fig. 2).
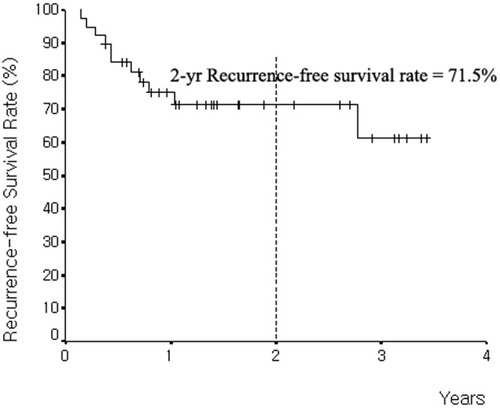
Cumulative recurrence-free survival curve of 38 HCC patients after liver transplantation. The 2-year recurrence-free survival rate is 71.5%.
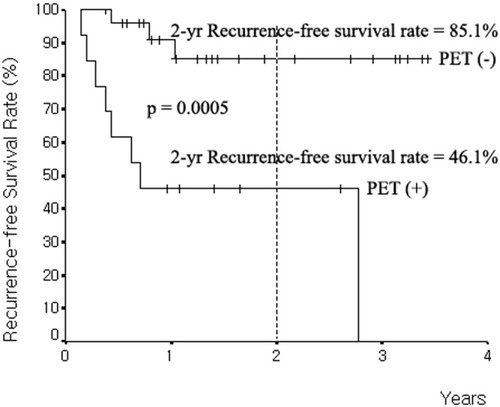
Cumulative recurrence-free survival curve according to 18F-FDG-PET imaging. The 2-year recurrence-free survival rate for PET− is 85.1%. The 2-year recurrence-free survival rate for PET+ is 46.1%. P = 0.0005.
Of the 6 PET+ patients who met the Milan criteria, 4 patients (66.7%) had recurrence. However, none of the 20 PET− patients who met the Milan criteria had recurrence. Of the 7 PET+ patients who exceeded the Milan criteria, 4 patients (57%) had recurrence, and of the 5 PET− patients who exceeded the Milan criteria, 3 patients (60%) had recurrence (Table 5).
| MC* | PET† | Tumor Recurrence | AFP (ng/mL) | Tumor Size (cm) | Number of Tumors | Vascular Invasion | Histologic Grade‡ |
|---|---|---|---|---|---|---|---|
| Meet (n = 26) | + (n = 6) | − | 20 | 1.5 | 2 | − | II |
| 46 | 1.3 | 1 | − | IV | |||
| + | 470 | 3 | 2 | + | II | ||
| 373 | 2.8 | 1 | + | III | |||
| 4,880 | 5 | 1 | + | III | |||
| 9,700 | 3 | 1 | − | III | |||
| − (n = 20) | − | ≤200 | − (Except 1 patient) | I, II, III | |||
| Exceed (n = 12) | + (n = 7) | − | 1,460 | 6 | 1 | − | III |
| 46 | 4.5 | 2 | − | III | |||
| 47 | 4.5 | 2 | − | III | |||
| + | 4,270 | 3.2 | 2 | + | III | ||
| 2,690 | 5.5 | 1 | + | III | |||
| 20,000 | 25 | ≥10 | + | IV | |||
| 1,360 | 4 | ≥10 | + | IV | |||
| − (n = 5) | − | 18 | 8 | 3 | + | II | |
| 52 | 4.2 | 4 | − | III | |||
| + | 1,360 | 3 | 5 | − | IV | ||
| 2,820 | 6 | ≥10 | − | III | |||
| 31 | 2.4 | 4 | − | IV |
- * Milan criteria.
- † 18F-FDG-PET.
- ‡ Edmonson and Steiner grading system.
DISCUSSION
LT offers the advantage of radical tumor removal even in patients with multifocal disease or severe cirrhosis. It also removes the risk of metachronous lesions developing in the liver remnant, and it restores normal liver function. However, because of the limited availability of donor organs, LT for HCC using deceased donors is justified only when curative intent can be realistically pursued. Best long-term results and lowest recurrence rates are achieved when candidates with early-stage HCC are selected.20, 23 Thus, a tumor factor based on the sizes and numbers of nodules is incorporated into the conventional staging procedure (i.e., the Milan criteria).20 However, we have experienced unexpected tumor recurrence after LT for HCC in patients who have met the Milan criteria. At present, the issue of concern is how to select candidates of LT for HCC and how to predict accurately and reduce tumor recurrence. Thus, we investigated the potential role of PET imaging for the evaluation of tumor recurrence after LT for HCC and its prognostic significance.
Well-differentiated HCC cells exhibit an 18F-FDG metabolism similar to that of normal liver tissue, whereas undifferentiated HCC cells do not.7, 22 Based on this result, the accumulation of 18F-FDG in a well-differentiated HCC may be similar to that of the surrounding normal liver, making the detection of HCC difficult. However, this characteristic could be used as an indicator of the degree of HCC differentiation.22 In a recent study, well-differentiated and well-to-moderately differentiated types were found to show a tendency toward negativity by PET imaging, whereas poorly differentiated and moderately-to-poorly differentiated types show increased 18F-FDG metabolism.24
In the present study, the association between the PET+ findings and the degree of HCC differentiation did not reach statistical significant difference (P= 0.074). However, we found that PET+ scans showed a statistically significant association with preoperative AFP and vascular invasion (P < 0.05), and most of the cases with posttransplant recurrence (63.6%) had evidence of vascular invasion. Thus, these results show that PET+ scans could reflect the aggressiveness and malignant potential of these HCC lesions.
Several studies have identified tumor size, tumor number, vascular invasion, histological grade, and preoperative AFP level as key risk factors of tumor recurrence after LT for HCC.25-31 Preoperative AFP level, vascular invasion, histological grade, and aggressive behavior during the waiting period are likely to reflect the risk of recurrence and should be considered when one is considering a patient for LT.28, 31 Moreover, because PET+ imaging reflects histological grade and vascular invasion, PET imaging findings and preoperative AFP level could further increase prognostic precision in terms of estimating the post-LT risk of tumor recurrence, and thus, substantially improve the patient selection process.
In this study, the association between tumor recurrence and PET+ imaging was significant (P = 0.016), and HCC patients with a PET+ finding were found to have an overall higher risk of tumor recurrence than those with a PET− finding (odds ratio = 7.6; 95% confidence interval, 1.990-28.997) (Table 3). In addition, a significant difference of cumulative recurrence-free survival was observed between those with different PET imaging findings (P = 0.0028) (Fig. 2). Also, the 1-year recurrence-free predictive value was 92.0%, according to PET imaging, while 1-year recurrence predictive value was 53.8%. These results means that a PET− finding predicts recurrence-free survival well (Table 4).
Of the 6 PET+ patients who met the Milan criteria, 4 patients (66.7%) experienced recurrence, but none of the 20 PET− patients who met the Milan criteria had recurrence, indicating that HCC patients who meet the Milan criteria with a positive PET imaging can be highly anticipated to experience recurrence. Therefore, PET+ HCC patients should be selected cautiously as candidates for LT, although a PET+ finding is not still an absolute contraindication for LT in HCC patients.
Histological grade and vascular invasion cannot be determined preoperatively, but PET+ liver scans could reflect these parameters and the risk of tumor recurrence. In conclusion, when LT selection criteria for HCC patients are applied or somewhat widened, 18F-FDG-PET imaging should be considered to evaluate tumor aggressiveness for a better estimate of post-LT recurrence risk.




