A new side effect of immunosuppression: High incidence of hearing impairment after liver transplantation
Abstract
Little is known about hearing impairment in patients after organ transplantation. We conducted a single-center study to evaluate hearing impairment in patients after orthotopic liver transplantation (OLT). A questionnaire was sent to 695 adult patients after OLT to assess characteristics and course of auditory impairment. Risk factors such as ototoxic drugs were taken into consideration. Clinical follow-up, including immunosuppressive therapy, was analyzed in detail. The questionnaire was completed by 521 patients (75%). Hearing impairment was reported by 184 patients (35%). A total of 43 patients (8%) suffered from hearing abnormalities prior to OLT. The remaining 141 patients (27%) developed hearing impairment after transplantation. Main problems were hearing loss (52%), tinnitus (38%), and otalgia (30%). There was no association of post-OLT hearing disorders with age or known risk factors. In 43% of patients, onset of hearing impairment was within 2 yr post-OLT. Hearing loss was positively associated with tacrolimus immunosuppression in univariate (P < 0.05) and multivariate analysis (P < 0.02). Patients using a hearing aid received tacrolimus more frequently than cyclosporine (P < 0.05). In conclusion, subjective hearing impairment is frequent in patients after OLT and contributes to post-OLT morbidity. Calcineurin inhibitor-related neurotoxicity appears as a possible mechanism. Further prospective investigations with objective hearing tests are necessary to confirm these results and to evaluate the role of immunosuppression. Liver Transpl, 2006. © 2006 AASLD.
Hearing impairment is common and its prevalence increases with age.1 A number of risk factors, such as ototoxic drugs (e.g., aminoglycoside antibiotics, loop diuretics), are known to cause hearing impairment.2, 3 Main clinical manifestations are sudden or chronic hearing loss, tinnitus, and otalgia. It has been shown that hearing impairment is a major factor in the subjective perception of health status.4 It may therefore severely influence patients' quality of life.
Nowadays, orthotopic liver transplantation (OLT) is a standard procedure in the therapy of end-stage liver disease. With increasing long-term survival, therapeutic side effects are becoming more important and significantly impact the patients' quality of life.5-7 Little is known about hearing impairment in patients after organ transplantation. Many side effects of immunosuppressants have been well studied. Of these, cardiovascular side effects are common in patients receiving calcineurin inhibitors.8, 9 Cardiovascular factors are known to be involved in the pathophysiology of some hearing disorders. Another frequent side effect of calcineurin inhibitors that may potentially cause hearing impairment is neurotoxicity.10, 11
Up to now, only few cases reported hearing loss in adults after organ transplantation receiving different immunosuppressants (cyclosporine, tacrolimus, OKT3, antithymocyte globulin).12-17 We conducted a single-center study including all adult patients alive after liver transplantation to evaluate their subjective hearing status and detect hearing impairment.
Abbreviation
OLT orthotopic liver transplantation
EXPERIMENTAL PROCEDURES
The study was approved by the Ethics Committee of the Hannover Medical School. The Declaration of Helsinki was followed. A questionnaire was sent to all 695 alive adult patients after liver transplantation who are cared for at our center. Characteristics and course of auditory impairment were assessed by the questionnaire. It explicitly asked for the following problems: 1) general hearing problems, 2) sudden hearing loss, 3) chronic hearing loss, 4) need of hearing aid, 5) tinnitus, 6) otalgia or auditory pressure sensation, 7) buzzing, 8) middle ear effusion, 9) impacted cerumen, and 10) aural surgery or trauma. For all problems, date of onset, extent (uni- or bilateral), and follow-up of the hearing impairment were requested as well.
Beyond the general data on patients and their course before and after liver transplantation, actual and past history of immunosuppression was noted in full detail. Risk factors such as ototoxic drugs (i.e., aminoglycoside antibiotics, erythromycin, vancomycin, loop diuretics, salicylates, vinblastine, cisplatin), renal failure (necessity of renal replacement therapy or creatinine clearance <60 mL/minute or serum creatinine >100 μmol/L), arterial hypertension (necessity of antihypertensive drug therapy or blood pressure elevated in 24-hour measurement or blood pressure >135/85 mmHg on at least 2 occasions), diabetes mellitus (necessity of antidiabetic treatment or positive oral glucose tolerance test), and intense exposure to noise (subjective, job related) were documented.
SPSS software version 11.5 (SPSS, Chicago, IL)was used for statistical analysis. All data are presented as mean ± standard deviation. Chi-square test was used for categorical variables. Comparisons between independent groups were performed with the unpaired t-test or analysis of variance, respectively. Correlations were assessed with Pearson's correlation coefficient. Multivariate associations were evaluated using pairwise stepwise multiple regression analysis. P < 0.05 was considered statistically significant.
RESULTS
The questionnaire was fully completed by 521 of the 695 patients (75%). Auditory impairment was reported by 184 of them (35%). A total of 43 of these 184 patients (23%; 8% of all responding patients, respectively) suffered from preexisting hearing abnormalities prior to OLT. The remaining 141 patients (77%; 27% of responding patients, respectively) newly developed hearing impairment after OLT. Mean patient age was 51 ± 13 yr with a mean follow-up of 8 ± 5 yr since OLT. The main characteristics and transplant indications in the different patient groups are given in Table 1.
| Patients' characteristics | Hearing impairment | No response | Total | P | ||
|---|---|---|---|---|---|---|
| Post-OLT | Pre-OLT | No | ||||
| No. of patients (%) | 141 (20) | 43 (6) | 337 (49) | 174 (25) | 695 (100) | |
| Male (%) | 47% | 70% | 50% | 53% | 52% | ‡, § |
| Age at evaluation (yr) | 51 ± 13 | 53 ± 13 | 49 ± 13 | 45 ± 14 | 49 ± 14 | * |
| Age at OLT (yr) | 41 ± 14 | 46 ± 13 | 41 ± 13 | 36 ± 15 | 40 ± 14 | *, ‡ |
| Follow-up since OLT (yr) | 8 ± 5 | 5 ± 4 | 7 ± 5 | 8 ± 5 | 7 ± 5 | *, ‡ |
| Retransplantation (%) | 12% | 12% | 9% | 12% | 10% | |
| Multiorgan transplantation (%) | 4% | 5% | 3% | 1% | 4% | |
| Living donor OLT (%) | 0% | 0% | 3% | 5% | 2% | † |
| Indication for OLT (%) | ||||||
| Virus-induced cirrhosis | 30% | 49% | 27% | 30% | 29% | ‡ |
| Autoimmune liver disease | 29% | 23% | 32% | 21% | 28% | * |
| Other cirrhosis | 11% | 13% | 8% | 10% | 9% | |
| Acute liver failure | 9% | 2% | 6% | 10% | 7% | |
| Vascular liver disease | 6% | 0% | 5% | 6% | 5% | |
| Liver tumor | 4% | 0% | 5% | 3% | 4% | |
| Other liver disease | 13% | 12% | 18% | 21% | 16% | |
- NOTE: Subgroups are patients with hearing impairment occuring after liver transplantation (post-OLT), prior to OLT (pre-OLT), without hearing impairment (no) and patients not responding to the questionnaire (no response).
- Abbreviations: OLT, Orthotopic liver transplantation.
- * P < 0.05 between patients with no response to the questionnaire and the responding patients.
- † P < 0.05 between patients with no hearing impairment and other responding patients.
- ‡ P < 0.05 between patients with preexisting hearing impairment and other responding patients.
- § P < 0.05 between patients with post-OLT hearing impairment and other responding patients.
Of the 141 patients with newly developed hearing disorders, 43 patients (30%) reported more than 1 symptom. Hearing loss was reported by 73 of 141 patients (52% of patients with hearing impairment after OLT; 15% of all 478 responding patients without preexisting hearing impairment, respectively). Other frequent complaints were tinnitus (n = 54; 38%; 11%, respectively) and otalgia (n = 45; 32%; 9%, respectively). All types of hearing disorders after liver transplantation are shown in Table 2.
| Type of hearing disorder | Patients | % of all patients* | % of patients with impairment post-OLT† |
|---|---|---|---|
| Hearing loss | 73 | 15% | 52% |
| Tinnitus | 54 | 11% | 38% |
| Otalgia | 45 | 9% | 32% |
| Sudden hearing loss | 19 | 4% | 13% |
| Hearing aid | 16 | 3% | 11% |
| Buzzing | 11 | 2% | 8% |
| Middle ear effusion | 6 | 1% | 4% |
| Impacted cerumen | 3 | 1% | 2% |
| Aural surgery, trauma | 2 | <1% | 1% |
- * All patients responding to the questionnaire without preexisting hearing disorders (n = 478).
- † Patients with hearing impairment that was not preexisting prior to liver transplantation (n = 141).
Mean time since liver transplantation at onset of hearing impairment was 4 ± 4 yr. In 43% of the patients (61/141), onset of hearing impairment was within 2 yr of OLT (Fig. 1). In 18 patients, 1 or all hearing disorders had already disappeared at the time of the interview. In 24 patients, the impairment was reported to occur intermittently.
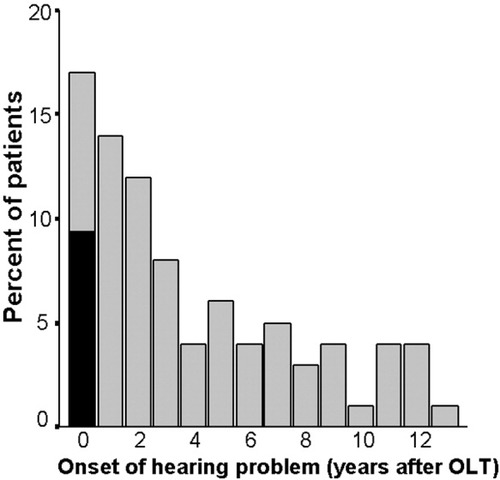
Onset of hearing impairment after liver transplantation. Shown is the percentage of patients who developed hearing impairment after liver transplantation (n = 141) in relation to its reported onset. In 9% of patients, onset of hearing impairment after liver transplantation was within 3 months of liver transplantation, as represented by the dark bar inside the first column.
The prevalence of preexisting hearing disorders increased with the patients' age (P < 0.02; see Fig. 2). In patients with post-OLT hearing impairment, this association was not found (P = 0.3). Other exogenic and endogenic risk factors for hearing disorders post-OLT were found in 124 of 141 patients (88%; Table 3). A total of 44 patients (31%) underwent potentially ototoxic drug therapy; 33 of these patients (23%) received loop diuretics. All risk factors were not statistically different between the different patient groups or between particular types of hearing impairment. Immunosuppression was not different between patients with or without hearing impairment after transplantation.
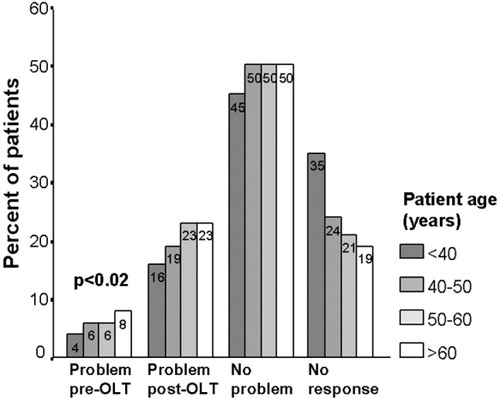
Hearing status and age after liver transplantation. Shown is the percentage of all patients of each age category at time of hearing evaluation (<40 yr, n = 187; 40–50 yr, n = 154; 50–60 yr, n = 177; >60 yr, n = 177). Prevalence of preexisting hearing disorders increased with patients' age (P < 0.02). However, a statistically significant increase of post-OLT hearing impairment with age was not found (P = 0.3).
| Patients' characteristics | Hearing impairment | Total | P | ||
|---|---|---|---|---|---|
| Post-OLT | Pre-OLT | No | |||
| Risk factors (%) | 88% | 88% | 92% | 90% | |
| Ototoxic drugs | 31% | 40% | 31% | 32% | |
| Renal failure | 69% | 70% | 72% | 71% | |
| Arterial hypertension | 64% | 65% | 73% | 70% | † |
| Diabetes mellitus | 16% | 19% | 16% | 16% | |
| Exposition to noise | 2% | 5% | 0% | 1% | *, † |
| Immunosuppression (%) | |||||
| Cyclosporine A | 81% | 84% | 83% | 83% | |
| Tacrolimus | 30% | 49% | 32% | 33% | * |
| Prednisolone | 91% | 86% | 93% | 92% | |
| Mycophenolate mofetil | 35% | 53% | 33% | 35% | * |
| Sirolimus | 3% | 2% | 2% | 2% | |
| Azathioprine | 17% | 9% | 18% | 17% | |
- NOTE. Subgroups are patients with hearing impairment occuring after liver transplantation (post-OLT), prior to OLT (pre-OLT) and patients without hearing impairment (no).
- Abbreviations: OLT, orthotopic liver transplantation.
- * P < 0.05 between patients with preexisting hearing impairment and other patients.
- † P < 0.05 between patients with no hearing impairment and other patients.
Hearing loss was reported as severe in 45 of 73 patients (62%). In 15 of 73 patients (21%), it was described as moderate. In the remaining 13 patients (18%), hearing loss had already disappeared at the time of evaluation. Sudden hearing loss was the cause of hearing impairment in 19 of 73 patients (26%). In 49% of patients (36/73), hearing loss occurred within 2 yr post-OLT. Hearing loss was associated with the use of tacrolimus immunosuppression (35% of patients with hearing loss received tacrolimus vs. 20% of patients with other hearing defects; P < 0.05; Fig. 3). Multivariate analysis was performed with hearing loss as a dependent variable. Patients' gender and age, indication for OLT, follow-up time since OLT, presence of exogenic risk factors, as well as use of the different immunosuppressants were used as independent variables. Length of follow-up since liver transplantation (P < 0.001) and use of tacrolimus (P < 0.02) were the only independent factors positively associated with hearing loss (R2 = 0.12; P < 0.001).
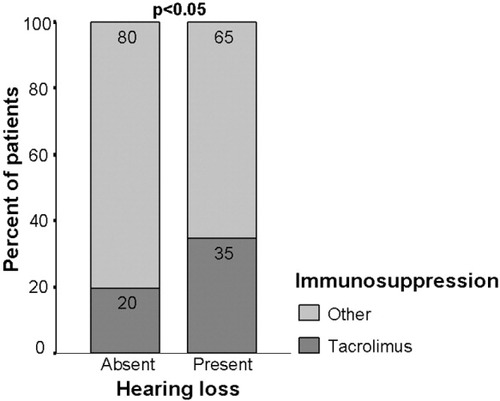
Hearing loss and tacrolimus immunosuppression. Shown is the percentage of patients with (n = 73) or without (n = 68) hearing loss. Hearing loss was associated with the use of tacrolimus immunosuppression (P < 0.05).
A total of 16 patients (11% of patients with hearing impairment after OLT) developed need of a hearing aid post-OLT. In 14 of them (88%), the hearing aid was bilateral. Principal immunosuppression equally consisted of cyclosporine A and tacrolimus (each 50% of patients). Thus, the proportion of patients receiving tacrolimus was significantly higher compared to control patients (28%; P < 0.05).
DISCUSSION
This is the first clinical study to systematically evaluate hearing impairment in adults after organ transplantation. We found a high incidence of hearing disorders in a large cohort of nearly 700 patients with long follow-up periods after liver transplantation. A high rate of response to the questionnaire (75%) ensured a small risk for statistical bias in the study. However, these data are based only on patients' self-reports without any objective analysis of hearing function. The most frequently reported subjective hearing problems after liver transplantation were hearing loss, tinnitus, and otalgia, often in combination. Use of tacrolimus immunosuppression was positively associated with hearing loss in uni- and multivariate analyses. There was no increasing prevalence of hearing impairment with age, as it is usually found.1
Two studies evaluated risk factors for hearing loss in pediatric patients after OLT without addressing the possible role of immunosuppression. Hearing loss was found in 12–15%.18, 19 In adults, one study found hearing and vestibular disorders in 5% of the patients under cyclosporine A 18 months after renal transplantation.20 To date, there is only one published case report suggesting an association of chronic hearing impairment after transplantation with immunosuppression.17 In contrast, a number of case reports have presumed an association of sudden hearing loss with a variety of immunosuppressants.12-16 In nearly all of them, dose correction or switching led to full hearing recovery. In our study, reversibility of hearing impairment was reported only in few cases. In agreement with the above-described cases, these were almost all episodes of sudden hearing loss.
Potential pathophysiological mechanisms linking the high incidence of hearing impairment after liver transplantation with immunosuppression include cardiovascular side effects as well as direct neurotoxicity. Cardiovascular effects may act directly, such as vasculopathy of the inner ear, or indirectly, such as auditory sequelae to systemic arterial hypertension or renal failure. However, a significant association of arterial hypertension, renal failure, or diabetes mellitus with hearing impairment was not detected by our study. Therefore, our data are in favor of a calcineurin inhibitor-associated neurotoxicity leading to hearing impairment. Neurotoxic side effects such as tremor may be found in up to 50% of patients and are usually dose dependent.10, 11 Levels of immunosuppressive drugs are kept higher in the early period following transplantation. Likewise, hearing impairment began early after liver transplantation in about 50% of our patients. However, as dose-independent neurotoxicity is known to occur as well, it may be related to hearing impairment later in follow-up. There is evidence that calcineurin inhibitor-related neurotoxicity is caused by endothelial damage and vasculopathy disturbing the blood-brain barrier. Regarding hearing impairment, vascular damage of capillary endothelial cells of the inner ear disturbing the blood-inner ear barrier may be hypothesized.21 In accordance to the literature, other immunosuppressants did not play an important role in our study.
Up to now, hearing impairment was not in the focus of clinical care for patients after liver transplantation. With the evidence of our study, hearing impairment should be added to the list of important side effects of immunosuppressants. Further prospective investigations are necessary to confirm these data by objective hearing tests and to evaluate the role of immunosuppressants. In addition, our findings should be confirmed in patients after transplantation of other organs.