A national curriculum and community of practice for health services and policy research training: Insights from the Health System Impact Fellowship National Cohort Training Program (HSIF NCTP)
We acknowledge the many individuals and organizations who have contributed to the HSIF NCTP [Co-Applicants on CIHR Grant Application: Iwona Bielska, Marcia Bruce, Ivy Cheng, Jawad Chishtie, Shelley Cook, Celine Cressman, Tawyna Crowshoe, Greta Cummings, Gillian Currie, Malcolm Doupe, Clayon Hamilton, Robin Hayeems, Lindsay Hedden, Jia Hu, Noah Ivers, Lauren Jewett, Daman Kandola, Malcolm King, Andriy Koval, Tatiana Kuzmyn, Jonathan Lai, Celia Laur, Danielle Lavallee, Jeanna Parsons Leigh, Shannon MacDonald, Jean-Sébastien Marchand, Ellen Rafferty, Chantelle Recsky, Kwestan Safari, Maria Jose Santana, Deepa Singal, Katelyn Tate, Jeanette Van Roosmalen, Daniel Warshafsky, Cynthis Weijs, Jennifer Zwicker. Collaborators: Stephen Bornstein, Adalsteinn (Steini) Brown, Jamie Day, Christine Friedenreich, William Ghali, Carmen Grabusic, William Hall, Brenda Hemmelgarn, Catherine Keogh, Gail MacKean, Dev Menon, Tim Murphy, Angelo Nwigwe, Victoria Shuckel, Tom Stelfox, Andriy Strogan, Kathryn Todd, Marcello Tonelli, Ross Wallace, Verna Yiu. Organizations: University of British Columbia, BC Academic Health Science Network (BC AHSN), University of Calgary, Alberta Health Services Strategic Clinical Networks (AHS SCNs™), University of Regina, University of Manitoba, IMAGINE Chronic Disease Network, Michael Smith Foundation for Health Research (MSFHR), University of Calgary Cumming School of Medicine, University of Calgary O'Brien Institute for Public Health, Alberta Innovates, Mitacs, Canadian Association for Health Services and Policy Research (CAHSPR), Canadian Health Services & Policy Research Alliance (CHSPRA), BC Ministry of Health, IMAGINE CITIZENS Collaborating for Health, Alberta Health Services, Alberta Health, University of Alberta, University of Calgary Patient and Community Engagement Research (PaCER) Patient Program, University of Saskatchewan, Saskatchewan Centre for Patient-Oriented Research (SCPOR), University of Toronto, Women's College Hospital, Santis Health, GlaxoSmithKline, Juniper, Chief Medical Officer of Health Ontario, Dalhousie University, Memorial University, Science to Business Network, Vanto Group, ISPOR—The Professional Society for Health Economic and Outcomes Research.]
Abstract
This overview outlines the development and implementation of the Health System Impact Fellowship (HSIF) National Cohort Training Program (NCTP)—a national training program for embedded health services and policy research (HSPR) in Canada. The program aims to improve HSPR capacity and make a recognizable impact within health systems. The HSIF NCTP aimed to achieve three specific goals related to advancing the community of practice in health services research: (1) providing tools and learning opportunities in HSPR competency areas, enabling the CoP to advance learning health systems nationally; (2) creating deliberate, ongoing networking opportunities that encourage diverse HSIF members to engage meaningfully, thereby strengthening community of practice collaboration; and (3) laying the groundwork for the evolution and sustainability of the community of practice within Canada's integrated HSRP ecosystem. Analysis of the program's evolution reveals critical elements to its development and implementation, including but not limited to adaptive learning environments that respond to emerging needs, cross-sectoral collaboration fostered through mentorship, and balanced instructional formats that combine theoretical depth with practical application. The curriculum, co-developed by fellows and faculty, emphasizes critical analysis of complex health system challenges. Insights from implementing and refining the program offer valuable lessons for developing embedded research training initiatives in healthcare settings.
Abbreviations
-
- AHRQ
-
- Agency for Health Research and Quality
-
- CHSPRA
-
- Canadian Health Services and Policy Research Alliance
-
- CIHR
-
- Canadian Institutes of Health Research
-
- CIHR-IHSPR
-
- Canadian Institutes of Health Research—Institute of Health Services and Policy Research
-
- CoP
-
- Community of Practice/Communities of Practice
-
- E&A
-
- Evaluation and Assessment
-
- ECR
-
- Early Career Researcher
-
- HSIF
-
- Health System Impact Fellowship
-
- HSPR
-
- Health Services and Policy Research
-
- LHS
-
- Learning Health Systems
-
- LTE
-
- Learning and Training Exchange
-
- NCR
-
- National Cohort Retreat
-
- NCTP
-
- National Cohort Training Program
-
- PDSA
-
- Plan-Do-Study-Act
-
- TMWG
-
- Training Modernization Working Group
1 INTRODUCTION
Health systems worldwide face increasing pressures to deliver high-quality services and achieve better patient outcomes to achieve the equity-informed quadruple aim of improving population health, enhancing patient experience, reducing costs, and supporting the well-being of care teams.1-3 Learning health systems represent a systemic paradigm shift in processes and priorities, whereby research is integrated within operational objectives amidst budget constraints and other systemic challenges.4-8 This transition necessitates changes in health services and policy research (HSPR) education to equip graduates with the knowledge and skills needed to excel outside traditional academic settings.9, 10 This educational shift also calls for emphasizing hands-on learning, embedding learners in real-world healthcare environments, and creating supportive infrastructure for non-academic roles and career paths.7, 11
In recent years, there has been a significant shift in the perception of non-academic career pathways within health services and policy research.9, 12 Many professionals are now pursuing careers focused on driving improvements in health systems and implementing substantive changes within healthcare settings.9, 13-15 This trend is partly due to a shortage of academic positions, prompting many individuals to seek impactful roles outside traditional academia. Concurrently, health system organizations in Canada are evolving into learning organizations, leveraging evidence to inform policy implementation.9, 16 This evolution has highlighted a growing demand for embedded research expertise, as evidenced by the creation of dedicated divisions for research and evaluation within federal and provincial governments, health professional associations, and other health authorities.9, 17
In response, the Canadian Institutes of Health Research—Institute of Health Services and Policy Research (CIHR-IHSPR) collaborated with the Canadian Health Services and Policy Research Alliance (CHSPRA) in 2015 to develop a comprehensive pan-Canadian strategy to enhance training in HSPR environments.18, 19 A direct outcome of this collaboration was the launch of the Health System Impact Fellowship (HSIF) in 2017, providing post-doctoral fellows (with the addition of doctoral trainees for subsequent years) specializing in HSPR with a unique opportunity for experiential learning as embedded researchers in health organizations addressing real-world challenges.12, 20
The fellowship facilitates embedded-research placements in health system organizations, fostering collaborations with universities to accelerate evidence-informed health system transformation.10 To date, 328 fellows (111 PhD trainees and 217 postdoctoral researchers) and 12 early-career researchers have participated in HSIF placements, spanning 139 health system organizations and 25 universities. This diverse group represents a wide range of scientific and clinical disciplines (e.g., epidemiology, nursing, health economics, implementation science).21
CIHR-IHSPR established the HSIF program as a dyad mentorship model with an academic supervisor and health organization supervisor for each fellow. This dual-supervisory structure was retained throughout the NCTP and was supplemented with targeted mentorship skill-building sessions. This included select workshops in the curriculum sessions to provide guidance to fellows on setting clear expectations with their academic and health system mentors, and in-person roundtable sessions with fellows and their mentors at the annual National Cohort Retreat events on topics like implementation barriers and stakeholder engagement. Fellows received direct training on managing triadic relationships, ensuring they could leverage both academic and health system perspectives to advance research and practice goals. Tailored activities also supported cross-mentor networking, enabling fellows to engage with multiple subject-matter experts and expand their mentorship support beyond the HSIF dyad. In addition, the annual orientation session, hosted by CIHR-IHSPR and the HSIF NCTP for incoming fellows and both their mentors, included a seminar on mentorship and allyship by an external expert. A separate session at the annual National Cohort Retreat was also scheduled for mentors to share experiences and practice tips about mentorship in general and specifically in the context of the dyadic mentorship model of the HSIF.
The HSIF program had three primary objectives: (1) develop impact-focused career pathways; (2) expand traditional training environments beyond academia by supporting experiential learning opportunities and the development of key professional competencies needed to succeed in healthcare organization environments; and (3) provide health systems with direct access to research-trained individuals supported by academic partnerships.15, 22
2 QUESTION(S) OF INTEREST
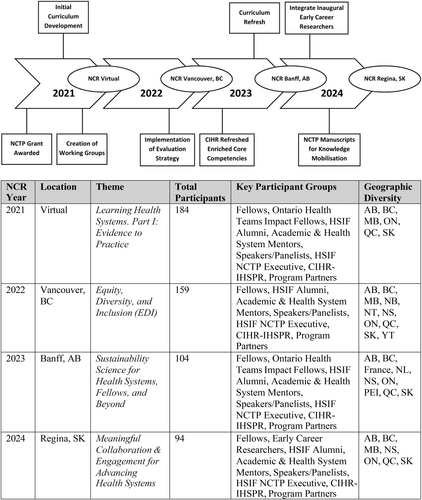
Building on early program success, CIHR-IHSPR sought to expand its support for the HSIF program in 2021 by transitioning its leadership of training activities to an external HSIF National Cohort Training Program (NCTP)23 (Figure 1). The HSIF NCTP was established to complement the HSIF program by enhancing the fellowship experience. It achieved this through a structured, cohort-based learning model bringing together fellows, academic mentors, and health system leaders in an integrated learning community that supported both individual growth and collective capacity building for health system transformation. While fellows gained hands-on learning experiences through their health system placements, the HSIF NCTP provided a collaborative platform for developing additional HSPR competencies and sharing insights across cohorts to support an active HSPR community of practice. The purpose of this overview paper is to describe the development and implementation of the HSIF NCTP, with particular attention to its role in advancing embedded HSPR training and advancing learning health systems. It also highlights the key training elements that facilitated the successful integration of research capacity within health systems.
3 METHODS
3.1 Overview, theoretical framing and objectives of the NCTP
The collective goal of the HSIF NCTP was to deliver a comprehensive training program that cultivated leadership competencies necessary for addressing complex health system challenges with evidence-based solutions. The HSIF NCTP leveraged the concept of Communities of Practice (CoP)24 to create both independent and collaborative learning opportunities in keeping with the HSIF NCTP's mandate to sustain and strengthen an active CoP within the Canadian HSPR landscape. This CoP approach created opportunities for knowledge exchange between fellows, academics, and health system leaders across different organizations and jurisdictions. Thus, more specifically, the HSIF NCTP aimed to achieve three specific CoP-related goals: (1) providing tools and learning opportunities in HSPR competency areas enabling the CoP to advance learning health systems nationally; (2) creating deliberate, ongoing networking opportunities that encourage diverse HSIF members to engage meaningfully, thereby strengthening CoP collaboration; and (3) laying the groundwork for the evolution and sustainability of the CoP within Canada's integrated HSRP ecosystem. Consistent with the concept of effective learning through a continuous cycle of concrete experiences and reflective observation,25 the embedded nature of the HSIFs in health systems enabled the application of theoretical insights gained through the NCTP to develop additional HSPR competencies and address real-world challenges. Through regular virtual and in-person training activities, participants engaged in collaborative learning while building a professional network that supported their development as embedded researchers.
The HSIF NCTP was shaped by an interdisciplinary team of health system leaders, academics, and HSIF alumni, drawing on HSPR and educational frameworks. Central to the framing of HSIF NCTP training activities were the core competencies in HSPR developed by CIHR-IHSPR for the HSIF (Table 1), which defined essential capabilities for researchers working within health systems. The HSIF NCTP's use of this framework allowed the program to emphasize competencies essential for HSPR graduates to effectively navigate the complexities of healthcare environments. From an educational standpoint, the HSIF NCTP's pedagogical approach incorporated principles from Competency-Based Medical Education, which emphasized outcomes-oriented learning tailored to specific learner needs.26, 27 This framework helped structure learning activities that built specific skills required for embedded research roles. The HSIF NCTP also drew on adult learning theory,27 recognizing fellows as experienced professionals who brought valuable perspectives to collective discussions.
| Framework (year) | Competency | Brief description |
|---|---|---|
| Enriched Core Competency Framework (2015) | Analysis & evaluation of health and health-related policies and programs | Conduct formativesummative evaluations linked to organizational planning; integrates technical, contextual and communication skills. |
| Analysis of data, evidence and critical thinking | Collect, analyze and synthesize diverse datasets (administrative, economic, big data) to frame problems and implementation options. | |
| Understanding health systems and the policy making process | Deep understanding of Canadian and global healthpolicy structures and decision pathways. | |
| Knowledge translation (KT), communication and brokerage | Tailor research evidence for multiple audiences using varied KT methods and channels. | |
| Leadership, mentorship & collaboration | Mobilize and guide multidisciplinary teams toward shared deliverables. | |
| Project management | Plan, resource and deliver projects through to knowledge exchange in academic and practice settings. | |
| Interdisciplinary work | Combine theories and methods from multiple disciplines to address complex questions. | |
| Networking | Build and sustain crosssector relationships inside and outside academia. | |
| Dialogue & negotiation | Achieve win–win outcomes through active listening, perspectivetaking and consensusbuilding. | |
| Change management and implementation | Design, lead and evaluate organizational change initiatives. | |
| Refreshed Enriched Core Competency Framework (2024) | Equity, diversity, inclusion, accessibility and antioppression | Integrate EDIA principles and intersectionality to advance equitable, antioppressive health research and practice. |
| Indigenous cultural safety and humility | Engage with Indigenous Peoples through culturally safe, antiracist research and partnerships. | |
| Leadership and mentorship | Inspire shared vision, sponsor emerging talent and cultivate continuous learning cultures. | |
| Innovation, implementation, and improvement | Generate and scale evidenceinformed innovations using implementation/improvement science to strengthen LHS capacity. | |
| Engagement, collaboration, and partnership | Design culturally safe, inclusive engagements and build productive intersectoral networks. | |
| Project management | Coordinate projects and portfolios from conception to dissemination, anticipating risk. | |
| Communication | Convey complex evidence clearly and persuasively to diverse audiences. | |
| Knowledge mobilization | Coproduce and integrate research with other ways of knowing to inform policy and practice. | |
| Health systems, policy processes, and systems science | Apply systems perspectives to adapt evidence within sociopolitical and economic contexts. | |
| Research and evaluation | Formulate relevant questions, select rigorous methods ethically and appraise evidence for actionable solutions. | |
| Data science | Extract, analyze and interpret multisource data (e.g., electronic health records, administrative, lived experience) to drive system improvement. |
- Note: Adapted from Canadian Institutes of Health Research (2025, April 1), Refreshed enriched core competency framework for health services and policy research (https://cihr-irsc.gc.ca/e/49883.html). Copyright 2025 by the Canadian Institutes of Health Research.
The NCTP strove to reflect the competencies in the development of the training curriculum and delivery of the sessions in keeping with their relevance in learning health systems and the objective of the overall HSIF program. The TMWG core competencies are broadly similar to those developed by the Agency for Health Research and Quality (AHRQ) in the United States, although the domain grouping of the competencies differs, and the TMWG specifically includes a competency on Indigenous Cultural Safety and Humility. In the updated competency framework from 2022, AHRQ includes a total of 38 core competencies prioritized across eight domains.28
3.2 Structure of the NCTP
The governance of the HSIF NCTP consisted of an Executive Committee, Advisory Committee, and several Working Groups, each of which fulfilled distinct roles in overseeing and directing the program. The HSIF NCTP was led by the Executive Committee and, through the Advisory Committee and Working Groups, supported by a broader consortium of co-investigators and collaborators from across Canada.
The Executive Committee, including HSIF alumni and mentors, was the primary decision-making body. The committee met monthly for decision-making and maintained continuous communication to support activities between meetings. The Advisory Committee, which included fellows, patients, and health system leaders, convened biannually with the Executive Committee to provide broad-based guidance on key considerations regarding the role of the NCTP within the Canadian HSPR ecosystem and approaches to sustainability. Supporting this governance structure was a dedicated NCTP Program Manager.
Furthermore, two Working Groups were established: (1) the Evaluation and Assessment (E&A) Working Group, tasked with designing and executing the program's evaluation framework; and (2) the Sustainability Working Group, initially focused on ensuring the program's long-term viability and exploring future opportunities for the Community of Practice (CoP). Over time, the latter evolved into the Learning and Training Exchange (LTE) Working Group, emphasizing practical application and collaborative curriculum design. The LTE Working Group assumed responsibility for aligning training activities with the overarching goals of the HSIF program.
Overall, this consortium encompassed the complete NCTP governance network—comprised of the Executive Committee, Advisory Committee, and two Working Groups (Evaluation and Assessment Working Group and Learning and Training Exchange Working Group) and the annual NCR Planning Committee—together with the extended group of co-investigators and collaborators. In total, 65 members from eight provinces participated, including 22 HSIF fellows and alumni, 14 HSIF mentors, and representatives from healthcare organizations, academic institutions, patient advocacy groups, and health system leadership. This structure enabled strategic partnerships across multiple groups, including (1) patients, patient researchers, and patient-focused organizations; (2) health system leaders; (3) university-based academics; (4) representatives from funding institutions; (5) professional development and training companies; (6) public and government relations firms; (7) private sector and industry representatives; and (8) non-governmental organizations.
With travel funding provided through IHSPR to enable and encourage full participation by HSIF fellows, core program activities included regular virtual learning sessions and an annual National Cohort Retreat. These activities were designed to facilitate cross-cohort collaboration and knowledge exchange while building networks that support embedded research careers.
4 RESULTS
4.1 Guiding principles
A commitment to continuous improvement was central to the HSIF NCTP, supported by a structured framework that emphasized inclusivity, a fellow-driven ethos, competency-based methodologies, and co-creation. These principles shaped both program structure and implementation. At the heart of the program was an iterative improvement process using the Plan-Do-Study cycle that engaged HSIF alumni, mentors, and current fellows in design, implementation, and evaluation, ensuring the training activities evolved to meet changing educational complexities in health systems and the related needs of the fellows and their learning expectations demands.
Training opportunities were developed through sustained interaction among HSI fellows, alumni, mentors, and NCTP committee members facilitated through co-creation and continuous evaluations of NCTP sessions and events. Through this collaborative process, strategies and co-created activities were proposed, ensuring alignment with the needs of learners and the HSPR CoP participants. The NCTP grant team—including current and alumni fellows, alongside academic and health system supervisors—shaped the program's trajectory. The NCTP actively embraced diverse viewpoints from across the educational spectrum, supported by experienced team leads and supplementary training. By employing inclusive practices, trainee perspectives were meaningfully incorporated at all project stages, guiding decision-making and program development.
4.2 Curriculum development and learning exchange: innovative learning framework
The NCTP had expanded to include a wide array of training events and activities to align with the enriched core competencies established by the CIHR-IHSPR Training Modernization Working Group (TMWG) (Table 1).9, 18 To implement these competencies effectively, the program established the Learning and Training Exchange Working Group (LTE-WG) which included current HSI fellows, alumni, and academic and health system mentors. The LTE-WG operationalized these competencies within the NCTP through a structured, competency-based learning framework aligned with the TMWG enriched core competencies and supported the professional development of emerging research leaders in HSPR.
At the foundation of the curriculum was a set of four complementary modalities offered each quarter, allowing for both conceptual breadth and practical depth. Specifically, each theme included one to two sessions drawn from (1) professional development presentations (1–2 h, expert-led); (2) skill-building workshops (3–6 h, professional-led); (3) Career Cafés (fellow-led, focusing on mentorship and career navigation); and (4) networking “happy hours” (1–2 h, also fellow-led) (Table 3). Guest facilitators from health system organizations regularly contribute to these sessions, covering topics such as leadership, project management, collaboration, and knowledge translation. These educational opportunities aimed to prepare and empower fellows in implementing meaningful changes in the health system and contributing to evidence-informed decision-making.
The Professional Development sessions and workshops were deliberately designed to integrate academic (didactic) content with operational (practice-based) learning to ensure both conceptual understanding and practical application. This integration occurred through a structured approach that combined expert-led instruction, collaborative exercises, and contextualized practice.
Workshop sessions followed a consistent structure: introduction to key concepts, interactive demonstrations, collaborative practice, and contextual application and reflection. Workshops targeted both technical and interpersonal skills, and to ensure relevance across diverse operational environments, the workshops often incorporated case studies, breakout groups, and encouragement of cross-disciplinary dialogue to foster adaptive thinking.
For example, Theme 1 in the NCTP curriculum was ‘Strong Start,’ which was focused on two of the professional skills competencies of Project Management and Leadership from the TMWG Core Competency Framework (Tables 2 and 3). This was delivered as a workshop for the delivery mode through a professional consultant with academic credentials with the aim of applied skill-building and included both didactic academic content and practice-based learning through hands-on exercises using project management tools and interactive discussions in breakout sessions with subsets of the workshop participants.
| Original NCTP Curriculum | |||
|---|---|---|---|
| Theme number | Theme name | Competencies | Theme objectives |
| 1 | Strong Start | -Project Management -Leadership, Mentorship & Collaboration |
To provide participants with a comprehensive understanding of the key aspects of health system impact, setting the stage for further learning and skill development throughout the program. The goal is to establish a strong foundation for participants to effectively navigate the health system and initiate meaningful changes in their respective roles as emerging health system leaders. |
| 2 | Learning Health Systems Part 1: Evidence to Practice | -Knowledge Translation, Communication and Brokerage -Analysis & Evaluation of Health & Health-Related Policies and Programs |
To enhance participants' understanding of the principles, processes, and strategies involved in using research evidence, engaging in knowledge translation, and implementing evidence-based interventions to drive meaningful changes within the context of learning health systems. |
| 3 | Informing Policy | -Understanding Health Systems and the Policy Making Process -Analysis of Data, Evidence and Critical Thinking -Dialogue & Negotiation -Networking |
To enhance participants' understanding of the policy development process and equip them with the skills and knowledge to engage with policymakers, advocate for evidence-informed policies, and contribute to policy change within the health system that improves health outcomes. |
| 4 | Breaking Silos: The Art & Science of Leadership | -Leadership, Mentorship & Collaboration -Networking -Dialogue & Negotiation |
To develop participants' leadership capabilities by enhancing their understanding of effective leadership principles, strategies, and skills, and empower them to lead and drive transformative changes in the health system. |
| 5 | Patient-Oriented Research: Partnering with Partners with the Most at Stake |
-Interdisciplinary Work -Dialogue & Negotiation |
To enhance participants' understanding of Patient-Oriented Research (POR) and the importance of engaging partners, particularly those with lived experiences, in the research process. Participants will be equipped with the knowledge and skills to effectively engage patients, caregivers, and other partners in research partnerships, ensuring that research is patient-centered, relevant, and impactful. |
| 6 | Equity, Diversity & Inclusion: Thoughtful Representation Matters | -Understanding Health Systems and the Policy Making Process -Leadership, Mentorship & Collaboration -Indigenous Cultural Safety and Humility |
To enhance participants' understanding of equity, diversity, and inclusion (EDI) principles within the context of health system impact, by equipping them with the knowledge and skills to address systemic inequities, promote inclusivity, and foster thoughtful representation in their work as emerging health system leaders. |
| 7 | Demonstrating Impact | -Knowledge Translation, Communication and Brokerage |
To equip participants with the knowledge and skills to effectively measure, evaluate, and communicate the impact of their health system impact initiatives. It aims to enhance participants' understanding of evaluation methods, outcome measurement, and knowledge dissemination strategies so that they can demonstrate the effectiveness and value of their work. |
| 8 | Learning Health Systems Part 2: Implementation Science |
-Change Management and Implementation | To deepen participants' understanding of implementation science principles and methods within the context of health system impact, by equipping them with the knowledge and skills to effectively plan, execute and evaluate the implementation of evidence-based interventions and drive sustainable changes in the health system. |
| Training delivery modality | Description | Goal/objective |
|---|---|---|
Professional Development Session Expert led |
Panel session or invited speaker presentation to discuss a topic of interest. | -Provide overview of the topic and discuss the topic with attendees. |
Workshop Professional led |
An intensive educational session. | -To Provide in-depth training to develop and/or practice a skill or expertise. |
Networking Happy Hour Fellow led |
A PI-fellow from the grant will facilitate an evening networking session. The theme of the “happy hour” will correspond to the quarterly theme. The fellow will structure the session using innovative facilitation techniques to generate dialogue and meaningful interactions. Group peer-mentorship session or other format networking activities. |
-To foster a sense of togetherness, camaraderie and connection among current and alumni fellows. -To facilitate deliberate networking opportunities for fellows to collaborate on current or future projects. -To provide specific opportunities for the alumni and fellow community to design and lead sessions that advance this community of practice. |
Career Café/Lunch and Learn Co-organized |
A series of lunch and learn sessions from experts in sectors in which fellows may seek a career:
|
-To bolster fellows career preparedness for careers in various sectors aligned with HSIF core competencies. -To introduce fellows to leaders in prospective career paths/fields and be exposed to non-traditional academic career trajectories. |
Another example is Theme 2—Learning Health Systems Part 1: Evidence to Practice. In this theme, sessions focused on the two research and analytic competencies of ‘Knowledge Translation, Communication & Brokerage’ and ‘Analysis & Evaluation of Health & Health-Related Programs & Policies’ from the TMWG Core Competency Framework (Tables 2 and 3). The sessions included Professional Development Session led by an expert in the field around the topic of ‘Are we ready to implement evidence to practice,’ and a Networking Happy Hour lead by one of the HSI fellows on the topic of ‘The building blocks of value-creating learning health systems.’ Similarly, this format provided opportunities to integrate academic content with applied content and learning through a variety of interactive formats with experts and learners from different backgrounds, in different settings and with different degrees of experience.
Some of the sessions in the first 2 years of the NCTP were designed to reflect competencies from the forthcoming refreshed Enriched Core Competencies developed by the TMWG. These competencies were included in the curriculum based on discussions and feedback from both the NCTP Executive Committee and the NCR Planning Committee. Several members of the NCTP Executive Committee were also directly involved in the TMWG, which enabled early integration of the refreshed competencies into session planning. As a result, while some session objectives may not align directly with the original competency framework in Table 1, they reflect an intentional effort to align with the updated direction of competency development.
4.3 Training design and chronology
In the initial 2 years of the NCTP, the curriculum was organized around eight central themes (Table 2). Each quarterly theme included multiple events that reinforced core competencies and facilitated networking (Table 3). Continuous feedback revealed a need to reconfigure the curriculum to avoid repetition and maintain high engagement. In September 2023, in alignment with the newly revised 2024 competencies (Table 2), the NCTP transitioned to a ‘refreshed’ 2-year curriculum featuring four quarterly themes each year (with the themes repeated across 2 years). While the same four themes anchor both years, the specific content and learning objectives for each theme evolve in the second year, building on foundational skills introduced in the first. This cyclical approach ensures fellows encounter new content and build upon previously acquired knowledge over time. ‘Strong Start (Project Management & Leadership)’ remained central in both years due to its foundational importance.29
4.4 National cohort retreat
The annual National Cohort Retreat (NCR) was a flagship event of the NCTP, bringing together current fellows, alumni, and their academic and health system mentors for intensive learning and network building. Each annual retreat was organized by a dedicated Planning Committee comprising NCTP leadership, fellows, and alumni, who collaborated to select the retreat theme and co-designed, planned, and executed the two-day event. The chair role rotated among the NCTP Co-Principal Investigators, ensuring the retreat's alignment with the broader training objectives of the NCTP through the NCR—fostering engagement, professional development, and cross-sector collaboration.
The NCR was a cornerstone event designed to foster engagement and dynamic interaction, professional development, knowledge sharing, and collaboration among fellows, health system supervisors, and academic mentors across all cohorts. Spanning two full days, the retreat was strategically structured to provide immersive activities, panel discussions, and networking opportunities that strengthened connections within the cohort and with external partners.
By harnessing the expertise of HSPR leaders, the National Cohort Retreat (NCR) became a pivotal vehicle for expanding the Community of Practice (CoP) within the HSIF. Tactics to advance NCR goals included the participation of esteemed guests and speakers nationally and globally and engaging with diverse perspectives and innovative approaches during interactive sessions and workshops. This infusion of external expertise amplified the impact and reach of the HSIF CoP within the HSRP ecosystem.
The retreats evolved through different delivery formats in response to changing circumstances. The inaugural 2021 retreat was held virtually, followed by a hybrid model in 2022 that combined in-person Vancouver regional gatherings with virtual connections across sites. In 2023, the program transitioned to a full in-person format in Alberta and in 2024 in Saskatchewan, with travel support provided to ensure nationwide participation. The retreat structure balanced formal learning with relationship building through carefully sequenced activities. Morning plenary sessions typically featured Canadian health system leaders discussing emerging priorities, followed by interactive workshops where fellows practiced specific skills with expert facilitators. Dedicated networking periods allowed fellows to connect with potential collaborators and mentors, while evening social events rounded out the day to strengthen informal connections within the developing community of practice. The combination of structured learning and collaborative knowledge exchange created multiple pathways for participant skill development.
4.5 Evaluation and assessment
The Evaluation and Assessment Working Group was responsible for assessing the NCTP program and guiding improvements to the NCTP curriculum. The evaluation strategy centered on the Kirkpatrick Evaluation Model,30 which examined four levels of educational impact—ranging from learner reactions to training sessions through to long-term organizational impact. Through iterative assessments guided broadly by the Plan-Do-Study-Act (PDSA) cycle,31-33 the Evaluation Working Group administered regular surveys to measure reactions, learning, behaviors, and impact—enabling rapid adjustments to program content and delivery. These evaluations yielded valuable insights into the NCTP curriculum's strengths and weaknesses, informing targeted enhancements over time. A detailed report including participation, and both quantitative survey responses and qualitative comments through open-ended questions was analyzed quarterly for the training events in each theme and for each NCR event and approved by the NCTP Executive Committee. The comments from the NCR were used to inform the planning committee for the next NCR event. For example, fellows expressed a specific desire for unstructured or semi-structured sessions during the NCR to further cultivate connections and facilitate informal knowledge-sharing, which served as catalysts for improvements in their local health system or at a larger scope.
The performance of fellows with regard to their competencies and impacts, as well as the long-term organizational outcomes, is tracked annually by the CIHR IHSPR, which administers the HSIF awards program and the associated reporting. This includes tracking the number of fellows, their placements, their subsequent employment and career paths, and contributions to organizational goals. In addition, each HSI fellow and their academic and health system mentors are invited to complete pre- and post-assessments and provide qualitative impact statements to document competency development and perceived value to the system19, 21
5 DISCUSSION: REFLECTIONS ON KEY LEARNINGS AND INSIGHTS
This overview of the HSIF NCTP described the program's core objectives, approaches applied, and key achievements, as well as the co-design of the NCTP's curriculum and evaluation approaches. The NCTP, co-designed with trainees and mentors, had established a dynamic and collaborative learning environment that not only facilitates critical thinking but also helped equip future leaders to navigate and advance the complex Canadian health system.
A central element of the NCTP was its focus on a sustainable CoP, which posited that learning is fundamentally a social process occurring within communities in which members share common goals and engage in collaborative learning. Through shared experiences, resources, and best practices, NCTP participants exchanged knowledge and collaborated in problem-solving, preparing them for life-long learning.
- Dynamic Learning Environment that Evolved Over Time: A key takeaway from the NCTP was the importance of cultivating a dynamic learning environment with a longitudinal perspective. In a rapidly changing health system, adaptability and continuous learning were essential. The program's design and evolution, informed by the PDSA cycle,31-33 ensured that both content and delivery methods remained flexible and responsive to emerging trends and needs.
- Cross-Sectoral Perspectives: Diverse engagement and networking strategies exposed participants to a wide array of viewpoints from multiple sectors, including academia, healthcare delivery organizations, and policy-making bodies. Such exposure enabled fellows to develop holistic perspectives on health system challenges and solutions at the macro (system), meso (organization) and micro (individual team) levels. This breadth of viewpoints ignited innovative problem-solving approaches and enriched discussions.
- Nurturing a Supportive Atmosphere: Fostering a supportive atmosphere was integral to the program's effectiveness. By cultivating an inclusive space for learning with multiple formats and explicit engagement activities, the NCTP encouraged open exchange of ideas and experiences among fellows. This culture of openness allowed participants to discuss challenges candidly, share insights, and offer mutual support, thereby enhancing individual learning experiences and building a network of professionals across the country who are committed to collaborative health system improvements. This was one of the key opportunities that was emphasized in planning the content of the retreats.
- Interactive Engagement Formats:Beyond conventional training approaches, highly interactive sessions were instrumental in participant engagement in the virtual NCTP training sessions and the in-person NCR events. The vitality of face-to-face interaction was apparent at the NCRs, highlighting positive nurturing relationships and contributing to a sense of camaraderie among fellows. In-person encounters provided invaluable opportunities for meaningful interactions, networking, and the organic exchange of ideas.
- Balancing Depth and Scope: Striking an optimal balance between depth of content and session frequency emerged as an important priority for maximizing program effectiveness and participant engagement. HSIFs preferred fewer, more impactful sessions, emphasizing the value of in-depth content exploration. This aligns with adult learning theories that stress practical application and relevance to learners' professional contexts, as well as the need to accommodate busy schedules.
- Embracing Co-Design Approaches: Empowerment through co-design ensured alignment with unique learning needs and preferences. This participatory model fostered a sense of ownership and engagement among participants, while allowing for diverse perspectives that enriched the curriculum and made it more responsive to the evolving demands of the healthcare sector.
- Foundational Role of Critical Thinking: Critical thinking emerged as a core skill throughout the program, enabling fellows to dissect complex issues and formulate evidence-based solutions. This competency was enhanced through a variety of interactive sessions and peer/alumni engagements, in both structured and unstructured formats, across the program's duration.
Despite its strengths, the NCTP faced several challenges that warranted attention to ensure ongoing success and sustainability. Maintaining relevant content in a rapidly evolving healthcare context necessitated regular updates and ongoing investments of time and resources, including curriculum development and access to curricular expertise. While face-to-face interactions were beneficial for relationship-building, they posed logistical and financial challenges—particularly given Canada's broad geographic dispersion and the potential for travel or public health restrictions (as observed during the COVID-19 pandemic). We encountered logistical and technological challenges when coordinating across institutions and provinces, as well as strategies that proved effective. Concrete strategies we used to maintain fellow engagement in virtual spaces included synchronous and asynchronous communication mechanisms (e.g., discussion forums through Slack, breakout rooms for interactive exchange in smaller groups during training sessions). In addition, while the fellows were funded through their HSIF training allowance to attend the NCR, their academic and health system mentors were not funded, and this posed challenges with participation for mentors and HSIF alumni.
Securing sustained funding remained critical for program continuity and evolution. Efforts made to secure long-term support included pursuit of external grants and public-private partnerships (monetary and in-kind). The NCTP submitted two requests for additional resources from CIHR IHSPR for Year 3 and 4 to extend operational support for the program manager to coordinate the training platform, expand the scope of the NCTP to include specialized training for the inaugural cohort of HSIF Early Career Researchers starting in fall 2023, and for scientific publication of the NCTP evaluation and curriculum. In addition, based on continued success of the HSIF and NCTP and recognition of the resource requirements to support the scope of the NCTP, CIHR IHSPR was able to expand funding support for future sustainability of the HSIF program through a competitive CIHR Health Research Training Platform (HRTP) funding program at a higher level of support.34 With NCTP Executive Committee support, the application for the HRTP was successful with principal investigator leadership from one of the HSIF alumna members, who was a co-principal applicant on the NCTP grant proposal and a member of the NCTP Executive Committee.
6 CONCLUSION
The NCTP's experience offered valuable insights for multiple partners in health system transformation. For policymakers, the NCTP illustrated the value of investing in programs that promoted training, professional development, and collaboration among health system–embedded scholars, thereby enhancing the capacity for evidence-informed policy development. Educators could adopt the co-creation and CoP frameworks demonstrated by the NCTP to improve curriculum relevance, learner engagement, and program sustainability. Practitioners could benefit from the program's focus on critical thinking, cross-sectoral perspectives, and networking opportunities. This CIHR-funded NCTP program has paved the way to an expanded opportunity for the sustainability of the health services research community of practice, including support for the CIHR Early Career Researcher (ECR) opportunity with the first incoming cohort of ECRs starting in February 2024. Having fellows embedded in health system organizations has exposed health delivery system leaders to the value of embedded scientists to advance LHS. Subsequent papers to this overview will focus on curriculum and evaluation in depth.
FUNDING INFORMATION
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Institute for Health Services and Policy Research (IHSPR) of the Canadian Institutes for Health Research (CIHR) and supplemental extensions [Funding Reference Numbers: Grant #177252 and Grant #184412]. Additional cash and in-kind support was provided by several organizations: the University of Calgary Cumming School of Medicine, the University of Calgary Vice President of Research Office, and the Alberta Health Services Strategic Clinical Network (all for the period from June 2021 to May 2022); the BC Academic Health Science Network and the Michael Smith Foundation for Health Research (both for the period from June 2022 to May 2023); the Alberta Children's Hospital Research Institute (for 2 years, from June 2021 to May 2023); Alberta Innovates (for the period from June 2021 to May 2022); the Alberta Strategy for Patient Oriented Research SUPPORT Unit (AbSPORU) (for 2 years, from June 2021 to May 2023); and the O'Brien Institute for Public Health (for the period from June 2023 to May 2024).
CONFLICT OF INTEREST STATEMENT
Deborah A. Marshall—Nominated Principal Investigator, Health System Impact Fellowship National Cohort Training Program funded by the Institute for Health Services and Policy Research (IHSPR) of the Canadian Institutes for Health Research (CIHR) and supplemental extension [Funding Reference Numbers: Grant #177252 and Grant #184412] and Svare Chair in Health Economics, Value and Impact. EL holds a Health System Impact Embedded Early Career Researcher Award from the Canadian Institutes of Health Research [Funding Reference Number: 191646].