Improved nasal recovery and intact olfactory function after a transseptal approach for endoscopic endonasal transsphenoidal adenomectomy: A retrospective analysis
Yen-Hui Lee and Huan-Chih Wang are equal contributed.
Funding information: National Taiwan University Hospital, Grant/Award Number: Grant no. 110-S5159
Abstract
Objectives
Endoscopic endonasal transsphenoidal adenomectomy (TSA) is the most frequently performed skull base surgery, and researchers have recently focused on preserving nasal function. The endoscopic transseptal approach is a promising procedure due to its reduced injury to the nasal mucosa; however, there are no studies comparing rhinological and neurosurgical outcomes concurrently with the standard endoscopic transnasal approach. Therefore, we conducted this study to investigate whether the transseptal approach could reduce nasal morbidities with comparable neurosurgical outcomes.
Methods
We retrospectively reviewed 25 patients who underwent endoscopic endonasal transseptal TSA for pituitary adenoma without encasement of internal carotid artery from January 2019 to December 2020. Another 25 patients who received transnasal approach from January 2017 to December 2018 were selected as controls. Patients with diseases affecting the nasal cavity/olfaction or usage of a nasoseptal flap were excluded for a better comparison of the two procedures. We collected data from radiological studies, endocrine studies, endoscopic evaluations, 22-item sinonasal outcome tests (SNOT-22) and Top International Biotech Smell Identification Test (TIBSIT) for comparison.
Results
Lower postoperative SNOT-22 and Lund-Kennedy endoscopic scores were observed in the transseptal group. The effect size of differences were classified as large effect (The absolute value of Cohen's d > 0.8). Nevertheless, the TIBSIT scores were not significantly different. The rates of gross total resection, recovery of hormonal abnormalities, and complications were not significantly different. After controlling possible confounding factors using multivariate analysis, the endoscopic transseptal approach remained an independent factor for lower SNOT-22 scores and Lund-Kennedy endoscopic scores.
Conclusions
The endoscopic transseptal approach provides improved recovery of nasal mucosa and intact olfaction without compromising neurosurgical outcomes.
Level of Evidence
2b.
1 INTRODUCTION
Transsphenoidal adenomectomy (TSA) has evolved enormously and is currently the most frequently performed skull base surgery.1 The endoscopic endonasal approach (EEA) has become a popular surgical method for TSA because of its excellent visualization and minimal comorbidities. Since EEA is a mature and established surgical approach with minimal complications, researchers have recently turned their focus to preserving nasal function and quality of life.
Many otolaryngologists wonder whether rhinological outcomes can be altered by choosing different surgical corridors for TSA, which are classified according to the routes of sphenoidotomy.2 The most common route of sphenoidotomy is transnasal, namely, dissection directly from the bilateral sphenoethmoidal recess in the nasal cavity. Although it seems straightforward, it inevitably damages the anterior wall of the sphenoid sinus, the posterior nasal septum, and their overlying mucosa. In contrast, transseptal sphenoidotomy, that is, dissection through the subperichondrial and subperiosteal planes of the nasal septum, preserves the nasal mucosa and restores the integrity of the sphenoid sinus and posterior nasal septum. The transseptal approach, via either the endonasal or the sublabial route, was once the state-of-the-art surgical method performed in microscopic TSA.3 Recently, several groups have undertaken efforts to develop endoscopic endonasal transseptal TSA and have reported promising rhinological results.4-10 Endoscopic endonasal transseptal TSA should receive more attention during the coronavirus disease 2019 (COVID-19) pandemic because the integrity of the sphenoid sinus prevents unexpected injuries from common nasal procedures, such as nasopharyngeal swab tests or nasogastric tube placement,11, 12 for the rest of the patients' lives.
However, it was questioned that the benefit of endoscopic endonasal transseptal TSA in preserving nasal mucosa may be at the sacrifice of neurosurgical outcomes for its limited surgical exposure and maneuverability. Several studies have reported either soley rhinological or neurosurgical outcomes of endoscopic transseptal approach.4, 7, 8 Previous comparative studies mentioned the comparison of outcomes with microscopic transseptal approach,5, 13 while no studies concurrently compared both rhinological and neurosurgical outcomes of the endoscopic transseptal TSA with those of standard endoscopic transnasal TSA. Therefore, we conducted this study to investigate whether the endoscopic transseptal approach for TSA could prevent nasal morbidities without compromising neurosurgical outcomes.
2 MATERIALS AND METHODS
2.1 Patients
Our surgical teams started performing the transseptal approach in January 2019 for all primary endoscopic skull base surgeries for pituitary tumors without encasement of internal carotid artery (ICA). Thus, we reviewed all patients who received the transseptal approach from January 2019 to December 2020 (transseptal group), and we excluded patients with the following criteria: (1) histopathology other than pituitary adenoma, (2) concurrent diseases affecting nasal cavity or olfaction, and (3) the harvest and use of the nasoseptal flap.
Of 35 consecutive adult patients (≥20 years old) who underwent the transseptal approach, 10 (29%) patients were excluded for the following reasons: 7 (20%) had different pathologies other than pituitary adenoma, 2 (6%) had chronic sinusitis simultaneously, and 1 (3%) had a positive PCR test result for SARS-CoV-2. A total of 25 patients were included for analysis (transseptal group).
Another 25 age- and sex-matched patients who underwent transnasal approach from January 2017 to December 2018 were selected as controls (transnasal group). The inclusion and exclusion criteria were the same as those for the transseptal group. That is, both groups included patients having normal nasal cavities/olfaction and pituitary adenoma without encasement of ICA, and patients using nasoseptal flap were excluded from both groups for better comparison of these two procedures.
This study was approved by the institutional review board of our hospital (IRB: 202011002RINA) and followed the Strengthening the Reporting of Observational Studies in Epidemiology guideline.
2.2 Preoperative assessment
Before surgery, all patients provided a detailed history and underwent radiological studies and endocrinological function tests. The radiological studies encompassed magnetic resonance imaging (MRI) with a pituitary protocol and fine-cut computerized tomography. The size of the tumor was defined as the maximal diameter measured on a coronal view, and regional invasion of the tumor was also recorded. We evaluated endocrinological function with a complete hormone battery of the anterior pituitary lobe, and the functional status could thus be classified as normal, hypersecreting or hypopituitarism.
In addition, we screened all patients for the presence of any nasal symptoms using 22-item sinonasal outcome test (SNOT-22) and performed an endoscopic examination preoperatively to rule out sinonasal disease. To evaluate baseline olfactory function, we used the Top International Biotech Smell Identification Test (TIBSIT, Top International Biotech, Neihu, Taipei, Taiwan), which substitutes odors more familiar to the Taiwanese population for certain odors in the traditional Chinese version of the University of Pennsylvania Smell Identification Test.14
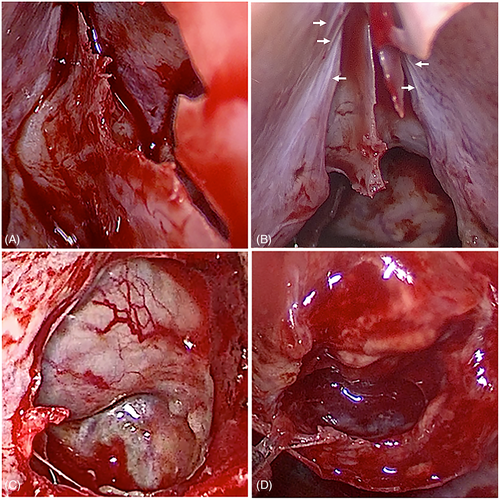
2.3 Surgical techniques: Endoscopic transseptal approach
After lateralization of the bilateral turbinates, the first incision was made anterior to the nasal septal body to avoid bleeding. The mucosal flap was elevated from the subperichondrial and continuing subperiosteal planes, followed by dissection superiorly to the perpendicular plate of the ethmoid bone, posteriorly to the sphenoid rostrum, laterally to the sphenoid sinus ostium, and inferiorly to the nasal floor. Another incision was made on the side posterior to the nasal septal body to avoid perforation, followed by the same dissection. The binostril approach allowed better surgical exposure and a good preservation of septal L-strut. Partial removal of the perpendicular plate was performed, and we applied a Cottle nasal speculum between the septal flaps to establish a surgical corridor (Figure 1A) and to prevent injury to the septal mucosa and olfactory neuroepithelium (Figure 1B). Then, we performed a sphenoidotomy by removing the rostrum (Figure 1C). After creating a sufficient space for four-handed surgery, the neurosurgeons removed the tumor until the arachnoid membrane descended (Figure 1D). Finally, we repositioned the rostrum and septal flaps to prevent adhesion in possible revision surgery in the future. The bilateral turbinates were restored to the neutral position to prevent sinusitis, and the incision wounds were left unsutured to facilitate drainage of the exudate.
2.4 Surgical techniques: Endoscopic transnasal approach
In the transnasal group, bilateral turbinates were also lateralized to expose sphenoethmoidal recess. Then, part of posterior nasal septum and the rostrum, including the overlying mucosa and bony structures, were removed to establish surgical corridor. The following procedures were similar to endoscopic transseptal approach described above, except that the sphenoid sinuses were left wide open and the posterior septectomy window remained at the end of the surgery. That is, the difference between the two approaches is integrity of anterior wall of sphenoid sinus and posterior nasal septum. Procedures affecting nasal outcomes, including resection of middle turbinates and reconstruction using nasoseptal flap, were not performed in either group to ensure comparability.
2.5 Neurosurgical outcomes
We collected rate of total resection and rate of alteration in pituitary hormones as neurosurgical outcomes. Gross total resection was defined as the absence of visible residual tumor on follow-up MRI 6 months after the operation. We defined the postoperative alteration of hormone status at 6 months after surgery as follows: (1) improved denoted that any of the abnormal axes became normal or closer to the normal value; (2) stationary denoted that the abnormal axes remained unchanged; or (3) worsened denoted that the abnormal axes became more deviated from the normal value.
2.6 Rhinological outcomes
We quantified the recovery of nasal mucosa using Lund-Kenney endoscopic at 2 weeks, 1 month, 3 months and 6 months after surgery. To compare subjective nasal symptoms, we collected scores of SNOT-22 at 6 months after the surgery, which was already validated as an effective tool after endoscopic skull base surgery.15 Additionally, we recorded data on TIBSIT at 6 months after the surgery and classified the olfactory status according to the normative values for different age and sex groups.14
2.7 Postoperative pain
The postoperative pain was evaluated periodically using visual analogue scale (VAS), with 0 representing painless and 10 representing the most severe pain. For pain relief, all patients received oral acetaminophen 500 mg every 6 h, and the frequency was decreased if VAS score less than 1. Adjunctive medications, including napoxen 250 mg every 12 h as needed and tramadol 50 mg every 6 h as needed, were administered for VAS score 3–6. Rescue analgesia was provided with intravenous ketorolac every 6 h as needed for severe pain (VAS more 6). VAS score on postoperative day 1, total consumption of oral acetaminophen, and the numbers of patients receiving adjunctive oral analgesics or rescue intravenous ketorolac were collected for comparison.
2.8 Complications
Diabetes insipidus, postoperative CSF leakage, hypopituitarism, intracranial hemorrhage and meningitis were recorded as neurosurgical complications. Epistaxis, septal infection and chronic sinusitis were recorded as nasal complications.
2.9 Statistical analysis
Student's t test and Chi-square test/Fisher's exact test were used for comparisons of the characteristics and outcomes of the two groups. The sequential changes in Lund-Kennedy scores were analyzed with repeated-measures ANOVA, followed by comparisons between groups at the four postoperative timepoints using Student's t test with Bonferroni correction. The difference in scores was summarized in Cohen's d effect size. A Cohen' d effect size of 0.2 was considered a small but important effect, 0.5 represented a medium effect, and an effect size of greater than or equal to 0.8 indicated a large effect. The effect of the transseptal approach on SNOT-22 scores and Lund-Kennedy scores was further analyzed using linear regression and generalized estimating equations to control confounding factors. A p value of less than .05 was considered statistically significant. All analyses were conducted with R, version 4.0.2.
3 RESULTS
3.1 Clinical characteristics
The demographics, radiological features and endocrine functions are summarized in Table 1. The mean ages of the transseptal and transnasal groups were 59.2 ± 14.6 and 56.3 ± 15.8 years, respectively. There were 11 male and 14 female subjects in the transseptal group and 14 male and 11 female subjects in the transnasal group. Age and sex were not different between the two groups.
| Transseptal (N = 25) | Transnasal (N = 25) | p | |
|---|---|---|---|
| Demographic characteristics | |||
| Age (years) | 59.2 ± 14 6 | 56.3 ± 15.8 | .49 |
| Female | 14 (56) | 11 (44) | 1.00 |
| Radiological features | |||
| Size (cm)a | 2.36 ± 0.79 | 2.32 ± 0.86 | .98 |
| Hardy grade | .18 | ||
| I | 0 (0) | 4 (16) | |
| II | 12 (48) | 9 (36) | |
| III | 9 (36) | 10 (40) | |
| IV | 4 (16) | 2 (8) | |
| Parasellar | 23 (92) | 19 (76) | .25 |
| Suprasellar | 21 (84) | 19 (76) | .73 |
| Infrasellar | 4 (16) | 10 (40) | .11 |
| Endocrine function | .42 | ||
| Normal | 16 (64) | 12 (48) | |
| Hypopituitarism | 4 (16) | 4 (16) | |
| Hypersecreting | 5 (20) | 9 (36) | 1.00b |
| Growth hormone/IGF-1 | 2 (8) | 4 (16) | |
| Prolactin | 3 (12) | 1 (4) | |
| ACTH/Cortisone | 0 (0) | 2 (8) | |
| TSH | 0 (0) | 1 (4) | |
| FSH/LH | 0 (0) | 0 (0) | |
| Mixed | 0 (0) | 1 (4) |
- Note: Data are presented as the mean ± SD or number (%); Student's t test was used for continuous variables, and Chi-square/Fisher's exact test was used for categorical variables when appropriate.
- a The maximal diameter of the tumor on coronal view was measured.
- b Distribution of hypersecreting hormones was compared using Fisher's exact test.
The mean tumor size in the transseptal group was 2.36 ± 0.79 cm, while that in the transnasal group was 2.32 ± 0.86 cm. The numbers of lesions classified by Hardy classification from I to IV were 0 (0%), 12 (48%), 9 (36%) and 4 (16%) in the transseptal group and 4 (16%), 9 (36%), 10 (40%) and 2 (8%) in the transnasal group. The number of tumors with regional invasiveness, that is, with parasellar, suprasellar and infrasellar extension, was 23 (92%), 21 (84%), and 4 (16%), respectively, in the transseptal group and 19 (76%), 19 (76%), and 10 (40%), respectively, in the transnasal group. None of the radiological features were significantly different between the two groups.
Preoperative hypopituitarism was noted in only 4 (16%) patients in both groups. Five (20%) patients in the transseptal group and 9 (36%) patients in the transnasal group had hypersecretion of hormones. The preoperative hormonal statuses and the distribution of hypersecreting hormones were not significantly different between the two groups.
3.2 Neurosurgical outcomes
The neurosurgical outcomes are summarized in Table 2. Gross total resection was obtained in 14 (56%) patients in the transseptal group and 15 (60%) patients in the transnasal group. Hormonal status improved in 8 (89%) patients with preoperative hormone abnormalities in the transseptal group and 12 (92%) patients in the transnasal group. There was no significant difference in gross total resection rate or hormone control between these two groups.
| Transseptal (N = 25) | Transnasal (N = 25) | p | |
|---|---|---|---|
| Gross resection rate | 14 (56) | 15 (60) | 1.00 |
| Hormone statusa | 1.00 | ||
| Improved | 8 (89) | 12 (92) | |
| Stationary | 1 (11) | 1 (8) | |
| Worsened | 0 (0) | 0 (0) |
- Note: Data are presented as number (%); Chi-square/Fisher's exact test was used for categorical variables when appropriate.
- a The number of patients with hormone abnormalities was 9 for the transseptal group and 13 for the transnasal group.
3.3 Rhinological outcomes
The postoperative Lund-Kennedy, SNOT-22 and TIBSIT scores are summarized in Figure 2. The postoperative Lund-Kennedy score was significantly lower in the transseptal group than in the transnasal group (p < .001, Figure 2A). Post hoc analysis revealed that the Lund-Kennedy scores were also lower at every timepoint after surgery (mean difference, −2.36, 95% confidence interval (CI), (−3.16, −1.56), Cohen's d, −1.67 at 2 weeks; mean difference, −2.64, 95% CI, (−3.52, −0.88), Cohen's d, −1.50 at 1 month; mean difference, −1.64, 95% CI, (−2.12, −0.48), Cohen's d, −1.13 at 3 months; mean difference, −1.72, 95% CI, (−1.76, −0.04), and Cohen's d, −1.15 at 6 months; all adjusted p < .001, Figure 2A). Also, given the comparable baseline, the SNOT-22 showed lower postoperative scores in the transseptal group than in the transsnasal group at 6 months after surgery (preoperative mean difference, −0.24, 95% CI, (−0.41, 0.73), Cohen's d, −0.16, p = .58; postoperative mean difference, −2.96; 95% CI, (−0.91, −5.01), Cohen's d, −0.83, p = .005, Figure 2B). The effect size of differences in Lund-Kennedy scores and SNOT-22 scores was classified as large effects (The absolute value of Cohen's d > 0.8). Nevertheless, the TIBSIT scores were not significantly different between the two approaches (preoperative mean difference, −0.79, 95% CI, (−3.08, 4.64), Cohen's d, −0.13, p = .68; postoperative mean difference, 1.46; 95% CI, (−5.43, 2.50), Cohen's d, −0.22, p = .46, Figure 2C). Olfactory status based on the normative values of different sexes and ages remained unchanged for all patients.

Table 3 shows the effect of the transseptal approach on the postoperative Lund-Kennedy scores and SNOT-22 scores using regression models. The univariate model revealed significantly lower Lund-Kennedy scores and SNOT-22 scores in the transseptal group (β, −2.09; 95% CI, (−2.54, −1.64), p < .001 and β, −2.96; 95% CI, (−4.98, −0.93), p = .005, respectively). After controlling for age, sex, Hardy grade, presence of regional invasion and endocrine function, the transseptal approach remained an independent factor for lower Lund-Kennedy scores and SNOT-22 scores (β, −2.24; 95% CI, (−2.73, −1.75), p < .001 and β, −2.46; 95% CI, (−4.60, −0.93), p = .02, respectively).
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| β | 95% CI | p | β | 95% CI | p | |
| Lund-Kennedy scorea | −2.09 | (−2.54, −1.64) | <.001e | −2.24 | (−2.73, −1.75) | <.001e |
| SNOT-22b | −2.96 | (−4.98, −0.93) | .005d | −2.46 | (−4.60, −0.93) | .02c |
- Note: Age, sex, Hardy grade, presence of regional invasion and endocrine function were controlled in multivariate analysis.
- Abbreviations: β, coefficients; CI, confidence interval.
- a A generalized estimating equation model incorporating the time factor was used for regression.
- b A linear model was used for regression.
- c p < .05.
- d p < .01.
- e p < .001.
3.4 Postoperative pain
The postoperative VAS pain score and usage of analgesics are summarized in Table 4. The VAS score of the transseptal group was less than that of transnasal group (mean difference, −1.04, 95% CI, (−1.24, −0.07), Cohen's d, −0.66, p = .02). The effect size was classified as medium (The absolute value of Cohen's d > 0.5). Accordingly, the number of patients requiring rescue IV ketorolac for more than two times was also significantly lower in transseptal group (p = .002). On the contrary, no significant difference found in total consumption of oral acetaminophen or in the number of patients requiring additional napoxen or tramadol for pain relief.
| Transseptal (n = 25) | Transnasal (n = 25) | p | |
|---|---|---|---|
| Postoperative pain | |||
| VAS score | 2.1 ± 1.7 | 3.2 ± 1.5 | .02a |
| Cumulative dosage of PO Acetaminophen (mg) | 7320 ± 4235 | 10,120 ± 6524 | .08 |
| Patients using PO Naproxen adjunctively | 4 (16) | 5 (20) | 1.00 |
| Patients using PO Tramadol adjunctively | 2 (8) | 2 (8) | 1.00 |
| Rescue IV ketorolac (≥2 times) | 3 (12) | 14 (56) | 0.002b |
- Note: Data are presented as the mean ± SD or number (%); Student's t test was used for continuous variables, and Chi-square/Fisher's exact test was used for categorical variables when appropriate.
- a p < .05.
- b p < .01.
- Abbreviations: IV, intravenous; PO, per os; VAS, visual analogue scale.
3.5 Complications
The postoperative complications are summarized in Table 5. The rates of neurosurgical complications, including transient diabetes insipidus, hypopituitarism, and postoperative CSF leakage, were not significantly different between the two groups (p = .76, 1.00 and 1.00, respectively). No patients had meningitis, prolonged diabetes insipidus or intracranial hemorrhage.
| Transseptal (n = 25) | Transnasal (n = 25) | p | |
|---|---|---|---|
| Neurosurgical complications | |||
| Transient diabetes insipidus | 7 (28) | 9 (36) | .76 |
| Prolonged diabetes insipidus | 0 (0) | 0 (0) | NA |
| Hypopituitarism | 1 (4) | 1 (4) | 1.00 |
| Postoperative CSF leakage | 1 (4) | 0 (0) | 1.00 |
| Intracranial hemorrhage | 0 (0) | 0 (0) | NA |
| Meningitis | 0 (0) | 0 (0) | NA |
| Nasal complications | |||
| Epistaxis | 1 (4) | 1 (4) | 1.00 |
| Septal infection | 1 (4) | 0 (0) | 1.00 |
| Chronic sinusitis | 0 (0) | 0 (0) | NA |
- Note: Data are presented as numbers (%); Chi-square/Fisher's exact test was used for comparison when appropriate.
One patient (4%) in each group reported self-limiting epistaxis. One (4%) patient in the transseptal group was found to have septal infection and was treated successfully with short-term antibiotics. There was no significant difference in these two complications between the two groups (p = 1.00 and 1.00, respectively). Chronic sinusitis was not noted postoperatively in both groups. None of the patients in the transseptal group had postoperative septal perforation.
4 DISCUSSION
Our study revealed that the endoscopic transseptal approach had less postoperative pain, better patient-reported nasal outcomes and objective endoscopic scores with intact olfactory function than the standard endoscopic transnasal approaches. Meanwhile, the neurosurgical outcomes and rate of complications were comparable. That is, endoscopic transseptal TSA facilitates nasal recovery without compromising neurosurgical outcomes.
In recent years, neurosurgeons and otolaryngologists have made a joint effort to reduce nasal morbidities.16-20 There is increasing evidence indicating that endoscopic transnasal TSA has better neurosurgical outcomes and fewer complications than microscopic transsetpal TSA,21-23 but the sinonasal outcomes have been inconsistent.5, 24, 25 Interestingly, Hong et al. found a better sinonasal quality of life in the early postoperative period in the microscopic transseptal group than in the endoscopic transnasal group.5 They proposed that their finding was due to their avoiding injury to the nasal mucosa in the microscopic transseptal approach. That is, the transseptal approach has great potential with excellent nasal outcomes when manipulating nasal tissue carefully.
Therefore, the endoscopic endonasal transseptal approach can be deemed a favorable technique that combines the advantages of both approaches: comparable neurosurgical outcomes from the endoscopic transnasal approach and minimal nasal morbidities from the microscopic transseptal approach. Favier et al. reported similar gross total resection, endocrine outcomes and rates of neurosurgical complications in the endoscopic transseptal approach, compared to the results of the endoscopic transnasal approach from other experienced teams.7, 8 The impact of the endoscopic transseptal approach on olfactory function was found to be minimal using psychophysiological olfactory tests.9, 26 Furthermore, rhinological outcomes measured with SNOT-22, Sniffin' Sticks and nasal endoscopy were not different at 3 month follow-up between the endoscopic and the microscopic transseptal approach.13
Although previous studies have described neurosurgical or rhinological outcomes of endoscopic transseptal approach, there was no study concurrently comparing both outcomes with the standard endoscopic transnasal approach. To the best of our knowledge, the current study is the first study to compare both neurological and rhinological outcomes of the endoscopic transseptal approach to the standard endoscopic transnasal approach. The result showed lower SNOT-22 scores, lower postoperative Lund-Kennedy scores and intact olfactory function in the transseptal group. Lower VAS pain score for pain and less usage of recue IV analgesics supports the less destructive nature of endoscopic transseptal approach. Meanwhile, the neurosurgical outcome and rates of complications were not inferior. That is, the endoscopic transseptal approach enhances nasal recovery without compromising resection, making it a worthy tradeoff for better rhinological outcomes.
We observed that olfactory function was well preserved in both groups. The possible explanation is that the olfactory neural fibers were not disrupted in either approach.27 In the transseptal approach, incisions are made anteriorly, and the olfactory nerves can be retained within the elevated mucosal flaps. The binostril method also allows for less tension in the mucosal flap, preventing an unbalanced force from disrupting the olfactory neuroepithelium, as in microscopic TSA.28 For the transnasal approach, the main route includes the posterior septum and spares the main olfactory neuroepithelium from permanent dysfunction.29
There may be some concern that managing unexpected high-flow intraoperative CSF leakage could be problematic for endoscopic transseptal TSA. In contrast, a nasoseptal flap can be harvested simply by dividing the septal mucosal flap superiorly and inferiorly with nasal scissors. For patients with a high risk of CSF leakage, an adequate nasoseptal flap, larger than the rescue flap in transnasal approach, could be developed easily by modifying the position of the septal incision. That is, making the septal incision more anteriorly can be considered at the beginning of the surgery. However, whether nasoseptal flap reconstruction via the transseptal route has a similar success rate requires further study.
Even though the endoscopic transseptal approach seems attractive, surgeons should remember that every procedure has its limitations. Dissection of the septal mucosal flap could be difficult in patients with previous nasal surgery, including septoplasty and rhinoplasty. In addition, tumors with more lateral extension may not be removed thoroughly. Finally, although septal infection was present in only one patient in our series, severe septal infection may result in perforation or nasal deformity. We should carefully examine patients with unusual postoperative nasal pain.
There were several limitations in this study. First, the study was retrospective in nature and with smaller size. The result still requires validation with randomized-controlled studies. Second, we included only pituitary adenoma, and whether the conclusions can be generalized to other sellar pathologies remains unexplored. Finally, we only analyzed data until 1 year after surgery. Long-term complications, especially septal complications, require a longer follow-up.
5 CONCLUSIONS
The transseptal approach is an effective procedure for pituitary adenoma with better nasal recovery than other approaches. It might be considered as an alternative surgical technique for pituitary adenoma under selected circumstances.
FUNDING INFORMATION
The study was funded by Grants no. 110-S5159 from National Taiwan University Hospital.
CONFLICT OF INTEREST
The authors declare there is no potential conflict of interest.




