Ossicular joint histopathology in cases of age-related hearing loss
Abstract
Objectives
Age-related hearing loss (presbycusis) is a prevalent condition traditionally attributed to inner ear dysfunction. Little is known about age-related changes in the ossicular joints or their contribution to presbycusis. Herein, we performed an otopathologic evaluation of the ossicular joints in cases of presbycusis without a clear sensorineural explanation.
Methods
Histopathologic analysis of the incudomallear (IM) and incudostapedial (IS) joints was performed in specimens from the National Temporal Bone Registry with audiometrically confirmed presbycusis but without histologically observed sensorineural, strial, or mixed features; deemed cases of “indeterminate” presbycusis. Specimens identified as “indeterminate” presbycusis (IP, n = 18) were compared to specimens with histologically confirmed sensorineural presbycusis (n = 16) and strial presbycusis (n = 11). Presbycutic specimens were also compared to age-matched controls (n = 9) and young controls (n = 14).
Results
The synovial space at the center of the IM joint was wider in the IP group (194 ± 36.8 μm) compared to age-matched controls (138 ± 36.5 μm), young controls (149 ± 32.2 μm), and ears with sensorineural presbycusis (148 ± 52.7 μm) (p < .05). The synovial space within the IS joint was wider in the IP group (105 ± 33.0 μm) when compared to age-matched controls (57.9 ± 13.1 μm) and ears with sensorineural presbycusis (62.3 ± 31.2 μm) (p < .05).
Conclusion
IP ears have wider IM and IS joints when compared to ears with sensorineural presbycusis and age-matched controls. Findings point to a potential middle ear source of high frequency conductive hearing loss in a subset of presbycutic ears.
Level of Evidence
Retrospective study.
1 INTRODUCTION
Presbycusis or age-related hearing loss is a prevalent condition that is estimated to impact more than half of all people over 70 years of age in the United States.1 Clinical hallmarks of the disease include reduced hearing sensitivity, decreased ability to discern speech in noise, and challenges with sound localization.2 Such persistent sensory deficits have psychosocial implications and have been shown to contribute to an increased risk of loneliness and depression among elderly adults.3, 4 In addition, recent evidence suggests a link between hearing loss and both age-related cognitive decline and dementia.5, 6 From an economic perspective, presbycusis is estimated to contribute to at least $3.3 billion in excess medical costs in the United States7 and around $980 billion in total costs internationally.8
Despite its prevalence and societal impact, the precise pathophysiology involved in presbycusis remains unclear. In order to understand the histopathologic correlates of audiometrically defined presbycusis, Harold Schuknecht established five “classic” categories of presbycusis: sensory, neural, strial, mixed, and indeterminate.9-12 Although most cases of presbycusis are multifactorial and consist of overlapping phenotypes,13 Schuknecht's classification system has served as a framework for human temporal bone and animal studies that have further explored the mechanisms by which the degeneration of inner and outer hair cells, spiral ganglion neurons, and the stria vascularis contribute to presbycusis.12, 14, 15 Recent advances in differential interference contrast (DIC) microscopy have allowed for higher resolution assessment of hair cell loss16 and suggest that many cases of presbycusis may be explained primarily as a loss of hair cells rather than strial atrophy.16, 17 However, even updated models using histopathologic correlates of audiometric hearing loss severity cannot account for the full extent of threshold elevation with inner ear findings alone. Indeed, as many as 25% of cases in Schuknecht's “classical” analyses lacked a clear inner ear etiology and were deemed indeterminate presbycusis (IP).18
Human otopathology and middle ear functional work support the idea that age-related changes in the conductive pathway contribute to presbycusis. Specifically, recent work has revealed age-related degenerative changes along the ossicular chain localizing to the incudomallear (IM) and incudostapedial (IS) joints19 as well as the distal incus.20, 21 Results from middle ear function testing with both wideband acoustic immittance and laser Doppler vibrometry has demonstrated an increase in middle ear compliance with age.22 Functional studies from patients with increased middle ear compliance commonly demonstrate loose ossicular connections (e.g., partial ossicular discontinuity). Audiometrically, loose ossicular connections manifest as an isolated high frequency conductive hearing loss.23, 24
Taken together, these findings lead us to hypothesize that age-related changes at the IMJ and ISJ may have implications on ossicular compliance and high frequency conductive hearing. Specifically, we hypothesize that in a subset of presbycutic temporal bones without clear evidence of inner ear pathology, middle ear otopathologic assessment may reveal widening of the IM and/or IS joint when compared to other types of presbycusis. Herein, we apply a combination of two previously described methods to study both the IMJ and ISJ in human temporal bones with a prior designation of “indeterminate” presbycusis. We compare measures to ears with histopathologic evidence of other presbycusis types as well as normal hearing controls.
2 MATERIALS AND METHODS
All temporal bone (TB) specimens included in this study are a part of the National Temporal Bone Bank and were available for review at the Massachusetts Eye and Ear Infirmary. The study received approval by the institutional review board (2019P003755) and all patients provided informed consent as part of their enrollment into the National Temporal Bone Registry.
Methods used for preparation and analysis of temporal bone specimens have been previously described.12 In brief, all TB specimens were decalcified in ethylene diamine tetra-acetic acid, and then dehydrated and embedded in celloidin for sectioning. TB sections were cut in a horizontal plane at a thickness of 20 μm, stained with hematoxylin and eosin (H&E), and mounted on glass slides. The original sections were examined microscopically by otopathologists, and all histologic features were recorded using classical techniques.
2.1 Cases and controls
All cases of presbycusis with a history of ear surgery, head trauma, middle ear neoplasm, hereditary otologic syndromes, exposure to excessive noise or ototoxic medications, or audiometric evidence of low frequency conductive hearing loss >10 dB was excluded prior to selecting cases within each subtype of presbycusis (Figure 1).
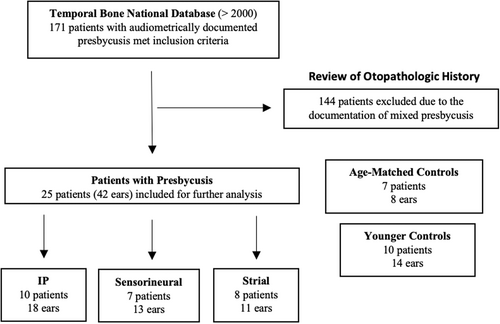
Cases of IP were those with (1) audiometrically documented presbycusis (defined as down-sloping [≥2 kHz] moderate to severe or profound hearing loss) without a clinical history to suggest another known hearing loss etiology and (2) no clear histopathological evidence of a sensory, neural, strial, or mixed etiology. Sensorineural presbycusis cases were those with (1) audiometrically documented presbycusis (same definition as above) and (2) clear histopathological evidence of either a sensory, neural, or mixed etiology. Strial presbycusis were those with (1) audiometrically documented presbycusis (defined as down-sloping or flat curve moderate or severe hearing loss [≥2 kHz]) and (2) clear histopathological evidence of a strial etiology.
Inclusion criteria for control cases was audiometrically documented air conduction ≤30 dB at 2, 4, 6, and 8 kHz. Control cases were excluded if there was a history of ear surgery, head trauma, middle ear neoplasm, hereditary otologic syndromes, or exposure to excessive noise or ototoxic medications. To permit further comparison of age-only related changes, controls were divided into age-matched controls (age >45 years) and young controls (age <45 years).
2.2 Image acquisition and analysis
All TB slides from each subject were evaluated following high-resolution digitization using a 400-slide capacity brightfield scanner (Aperio AT2; Leica Biosystems, Wetzlar, Germany). Images were obtained with a resolution of 246,016 pixels/mm2 at 5× magnification and measurements were made in ImageJ (http://rsbweb.nih.gov/ij/). Following acquisition, all TB images were de-identified and labeled with a unique, random study ID to ensure reviewers were blinded when completing measurements for each case.
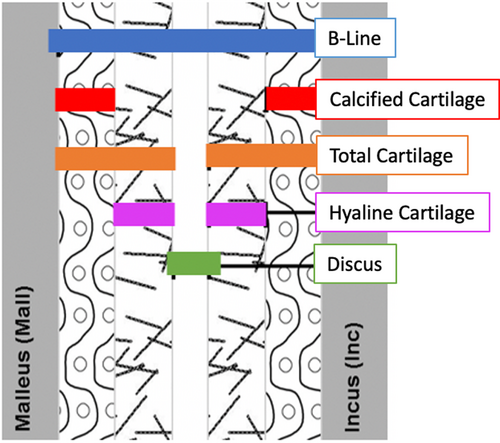
For the IMJ analysis, we adapted the method developed by Fausch and Röösli to capture 27 parameters (Figure 2) on a single horizontally cut TB section.25 Of the 10–12 sections that captured the IMJ, the single section with the longest distance between the synovial membranes resting on the lateral ligaments of the joint capsule (Longline) was selected. Given the horizontally sectioned slide orientation, the “Longline” runs in the anterior to posterior direction. Along the longline, the IMJ is subsequently quartered to visualize three equidistant positions (two peripheral and one central) at which nine parameter measurements that are roughly perpendicular to the longline, in the medial-lateral direction, are made. The nine parameter measurements include: the distance between the osseus surfaces (B-line), the cartilage levels (hyaline, calcified, and total cartilage) on the malleus and incus surfaces of each ossicle, the combined total cartilage on both ossicles (total cartilage M + I), and the width of the articular disk between the incus and the malleus (Discus). The nine parameter measurements are repeated at each of the three positions to provide 27 measurements per specimen.
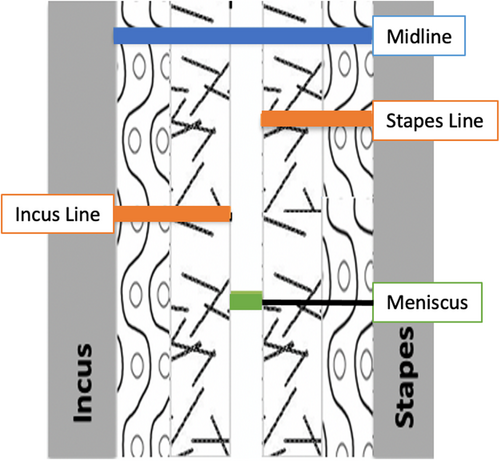
For the ISJ analysis, we adapted the method developed by Ogando et al. to capture seven parameters (Figure 3) on a single horizontal TB section.26 Of the 42 ears with presbycusis, only 26 contained sections that included the ISJ (11 IP, 10 sensorineural, and 5 strial) and of the 22 control ears, 12 contained sections through the ISJ (4 age-matched and 8 younger). Of the one to three sections that captured the ISJ, the section with the longest distance between the synovial membranes resting on the ligaments of the joint capsule (Longline) was selected. Like the IMJ, the ISJ along the longline was quartered to visualize three equidistant positions at which measurements were completed. The seven parameter measurements include: the distance between osseus surfaces of the incus and stapes at each position (antline, midline, and postline), the width of the calcified cartilage from bone to the edge of the articular disk along both the incus (Incus line) and stapes (Stapes line) at the Midline, the combined calcified cartilage on both ossicles at the Midline (total cartilage I + S) and the width of the articular disk between the incus and stapes at the Midline (Meniscus line). Please refer to Table 1 for a complete list of measurement descriptors for reference.
| Indicator | Measurement description |
|---|---|
| IMJ analysis | |
| Longline | Anterior–posterior distance limited by the synovial membrane |
| Central line | Malleal to incudal distance at ½ length of the longline |
| Peripheral lines | Malleal to incudal distance at both ¼ and ¾ length of the longline |
| B-line | Malleal to incudal distance |
| Total cartilage M/I | Total cartilage along both the malleus and the incus |
| Calcified cartilage M/I | Calcified cartilage attached to either malleus or incus (from bone to the hyalinized cartilage) |
| Hyaline cartilage M/I | Hyaline cartilage attached to either malleus or incus (from bone to the edge of the articular disk) |
| Discus | Articular disk present between malleus and incus at longline midpoint |
| Total cartilage M + I | Sum of the total cartilage M and total cartilage I, reflective of total cartilage present at the midpoint |
| ISJ analysis | |
| Longline | Anterior–posterior distance limited by the synovial membrane |
| Antline | Incudal to stapedial distance at anterior ¼ of the longline |
| Midline | Incudal to stapedial distance at the midpoint of the longline |
| Postine | Incudal to stapedial distance at posterior ¼ of the longline |
| Stapes line | Calcified cartilage attached to stapes (from bone to the edge of the articular disk) at the midpoint |
| Incus line | Calcified cartilage attached to incus (from bone to the edge of the articular disk) at the midpoint |
| Meniscus line | Articular disk present between incus and stapes at longline midpoint |
| Total cartilage | Sum of the stapes line and incus line, reflective of total calcified cartilage present at the midpoint |
To validate the methodology for both IMJ and ISJ evaluation, two blinded co-authors (P.R. and M.C.B.) individually analyzed all the appropriate parameters for 20 temporal bones, and the variations in measured lengths were assessed via Bland–Altman analysis.
2.3 Statistical analysis
Continuous variables are described by mean and standard deviation. Categorical variables are reported as absolute and relative frequencies. Welch's analysis of variance (ANOVA) and Dunnett's T3 multiple comparisons test were performed with the IP ears as the referent cases. Statistical significance for all tests was set at p < .05. All statistical tests were performed using GraphPad Prism version 9.0.0 for Mac OS X, GraphPad Software, San Diego, California USA, www.graphpad.com.
3 RESULTS
A total of 25 patients (42 ears) with audiometrically and histologically defined classic presbycusis subtypes, met inclusion criteria. Ten patients (18 ears) had “indeterminate” presbycusis, seven patients (13 ears) had sensorineural presbycusis, and eight patients (11 ears) had strial presbycusis. Seven normal hearing age-matched controls (8 ears) and 10 young controls (14 ears) also met inclusion criteria. The demographics for the ears in all five groups are shown in Table 2.
| General characteristics | Indeterminate | Sensorineural | Strial | Age-matched controls | Young controls |
|---|---|---|---|---|---|
| Patients | 10 | 7 | 8 | 7 | 10 |
| Ears | 18 | 13 | 11 | 8 | 14 |
| Age of ears (mean ± SD) | 75 ± 11 | 76 ± 6.5 | 76 ± 7.8 | 63 ± 8.8 | 32 ± 11 |
3.1 IMJ analysis
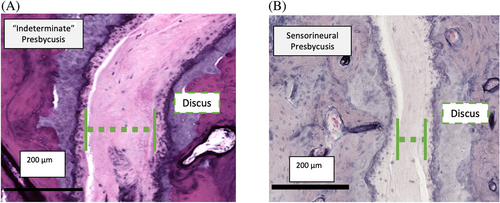
Nine central and 18 peripheral IMJ measurements were made in each specimen. Of note, the two sets of peripheral IMJ measurements are averaged together and reported as a single set of results. Results were tabulated and compared between presbycutic and normal hearing controls (Table 3) and compared between presbycutic subtypes (Table 4). When sorted and compared between presbycutic subtype, the IMJ was found to be wider at its center in IP cases when compared to the sensorineural ears as well as when compared to both age-matched and young controls. Specifically, the distance between the cartilaginous surfaces (discus) of each ossicle was found to be 40% wider in the IP patients (194 ± 36.8 μm) when compared to the sensorineural ears (139 ± 43.0 μm), 33% wider when compared to the age-matched controls (146 ± 28.4 μm), and 30% wider when compared to the young controls (149 ± 32.2 μm) (p < .05). Example IMJ sections with the discus illustrated are shown for “indeterminate” presbycutic patients (Figure 4A) and sensorineural presbycusis ears (Figure 4B).
| Indicators | All presbycusis | Age-matched controls | Young controls |
|---|---|---|---|
| IMJ central position analysis (mean ± SD) | |||
| B-line | 287 ± 78.1 | 252 ± 43.8 | 278 ± 71.9 |
| Total car M | 63.3 ± 41.6 | 49.9 ± 15.6 | 61.8 ± 41.8 |
| Calc car M | 36.4 ± 31.0 | 27.5 ± 9.93 | 43.2 ± 35.3 |
| Hyaline car M | 26.8 ± 17.0 | 22.4 ± 10.2 | 18.7 ± 10.3 |
| Total car I | 58.8 ± 23.5 | 56.4 ± 28.3 | 66.7 ± 41.6 |
| Calc car I | 37.3 ± 20.1 | 39.9 ± 21.6 | 47.7 ± 41.8 |
| Hyaline car I | 21.5 ± 13.6 | 16.6 ± 11.4 | 19.0 ± 9.09 |
| Discus | 165 ± 47.6 | 146 ± 28.4 | 149 ± 32.2 |
| Total cartilage M + I | 122 ± 48.8 | 106 ± 33.3 | 129 ± 70.2 |
| IMJ peripheral position analysis (mean ± SD) | |||
| B-line | 216 ± 72.9 | 199 ± 70.9 | 176 ± 55.8 |
| Total car M | 52.9 ± 28.5 | 53.9 ± 27.4 | 49.5 ± 25.8 |
| Calc car M | 31.4 ± 23.2 | 34.4 ± 24.1 | 33.0 ± 21.1 |
| Hyaline car M | 21.5 ± 12.5 | 19.5 ± 9.47 | 16.5 ± 8.60 |
| Total car I | 52.4 ± 25.9 | 57.9 ± 38.1 | 39.9 ± 20.7 |
| Calc car I | 32.1 ± 22.2 | 35.7 ± 33.6 | 25.8 ± 17.7 |
| Hyaline car I | 20.3 ± 11.9 | 22.3 ± 12.4 | 14.0 ± 6.31 |
| Discus | 111 ± 49.2 | 86.9 ± 39.1 | 86.5 ± 39.4 |
| Total cartilage M + I | 105 ± 44.4 | 112 ± 53.2 | 89.3 ± 36.9 |
| ISJ analysis (mean ± SD) | |||
| Antline | 242 ± 76.8 | 247 ± 89.3 | 272 ± 53.0 |
| Midline | 231 ± 66.4 | 209 ± 20.5 | 241 ± 50.9 |
| Postine | 293 ± 96.1 | 292 ± 79.0 | 282 ± 62.5 |
| Stapes line | 72.0 ± 30.8 | 57.0 ± 28.3 | 65.7 ± 20.2 |
| Incus line | 78.7 ± 40.9 | 89.2 ± 27.7 | 77.5 ± 33.9 |
| Meniscus line | 80.4 ± 37.6 | 63.0 ± 7.69 | 97.5 ± 32.7 |
| Total cartilage | 151 ± 59.2 | 146 ± 15.2 | 143 ± 43.0 |
- Note: All measurements are reported in micrometers.
- There were no significant differences between groups observed in this comparison.
| Indicators | Indeterminate | Sensorineural | Strial | Age-matched controls | Young controls |
|---|---|---|---|---|---|
| Central position (mean ± SD) | |||||
| B-line | 324 ± 88.6a | 250 ± 63.0a | 269 ± 48.2 | 253 ± 43.8a | 280 ± 71.9 |
| Total car M | 67.8 ± 60.0 | 60.4 ± 19.5 | 59.2 ± 21.2 | 49.9 ± 15.6 | 61.8 ± 41.8 |
| Calc car M | 41.5 ± 44.2 | 32.4 ± 15.7 | 32.9 ± 15.8 | 27.5 ± 9.93 | 43.2 ± 35.3 |
| Hyaline car M | 26.3 ± 22.2 | 28.0 ± 6.65 | 26.2 ± 17.3 | 22.4 ± 10.2 | 18.7 ± 10.3 |
| Total car I | 63.5 ± 25.8 | 50.5 ± 24.0 | 61.0 ± 17.7 | 56.4 ± 28.3 | 66.7 ± 41.6 |
| Calc car I | 39.3 ± 21.8 | 31.2 ± 19.5 | 41.4 ± 18.1 | 39.9 ± 21.6 | 47.7 ± 41.8 |
| Hyaline car I | 24.3 ± 13.8 | 19.3 ± 16.5 | 19.6 ± 9.28 | 16.6 ± 11.4 | 19.0 ± 9.09 |
| Discus | 194 ± 36.8a | 139 ± 43.0a | 149 ± 45.9 | 146 ± 28.4a | 149 ± 32.2a |
| Total cartilage M + I | 131 ± 66.6 | 111 ± 32.2 | 120 ± 26.6 | 106 ± 33.3 | 129 ± 70.2 |
| Peripheral position (mean ± SD) | |||||
| B–line | 215 ± 82.1 | 216 ± 63.7 | 217 ± 70.0 | 199 ± 70.9 | 176 ± 55.8 |
| Total car M | 46.3 ± 29.9 | 60.4 ± 29.3 | 55.0 ± 22.9 | 53.9 ± 27.4 | 49.5 ± 25.8 |
| Calc car M | 27.4 ± 23.9 | 37.1 ± 25.5 | 31.3 ± 18.0 | 34.4 ± 24.1 | 33.0 ± 21.1 |
| Hyaline car M | 19.0 ± 13.3 | 23.3 ± 11.1 | 23.7 ± 12.3 | 19.5 ± 9.47 | 16.5 ± 8.60 |
| Total car I | 50.5 ± 27.2 | 49.7 ± 25.7 | 59.3 ± 23.7 | 57.9 ± 38.1 | 39.9 ± 20.7 |
| Calc car I | 29.9 ± 22.9 | 31.2 ± 22.3 | 37.2 ± 21.1 | 35.7 ± 33.6 | 25.8 ± 17.7 |
| Hyaline car I | 20.6 ± 13.4 | 18.5 ± 7.36 | 22.1 ± 13.8 | 22.3 ± 12.4 | 14.0 ± 6.31 |
| Discus | 118 ± 53.2a | 106 ± 36.8 | 103 ± 56.0 | 86.9 ± 39.1 | 86.5 ± 39.4a |
| Total cartilage M + I | 96.9 ± 45.7 | 110 ± 47.3 | 114 ± 36.7 | 112 ± 53.2 | 89.4 ± 36.9 |
- Note: All measurements are reported in micrometers.
- a Indicates that the value is significantly different from the indeterminate presbycusis ears per ANOVA testing.
The distance between the osseous surfaces (B-line) of each ossicle was also found to be 30% wider in the IP patients (324 ± 88.6 μm) when compared to the sensorineural ears (250 ± 63.0 μm) and was wider when compared to age-matched controls (253 ± 43.8 μm) (p < .05). There were no differences in the cartilage thickness on either ossicular surface along the length of the IMJ when evaluated at the center of the joint. Taken together, the widened center of the IMJ in IP cases appears to be driven by an increased distance between the ossicles, manifest in the joint capsule (discus) without differences in cartilage thickness on either ossicle.
At the periphery, the discus of the IMJ was found to be 36% wider in the IP cases (118 ± 53.2 μm) when compared to the young controls (86.5 ± 39.4 μm) (p = .033). There were no differences in any of the other parameters evaluated at the periphery of the joint, including the B-line or the cartilage levels. When all presbycutic ears were combined, there were no significant differences in IMJ measurements when compared to both age-matched and young controls.
3.2 ISJ analysis
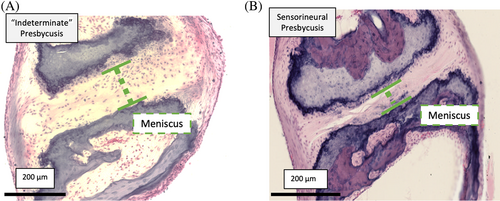
Seven width measurements of the ISJ were performed, analyzed, and compared (Table 2). When sorted and compared between presbycutic subtype, the ISJ was found to be wider in the IP cases when compared to the sensorineural ears as well as the age-matched controls (Table 5). Specifically, the articular cartilage between the incus and the stapes was found to be 60% wider in the IP patients (105 ± 33.0 μm) when compared to the sensorineural ears (65.5 ± 31.0 μm) and 40% wider when compared to the age-matched controls (63.0 ± 7.69 μm) (p < .05). There were no differences in any of the other parameters, including the total distance between the osseous surfaces (Midline) or the cartilage levels along the length of the ISJ. Example ISJ sections are shown for “indeterminate” presbycutic patient (Figure 5A) and a sensorineural presbycutic patient (Figure 5B). There were no significant differences in ISJ measurements between all combined presbycutic ears and the age-matched or young controls.
| Indicators | Indeterminate | Sensorineural | Strial | Age-matched controls | Young controls |
|---|---|---|---|---|---|
| Antline | 266 ± 81.9 | 209 ± 66.7 | 254 ± 74.7 | 247 ± 89.3 | 272 ± 53.0 |
| Midline | 247 ± 49.4 | 211 ± 75.3 | 237 ± 83.2 | 209 ± 20.5 | 241 ± 50.9 |
| Postine | 323 ± 82.8 | 259 ± 79.9 | 296 ± 144 | 292 ± 79.0 | 282 ± 62.5 |
| Stapes line | 70.2 ± 24.1 | 71.6 ± 35.3 | 77.0 ± 40.4 | 57.0 ± 28.3 | 65.7 ± 20.2 |
| Incus line | 71.8 ± 23.8 | 73.6 ± 40.3 | 104 ± 66.2 | 89.2 ± 27.7 | 77.5 ± 33.9 |
| Meniscus line | 105 ± 33.0a | 65.5 ± 31.0a | 55.9 ± 31.5 | 63.0 ± 7.69a | 97.5 ± 32.7 |
| Total cartilage | 142 ± 43.1 | 145 ± 68.5 | 181 ± 72.7 | 146 ± 15.2 | 143 ± 43.0 |
- Note: All measurements are reported in micrometers.
- a Indicates that the value is significantly different from the indeterminate presbycusis ears per ANOVA testing.
3.3 Methodologic consistency
Nine hundred and ninety-nine measurements (37 cases) at the IMJ were compared between two blinded reviewers. Via Bland–Altman analysis, the mean ± SD of the difference between the researchers was 0.597 ± 6.47 μm or 0.513 ± 5.56% when expressed as a function of the mean discus length for all measured groups.
4 DISCUSSION
This study demonstrates that both the IMJ and ISJ are wider in a population of presbycutic ears without histopathologic evidence of sensory, neural, strial, or mixed features when compared to ears with sensorineural presbycusis and normal hearing age-matched and young controls. At the center of the IMJ specifically, the space between the articular cartilage was wider in the IP cases compared to sensorineural cases, age-matched controls, and young-controls. Interestingly, the distance between the bony surfaces of the malleus and incus was wider in the IP cases when compared to the sensorineural cases and age-matched controls, but not the young controls, suggesting a widening of the entire bony joint, as opposed to a loss of cartilage. At the ISJ, the articular cartilage was wider in the IP cases compared to both sensorineural cases and age-matched controls. These quantitative findings are consistent with our original hypothesis, that in a subset of presbycutic patients without a classically described inner ear etiology for presbycusis, middle ear otopathologic assessment may reveal widening of both the IMJ and ISJ when compared to other types of presbycusis as well as young controls.
This work represents the first study to quantitatively assess ossicular joint width in distinct subtypes of presbycusis patients. Prior histologic studies of the incudomallear and incudostapedial joints have qualitatively demonstrated that degenerative changes occur within the joint spaces with age. In a study of 125 temporal bone sections, Etholm and Belal concluded that narrowing and obliteration of the ossicular synovium as well as increased calcification of the articular cartilage occurs with age at both the IMJ and the ISJ.19 Additional studies including a review of 152 temporal bone specimens by Gussen and a review of 40 temporal bone specimens by Savic and Djeric provided further evidence of IMJ surface defects including atrophy, fibrosis and calcification that occurred with age.27, 28
Although prior studies provided qualitative evidence of degenerative changes of the ossicular joints, using our systematic quantitative approach, we demonstrate that there were no significant differences in either the synovial width or the width of the hyalinized, calcified, or total cartilage between young ears when compared to age-matched controls. In fact, we report a widening of the ossicular synovium along the center of the IMJ and ISJ in cases of IP when compared to both sensorineural presbycusis and control ears.
The increased synovial width in the IMJ as well as the ISJ among IP ears most likely reflects an increase in the distance between the two ossicles rather than a decrease in the ossicular cartilage along either bony surface. This is demonstrated by the larger relative difference in the B-line than the total cartilage levels between presbycutic subtypes and controls. Importantly, we find that the increased joint width was isolated primarily to IP ears and appears to be distinct from other previously described age-related changes in the ossicular chain including bone resorption of the incus long process and decreases in incus osteocytes.20, 21
We also find that ossicular joints do not appear quantitatively different between IP ears and ears with classically defined strial presbycusis. Advances in DIC microscopy have allowed researchers to recognize that the subtle loss of hair cells may be an important driver of characteristically flat threshold loss on audiometry in cases of strial presbycusis.17 The similarities in IMJ and ISJ width in both our strial presbycusis and IP cases may also suggest an additional potential middle ear etiology for a portion of the observed hearing loss seen in both presbycutic subtypes.
Of note, in a recent study of 153 IMJ specimens, Dobrev et al. demonstrated an age-related increase in the IMJ space with a methodologically similar approach to the one adopted in the current study.29 This age-related increase in IMJ width is in keeping with key findings from this study as well as with previous work from our group.30 However, a key difference between our present work and the analysis performed by Dobrev et al. is the lack of comparison of classic histopathologic subtypes of presbycusis. To offer an audiologic correlate for their histopathologic findings, the authors compared audiograms of 1760 ears (974 subjects) from a separate database independent of their temporal bone specimens. They identified a small but statistically significant increase in the ABG at 4 kHz between younger and older ears. The association of aging and the development of a 4 kHz ABG has been explored in other audiometric studies,31 and findings have been heterogeneous.32 We hypothesize that a conductive form of presbycusis occurs in some but not all patients, and our findings are supported by a large literature pointing to multiple factors associated with age related hearing loss.2 Our finding that a subset of presbycutic ears demonstrated a greater degree of IMJ widening than histologically confirmed sensorineural or strial presbycutic ears may provide insight into the etiology of this 4 kHz ABG increase.
Although we are unable to make a claim about the functional impact of the widened ossicular joints in the IP ears, like Dobrev et al., we hypothesize that the observed differences may impart an alteration in ossicular compliance and impact middle ear transfer function. Prior work in cadaveric temporal bones has demonstrated that changes in the compliance of the ossicular joints impacts the amount of mechanical energy lost in the transmission of sound from the tympanic membrane (TM) to the oval window. Specifically, increases in middle ear compliance lead to increased absorption of mechanical energy by the joints and a decrease in the transfer of high-frequency sound. Clinically, partial ossicular discontinuity including distal incus necrosis or fracture has demonstrated an increase in middle ear compliance with an accompanying high-frequency conductive hearing loss.23, 24, 33 Although none of the IP cases that were evaluated had evidence of discontinuity, we hypothesize that the widening of the IMJ reflects a similar, though less dramatic, decoupling of the ossicular chain. For this reason, we speculate that the differences we observe on otopathological review may contribute to the high-frequency, down-sloping loss observed on the audiogram in IP cases. Clinically, given the lack of measured bone conduction thresholds over 4 kHz, a conductive component of hearing loss in the high frequencies may not be readily apparent.
Although our findings lend support to the hypothesis that changes along the conductive pathway contribute to high-frequency hearing loss, we recognize that there are important limitations in our work. Methodological limitations in measuring the IMJ include the subjectivity involved in determining the location of the borders between the calcified cartilage and bone as well as between the hyaline cartilage and the articular disk. Despite this area of potential discrepancy, there was reasonable methodological consistency, as evidenced by our Bland–Altman results.
Another limitation is in the number of specimens that we were able to analyze due to our relatively strict inclusion and exclusion criteria. Based on our criteria, we had 10 or less patients and between 18 and 11 ears within the indeterminate, sensorineural, and strial groups. It is also important to note that even within the discrete subtypes of presbycusis that were analyzed there was variability that was not captured (duration of hearing loss, degree of hair cell or spiral ganglion neuron loss or amount of strial atrophy, etc.). Therefore, our small sample size of ears and variability within each of the subtypes represent limitations in our study.
Although the specificity of our criteria allowed us to evaluate discrete subtypes of presbycusis, the lack of mixed presbycusis cases, which represent most cases in the National Temporal Bone Registry limits our ability to develop a robust regression analysis to understand the changes in the IMJ and ISJ as a function of age in presbycusis. The addition of mixed presbycusis and the extraction of the specific inner ear features (outer and inner hair cell counts with updated DIC techniques,16 spiral ganglion neuron counts, and stria vascularis area) will allow us to develop a multivariate model which would be better suited to assess the associations between age, gender, distinct otopathologic features and IMJ/ISJ width.
Future otopathologic study of the other elements in the conductive pathway including the ossicular ligaments and the TM in ears with “indeterminate presbycusis” is necessary.34-36 As the TM specifically has been demonstrated to undergo morphogenic changes with age37 and cadaveric temporal bone work reveals that the radial collagen fiber distribution play an important role in high-frequency hearing,38 careful histopathologic characterization of the TM in IP cases would also be helpful.
Finally, advances in non-invasive middle ear imaging techniques such as cone-beam CT39 and optical coherence tomography40 offer the potential to study structural and functional changes in the middle ear that occur with age in live subjects. We hope to better correlate these findings with high frequency audiometric thresholds in the future.
5 CONCLUSION
Both the IMJ and the ISJ were wider in cases of “indeterminate” presbycusis than in both sensorineural presbycusis and controls. These findings point to a potential source of high frequency conductive hearing loss in a subset of presbycutic ears. Further histopathologic and biomechanics research is necessary to understand the prevalence and functional effects of these observed differences.
ACKNOWLEDGMENTS
The authors would like to thank MengYu Zhu for her help with obtaining temporal bone specimens for analysis. This study was supported by NIH NIDCD (K08DC018575).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.