Surgical Outcomes by Early Airway Endoscopy Findings after Pediatric Staged Laryngotracheoplasty
Editor's Note: This Manuscript was accepted for publication on June 27, 2023.
This study was presented at the Triological Society Annual Meeting at COSM 2023, May 4, 2023, in Boston, Massachusetts.
The authors have no funding, financial relationships.
Abstract
Objectives
To determine how initial postoperative airway endoscopy findings after stent removal predict successful decannulation in children undergoing double-staged laryngotracheoplasty (dsLTP). Secondary objectives assessed timing of decannulation and number of endoscopic interventions needed after dsLTP.
Methods
A case series with chart review included children who underwent dsLTP at a tertiary children's hospital between 2008 and 2021. Rates of decannulation, time to decannulation, and number of interventions after dsLTP were recorded for children with high- or low-grade stenosis at the first bronchoscopy after stent removal.
Results
Of the 65 children who were included, 88% had high-grade stenosis and 98% had a preoperative tracheostomy. Successful decannulation happened in 74% of the children, and 44% of the children were decannulated within 12 months of surgery. For children with low-grade stenosis at the first endoscopy after stent removal, 84% were successfully decannulated compared with 36% of the children with high-grade stenosis (p = 0.001). After dsLTP, children with high-grade stenosis required 7.5 interventions (SD: 3.3) compared with 4.0 interventions (SD: 3.0) for children with low-grade stenosis (p < 0.001). Decannulated children with high-grade stenosis necessitated more endoscopic procedures (7.0 vs. 3.7, p = 0.02). Time to decannulation was similar between children with high- and low-grade early postoperative stenosis (21.9 vs. 17.8 months, p = 0.63).
Conclusions
Higher grade stenosis identified on the first airway endoscopy after suprastomal stent removal is correlated with lower decannulation rates and more postoperative endoscopic interventions. Although time to decannulation was not impacted by early stenosis grade, surgeons might utilize these early airway findings to counsel families and prognosticate possible surgical success.
Level of Evidence
4 Laryngoscope, 134:963–967, 2024
INTRODUCTION
The subglottis is the narrowest segment of the pediatric airway and the most susceptible to developing stenosis. Although a small percentage of subglottic stenosis (SGS) is congenital, the majority is acquired as a result of endotracheal intubation.1 Cases of pediatric SGS can develop after prolonged of brief intubation events.2 Despite an increased appreciation for the risks of intubation and selecting appropriately sized endotracheal tubes, SGS can still occur in young children.3
Double-staged laryngotracheoplasty (dsLTP) was initially described in 1974 by Fearon and Cotton as a solution to the presence of a long-term tracheostomy in patients with SGS.4 It is a staged open airway procedure using cartilage grafts to circumferentially expand the airway diameter. Costal cartilage is typically harvested, placed anteriorly and/or posteriorly, and supported by a suprastomal stent to facilitate healing. The tracheostomy remains present after surgery until airway caliber is deemed adequate. To date, dsLTP is commonly used in the treatment of SGS.
The goal of dsLTP is achieving a patent airway to facilitate decannulation. Because there are numerous elements that impact the success of dsLTP, determining factors that portend successful decannulation and counseling families about the likelihood of success can be challenging. The primary objective of this study was to determine how often initial postoperative airway endoscopy findings after stent removal predict the likelihood of decannulation. Secondary objectives assessed timing of decannulation and number of endoscopic interventions needed after pediatric dsLTP.
METHODS
A case series with retrospective chart review included consecutive dsLTP procedures at Children's Medical Center Dallas between 2008 and 2021. The University of Texas Southwestern Medical Center Institutional Review Board approved this study with exemption (IRB# 2019–1101). Exclusion criteria were patient age greater than 18 years, single-staged laryngotracheoplasty, endoscopic-only procedures, and resection with anastomosis procedures.
Patient characteristics recorded were age at surgery (years), gender (male or female), gestational age (months), ethnicity (Hispanic or not-Hispanic), and race (Asian, Black or African American, White, other). Preoperative risk factors identified were short gestational age (<37 weeks), neuromuscular disorder, hematologic disorder, baseline oxygen requirement, complex cardiac history, central nervous system abnormalities, reliance on gastrostomy tube nutrition, or developmental delay. These comorbidities were purposefully selected to align with data captured by the American College of Surgeons National Surgical Quality Improvement Program-Pediatric (ACS-NSQIP-P) database. This provides consistency for reporting across institutions and has been previously utilized for open airway outcomes. In addition, a positive methicillin-resistant staphylococcus aureus (MRSA) screen and diagnosis of gastroesophageal reflux disease (GERD) were determined as these have been found to affect outcomes in pediatric airway reconstruction.5, 6
Surgical data included presence of a preoperative tracheostomy, grade of stenosis at the time of surgery, preoperative vocal cord mobility, the location of the grafts placed (anterior, posterior, and both), and the size and type of suprastomal stent placed (Montgomery T-tube or Rutter stent). Grade of stenosis was defined by the Cotton-Myer grading scale.7 Grade I is defined as 0%–50% narrowing of the subglottic airway, grade II is 51%–70% narrowing, grade III is 71%–99% narrowing, and grade IV is assigned when there is no detectable lumen. Grades I and II were grouped as low-grade stenosis, and grades III and IV as high-grade stenosis.
Postoperative data included hospital length of stay (LOS), duration of stent placement (days), postoperative surgical-site infection (SSI), postoperative airway complications (pneumothorax, acute respiratory distress syndrome, and pneumonia), and readmission within 30 days.
A bronchoscopy is routinely performed 1–2 weeks after removal of the suprastomal stent. Subsequent operative reports were reviewed to determine grade of postoperative stenosis (first bronchoscopy after stent removal), time to tracheostomy decannulation (months), and number of endoscopic interventions required prior to decannulation. Endoscopic procedures included balloon dilations, application of steroids or mitomycin-C, scar division, and removal of granulation tissue. A revision airway reconstruction was not included as an intervention.
All statistics were performed with Stata (StataCorp. 2021. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC.). Continuous variables were presented as medians with interquartile ranges (IQR) and all comparisons of those continuous variables were performed using non-parametric Wilcoxon rank sum testing. Categorical variables were shown as counts with percentage along with Fisher's exact testing for significance. Log-rank testing was used to compare time with events between characteristic groups. Statistical significance was set at p < 0.05. This study adhered to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational studies.
RESULTS
A total of 65 children met inclusion criteria, and 48 (74%) were successfully decannulated after undergoing dsLTP. The mean age at reconstruction in children who were decannulated was 3.4 years (SD 1.5) compared with 5.7 years (SD 4.8) in children who were not decannulated (p = 0.06). Table I compares demographic characteristics based on decannulation status. No significant differences in sex, race, preoperative stenosis grade, preoperative tracheostomy status, and comorbidities were found between groups. Table II compares characteristics of children based on initial grade of postoperative stenosis. There was no difference in demographics, rate of GERD, MRSA, suprastomal stent type, and preoperative tracheostomy presence between those with low-grade and high-grade stenosis after dsLTP.
| Characteristic | Decannulated | Not decannulated | Total | p value |
|---|---|---|---|---|
| Total, no. (%) | 48 (74) | 17 (26) | 65 (100) | – |
| Age at reconstruction (y), mean (SD) | 3.4 (1.5) | 5.7 (4.8) | 4.0 (2.9) | 0.06 |
| Males, no. (%) | 26 (54) | 10 (59) | 36 (55) | 0.78 |
| Gestational age (wk), mean (SD) | 26.5 (3.2) | 27.2 (4.6) | 26.7 (3.6) | 0.50 |
| Race, no. (%) | ||||
| White | 22 (46) | 4 (24) | 26 (40) | 0.27 |
| Black or African American | 22 (46) | 10 (59) | 32 (49) | |
| Hispanic, no. (%) | 12 (26) | 2 (12) | 14 (22) | 0.32 |
| High-grade stenosis, no. (%) | 41 (85) | 16 (94) | 57 (88) | 0.67 |
| Preoperative tracheostomy, no. (%) | 48 (100) | 16 (94) | 64 (98) | 0.26 |
| MRSA, no. (%) | 12 (25) | 3 (18) | 15 (23) | 0.74 |
| GERD, no. (%) | 46 (96) | 15 (88) | 61 (94) | 0.28 |
- Abbreviations: GERD, gastroesophageal reflux disease; MRSA, methicillin-resistant Staphylococcus aureus; SD, standard deviation.
| Characteristic | Low-grade initially | High-grade initially | Total | p value |
|---|---|---|---|---|
| Total, no. (%) | 51 (78) | 14 (22) | 65 (100) | – |
| Age at reconstruction (y), mean (SD) | 3.8 (2.5) | 5.0 (4.1) | 4.0 (2.9) | 0.16 |
| Males, no. (%) | 27 (53) | 9 (64) | 36 (55) | 0.55 |
| Gestational age wk, mean (SD) | 26.8 (3.5) | 26.4 (4.2) | 26.7 (3.6) | 0.74 |
| Race, no. (%) | ||||
| White | 21 (41) | 5 (36) | 26 (40) | 0.79 |
| Black or African American | 25 (49) | 7 (50) | 32 (49) | |
| Hispanic, no. (%) | 10 (20) | 4 (29) | 14 (22) | 0.49 |
| High-s stenosis, no. (%) | 43 (84) | 14 (100) | 57 (88) | 0.19 |
| Preoperative tracheostomy, no. (%) | 51 (100) | 13 (93) | 64 (98) | 0.22 |
| MRSA, no. (%) | 12 (24) | 3 (21) | 15 (23) | 0.99 |
| GERD, no. (%) | 48 (94) | 13 (93) | 61 (94) | 0.99 |
| Stent type (%) | ||||
| Rutter | 23 (45) | 6 (43) | 29 (45) | 0.99 |
| Montgomery T-tube | 28 (55) | 8 (57) | 36 (55) | |
| Decannulated, no. (%) | 43 (84) | 5 (36) | 48 (74) | 0.001 |
| Total interventions needed, mean (SD) | 4.0 (3.0) | 7.5 (3.3) | 4.7 (3.4) | <0.001 |
| Time to decannulation (mo), mean (SD) | 17.8 (17.6) | 21.9 (17.7) | 18.3 (17.5) | 0.63 |
| Decannulation within 12 mo, no. (%) | 19 (44) | 2 (40) | 21 (44) | 0.99 |
- Abbreviations: GERD, gastroesophageal reflux disease; MRSA, methicillin-resistant Staphylococcus aureus; SD, standard deviation.
Of the 65 children included, 51 (78%) had low-grade stenosis and 14 (22%) had high-grade stenosis at their first bronchoscopy after dsLTP. Forty-three children (84%) with low-grade stenosis after dsLTP were successfully decannulated compared with five children (36%) with high-grade stenosis (p = 0.001). Time to decannulation was not significantly different between groups, with an overall mean time to decannulation of 18.3 months (SD 17.5, median 13.2 months, IQR 8.9–21.3).
The mean number of endoscopic interventions after dsLTP was 4.0 (SD 3.0) in the low-grade stenosis group compared with 7.5 (SD 3.3) in the high-grade stenosis group (p < 0.001). Among the decannulated children, those with low-grade stenosis needed 3.7 (SD 3.0) interventions, and those with high-grade stenosis needed 7.0 (SD 1.6) interventions (p = 0.02). In total, 5 (7.7%) children had an anterior graft, 3 (4.6%) had a posterior graft, and 57 (88%) had both an anterior graft and a posterior graft.
The duration of stent placement was not found to affect decannulation rates. Overall, 40 children (62%) had a stent in place for less than 3 weeks, and 30 (75%) of those were decannulated, whereas 25 children (38%) had a stent in place for longer than 3 weeks, of which 18 (72%) were decannulated (p = 0.78). Decannulation rates were similar between groups when stent duration was divided into <2, 2–4, and >4 weeks. Additionally, there was no difference in time to decannulation based on the duration of stent placement for the 48 children successfully decannulated.
Rutter stents were placed in 29 children (45%), and Montgomery T-tubes were placed in 36 children (55%). Stent size was reported for 52 children (80%) and ranged from 6 to 9 mm. Overall, 28 children (54%) had a 6 mm stent, 18 (35%) had a 7 mm stent, 5 (9.6%) had an 8 mm stent, and 1 (1.9%) had a 9 mm stent placed. Stent size distribution was evaluated and found to be similar between the children with Rutter stents and those with Montgomery T-tubes (p = 0.92).
Initial grade of stenosis after stent removal was not found to be different based on the type of stent used. Out of the children that had low-grade stenosis at initial bronchoscopy, 23 (45%) had a Rutter stent in place and 28 (55%) had a Montgomery T-tube (p = 0.99). Similarly, in children with high-grade stenosis at initial bronchoscopy 6 (43%) had a Rutter stent placed and 8 (57%) had a Montgomery stent placed (p = 0.99).
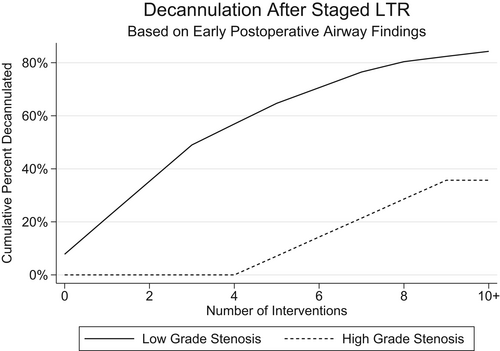
Figure 1 estimates the cumulative percent of decannulated children based on the number of interventions for low-grade and high-grade stenosis. For children with low-grade stenosis, the cumulative percent of decannulated children is approximately 50% when 3 to 4 interventions have been performed and increases to more than 80% when eight or more interventions are performed. The cumulative percent of decannulated children with high-grade stenosis only starts to increase when four or more interventions are performed. The percent of decannulated children with high-grade stenosis reaches approximately 40% after nine or more interventions have been performed.
DISCUSSION
DsLTP is a well-described procedure for the treatment of pediatric SGS. Based on the first bronchoscopy after stent removal, patients with low-grade stenosis had significantly higher rates of decannulation than those with high-grade stenosis. This was not affected by demographics, comorbidities, or preoperative stenosis grade. Time to decannulation was also similar between the two groups, despite the finding that patients with high-grade stenosis required significantly more endoscopic interventions to achieve decannulation. Although some of these findings may be intuitive, this is the first such study to try and quantify decannulation rates and time to decannulation based on the degree of stenosis after stent removal.
The decannulation rate after dsLTP in the literature ranges from 65% to 89%.8-13 In our study, the overall decannulation rate was 74% with a significantly higher rate in patients with low-grade stenosis after stent removal (84%) compared with those with high-grade stenosis after stent removal (36%). This suggests dsLTP is a frequently successful procedure for pediatric SGS with decannulation outcomes predicted by early endoscopy findings.
Endoscopic interventions such as balloon dilation, intraluminal administration of steroids or mitomycin-C, granulation tissue removal, or scar division are often performed after dsLTP. Endoscopic balloon dilation has been shown to be an effective adjunctive procedure following LTP.14 It is a safe and effective technique that allows maintenance of airway patency and improvement of airway caliber when scarring is observed postoperatively. Children in the low-grade stenosis group after dsLTP had about four endoscopic interventions prior to successful decannulation compared with seven interventions in the high-grade group. These findings are comparable with other studies in the literature. Koenigs et al. reported five endoscopic interventions prior to decannulation in 43.9% of their dsLTP population.11 Agrawal et al. reported 4.6 endoscopic procedures in their dsLTP patients and Khatib et al. noted 3.31 endoscopic procedures in patients decannulated compared with 1.29 in those not decannulated.9, 10 Our results indicate that children with high-grade stenosis postoperatively are likely to need more interventions prior to being successfully decannulated and emphasize the importance of postoperative endoscopic procedures in improving outcomes after dsLTP.9, 14, 15
Comorbidities and demographic factors were not found to be significantly associated with decannulation rate in children undergoing dsLTP. The presence of neurologic, cardiovascular, and pulmonary diseases did not reveal a correlation with tracheostomy decannulation. These results are consistent with findings in other studies.9, 11 Although children with significant comorbidities might be expected to remain tracheostomy-dependent longer, this has not been shown in the literature. One possible explanation is that most studies reporting open airway reconstruction results are limited to single-center experiences with small sample sizes unable to detect differences. In addition, there is patient selection bias as those with significant, neurologic, cardiovascular, or pulmonary disease are often considered poor candidates for this surgery.
The majority (88%) of the children in our sample had high-grade stenosis preoperatively. This was expected because only patients undergoing dsLTP, a procedure usually reserved for patients with higher grade stenosis, were included. The grade of stenosis at the first postoperative bronchoscopy after stent removal was grade I or II for 78% of the children, whereas 22% had grade III or IV stenosis at that time. Demographic characteristics, comorbidities, and presence of MRSA or GERD were not found to be different between the two groups. The type of stent used at the time of initial surgery was not found to affect stenosis grade at the initial postoperative bronchoscopy after stent removal. This suggests that surgical results after dsLTP might be independent of the suprastomal stent selected. The airway result and the propensity for scarring might instead be dependent on a patient's intrinsic healing factors, rather than the stent material used at reconstruction. Surgical and postoperative factors such as location of grafts and duration of stent placement also did not affect decannulation rate. This suggests that factors relating to postoperative results are multifactorial and include patient selection, choice of procedure, surgeon expertise, and patient-related considerations such as propensity for scarring and keloid formation.16
When assessing suprastomal stent duration, multiple timepoints were assessed. A stent duration more than 3 weeks did not impact decannulation outcomes compared with a duration of less than 3 weeks. Similarly, evaluation of 2- and 4-week timepoints did not make a significant difference in decannulation rate. This contrasts with previously published outcomes by Smith et al. in which stent placement was divided into short (21 days or less) and long terms (>21 days). Although that group found that time to decannulation was not affected by the duration of stent placement, they did find that children with long-term stents were 4.3 times more likely to get decannulated within a year after dsLTP.17 However, those findings could be partly explained by the increased use of intratracheal steroids in those with long-term stents, as well as location of graft placement.17 Further studies are required to adequately assess the effect of stent duration on postoperative decannulation rate, although controlling for variables such as comorbidities, postoperative medication administration, and location of graft placement.
In a landmark study by Hartnick et al.,15 it was stated “When faced with a family member who wants counsel as to what to expect as a result of an upcoming operation, the ability to predict the likelihood of success for that given procedure is important. It remains understood that each open surgical procedure will require several endoscopic evaluations and minor manipulations after the major procedure. Nevertheless, the ability to predict whether and how often subsequent major procedures will be required is a first step in the development of a disease-based, operation-specific predictive model.” In our study, patients with low-grade stenosis after stent removal were significantly more likely to be decannulated than those with high-grade stenosis. For those patients with high-grade stenosis who did achieve decannulation, they required significant more post-operative interventions than those with low-grade stenosis. These findings suggest that initial post-stent removal findings can help guide counseling and outcome prognostication with caregivers.
Time to decannulation was not found to be different between those with low-grade and high-grade postoperative stenosis. A mean time of 18 months to decannulation after dsLTP was identified, which is longer than previously reported in the literature. Koenigs et al. reported a median time to decannulation of 4 months with a range of 1–82 months,11 whereas Massie et al. reported a median time to decannulation of 7.7 months.13 This difference could be explained by variations in institutional protocols for decannulation, as well as surgeon preference on time to decannulation after dsLTP. Other barriers that could influence these findings include inconsistent patient follow-up and family preference. There are several factors that potentially prolong time to decannulation after pediatric airway reconstruction, and additional research should help further explore these associations.
There are a few key limitations to the findings from this study. The retrospective design introduces selection bias and the possibility for errors in documentation and missing information. These results also represent a single-center experience, which reflects the practices of the airway surgeons at this institution. Additionally, the rationale regarding graft placement, stent duration, and endoscopic intervention utilization is based on patient characteristics and surgeon preference, which might contribute to biases in the reported results. Despite these limitations, we believe our findings will be useful for pediatric airway surgeons when counseling caregivers. Future studies should be multi-institutional and attempt to standardize a postoperative decannulation protocol.
CONCLUSION
In this study of 65 children who underwent dsLTP, an overall decannulation rate of 74% was identified. Decannulation rate was not affected by patient demographics or surgical factors. Patients with low-grade stenosis on initial endoscopy after stent removal had significantly higher rates of decannulation and required significantly less postoperative interventions to achieve decannulation. These findings can guide surgeons in prognosticating surgical success, as well as in setting expectations when discussing outcomes with patient families.
CONFLICT OF INTEREST STATEMENT
Romaine F. Johnson is editor-in-chief of Laryngoscope Investigative Otolaryngology. He was not involved in the editorial evaluation of or decision to accept this article for publication. All other authors have no disclosures.




