Hearing Loss and Its Burden of Disease in a Large German Cohort—Hearing Loss in Germany
Editor's Note: This Manuscript was accepted for publication on December 02, 2021
The Gutenberg Health Study (GHS) is funded through the government of Rhineland-Palatinate (“Stiftung Rheinland-Pfalz für Innovation”, contract AZ 961-386261/733), the research programs “Wissen schafft Zukunft” and “Center for Translational Vascular Biology (CTVB)” of the Johannes Gutenberg-University of Mainz, and its contracts with Boehringer Ingelheim, and PHILIPS Medical Systems, including an unrestricted grant for the Gutenberg Health Study. p.s.w. is funded by the Federal Ministry of Education and Research (BMBF 01EO1503). p.s.w. and t.m. are PI of the German Center for Vascular Research (DZHK).
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Abstract
Objectives/Hypothesis
Hearing loss is the most common sensory impairment worldwide. It restricts patients in many aspects of their daily lives and can lead to social exclusion. Understanding this burden is a mandatory requirement for the care of those affected. Therefore, the aim of this study was to estimate the burden of hearing loss in a large German cohort.
Study Design
Cohort study.
Methods
The Gutenberg Health Study is designed as a single-center, prospective, and observational cohort study and representative for the city of Mainz, Germany, with its district. Participants were interviewed concerning common otologic symptoms and tested by pure-tone audiometry. The primary outcome was hearing impairment stratified by age and sex. The prevalence of tinnitus was estimated for a subcohort to calculate disability-adjusted life years (DALYs). All results were weighted by the European Standard Population (ESP) 2013.
Results
A total of 5,024 participants (mean age: 61.2 years, 2,591 men and 2,433 women) were included in the study. Hearing impairment showed the following prevalence: 28.2% (95% confidence interval [CI], 26.9%–29.4%) mild impairment, 10.1% (95% CI, 9.3%–11.0%) moderate impairment, 2.3% (95% CI, 1.9%–2.7%) moderately severe impairment, 0.2% (95% CI, 0.1%–0.4%) severe impairment, 0% (95% CI, 0.0%–0.1%) profound impairment, and 0.1% (95% CI, 0.0%–0.2%) complete impairment. Weighted for the ESP 2013 (all ages), hearing impairment across all levels (with/without tinnitus) causes a total of 2,118.97 DALYs per 100,000.
Conclusion
With 40.9% affected, the hearing loss represents a relevant burden of the German population. Understanding this will provide the basis for future guidelines on how to care for these patients.
Level of Evidence
2 Laryngoscope, 132:1843–1849, 2022
INTRODUCTION
Hearing loss affects around 466 million people worldwide.1 Given current demographic changes and rising life expectancy, the prevalence of hearing loss is presumed to be constantly increasing. The World Health Organization (WHO) predicts that by 2050, more than 900 million people worldwide will suffer from hearing impairment.1
At the patient level, hearing loss depicts a huge infringement in a patient's social well-being.2 Lacking the ability to communicate with others inevitably leads to social marginalization and a loss of productivity. Due to the fact that hearing loss usually develops slowly over time, it often goes unnoticed for quite a while and patients remain untreated.3 With this in mind, we must assume that hearing impairment contributes significantly to the overall disease burden worldwide.
The Global Burden of Disease (GBD) project is a quantitative assessment to estimate the GBD.4 They introduced the disability-adjusted life year (DALY) as a health metric.5 It measures the gap between a disease state and the hypothetical state of perfect health by combining morbidity and mortality into one measure. Here, morbidity is expressed as “years lived with disability” (YLD) and is represented by the product of the duration (D) of a disease and the disability weight (DW) assigned to it. Mortality, on the other hand, is calculated by subtracting the age at premature death from a standard life expectancy (life expectancy − age at death). Thus, at the individual level, DALY = YLD + years of life lost (YLL). As a measure of population, YLD and YLL must be multiplied by the incidence of a disease. Although incidence used to be the measure of choice, prevalence is more commonly used in epidemiological studies.6
DW is a weighting factor that expresses the severity of a disease state within a continuum between 0 (perfect health) and 1 (equivalent to death). The GBD study distinguishes between hearing loss with and without ringing. DW for hearing loss range from 0.010 for mild hearing loss to 0.316 for complete hearing loss with ringing (see Table I).7 They are thus rated as more disabling than visual impairments (from 0.003 for mild impairment (distance vision) to 0.187 for blindness).8
| Disability Weight (2013) | |
|---|---|
| Hearing loss: mild | 0.010 |
| Hearing loss: moderate | 0.027 |
| Hearing loss: moderately severe | 0.092 |
| Hearing loss: severe | 0.158 |
| Hearing loss: profound | 0.204 |
| Hearing loss: complete | 0.215 |
| Hearing loss: mild, with ringing | 0.021 |
| Hearing loss: moderate, with ringing | 0.074 |
| Hearing loss: moderately severe, with ringing | 0.167 |
| Hearing loss: severe, with ringing | 0.261 |
| Hearing loss: profound, with ringing | 0.277 |
| Hearing loss: complete, with ringing | 0.316 |
The recent GBD study stated that 4.63% of all years lived with disability (YLD) was caused by hearing impairment.9 In comparison to 2007, this burden has increased by 22.4%. Hereby, hearing loss is the most prevalent sensory impairment and should be given high priority in its treatment. This is especially true for high-income countries, as they have the highest prevalence of hearing loss (moderate or higher grade) at 7.5%.10 However, to reduce this burden of disease, we need to better understand its occurrence at the national and subnational levels.
Although hearing loss is the most common sensory impairment, population-based national studies are still sparse. A comprehensive review from 2009 found only six studies reporting hearing loss applicable to the European region.11 None of these studies were from Germany, even though Germany accounts for more than one-tenth of the European population. The WHO Programme for the Prevention of Blindness and Deafness and Hearing Impairment initiated a central database for hearing impairment. They stated important criteria for studies to be eligible: Studies must have a randomly selected sample, they must be population based, and they must be representative for a country or a subregion.11 Furthermore, to make results comparable, studies must report standardized outcome measures.
Roth et al. recommended using the WHO classification for this purpose.12 But the earlier WHO classification of hearing impairment was recently revised by the GBD Hearing Loss Expert Group.7, 13 They proposed lowering the normal hearing threshold to 20 decibels (dB) and gave six categories of hearing impairment, differentiated by 15 dB increments. This choice represents the minimum difference in pure-tone audiometry that is considered clinically significant.14 The WHO adapted to this grading of hearing impairment in their recently published World Report on Hearing.10 In addition, the GBD 2019 Hearing Loss Collaborators distinguish two types of health conditions: Hearing loss with and without ear ringing (tinnitus).7
This study aims to report on the prevalence of hearing impairment and its burden of disease in a large, population-based, randomly selected cohort study. It is the largest study in Germany thus far as known to the authors.
MATERIAL AND METHODS
The Gutenberg Health Study (GHS) is a large, ongoing population-based study and designed as a single-center, observational, prospective cohort study. It was initiated in 2007 at Mainz University Hospital, Germany, and planned to cover the population of the city of Mainz and its district of Mainz-Bingen, Germany. It was approved by the institutional review board (Ethics Commission of the State Chamber of Physicians of Rhineland-Palatine, reference no. 837.020.07). In accordance with the Declaration of Helsinki, written informed consent was obtained from all subjects before participation in the study. The population sample was randomly drawn from the local residents' registration office and stratified by sex and residence (rural vs. urban) for each age decade. Exclusion criteria were physical and mental disabilities that might prevent the participant from attending the study site. Furthermore, residents with insufficient knowledge of the German language were also excluded. In 2017 (10-year follow-up [10-FU], from 2017 to 2020), comprehensive otologic examinations were included in the broad and interdisciplinary examination battery. A detailed description of the study design has been published elsewhere.15
The validity of the audiologic examinations was ensured by implementing a standard operating procedure. All study contacts and examinations of participants took place in the premises of the University Hospital Mainz. The study nurses were trained and continuously educated by certified audiology assistants from the university's Department of Otorhinolaryngology.
After going through an interview concerning common otologic symptoms (i.e., tinnitus), pure-tone audiometry for air and bone conduction was tested separately for both ears at the following frequencies: 0.125, 0.25, 0.5, 0.75, 1, 2, 3, 4, 6, 8 and 10 kHz. All tests were performed with the Auritec® AT1000 clinical audiometer and in a soundproof booth.
Participants with missing data in the frequency 0.5, 1, 2, or 4 kHz were excluded from the study. In addition to that, participants with missing data for tinnitus were excluded from the subcohort.

We assumed YLL to be zero for hearing impairment. This is in accordance with prior literature.7, 17 Hence, with YLL = 0, YLD = DALY. For this, we used the most recent DWs for hearing loss as published in 2021 (Table I).7 DALYs for hearing loss with and without tinnitus were calculated separately by multiplying prevalence by DW.
The results were weighted to a reference population (ESP 2013) and reported as a prevalence of 100,000.18 The ESP is an age-standardized population based on the average population of all 27 Member States of the European Union plus the 4 European Free Trade Association countries. It was first reported in 1976 and revised in 2013. It is intended to facilitate the reporting of population-based indices by minimizing errors that occur when reporting crude rates.
Because no one in the study population was below 25 years or older than 86 years, the calculated weighted prevalences only apply to the subsection of the reference population in this age range and not to the whole reference population. Furthermore, for some reference populations, the oldest age groups (given in the form of “≥85” or “85–95” and thus) do not overlap neatly with our age groups, so that the exclusion of the oldest participants in the sample yields more unbiased estimates for the remaining age range. We will, however, also report estimates using all study participants both for completeness and because hearing loss increases with age so that data on the later age brackets are particularly valuable and should not be discarded. All statistical analyses were performed using R version 3.6.1 (2019-07-05).
RESULTS
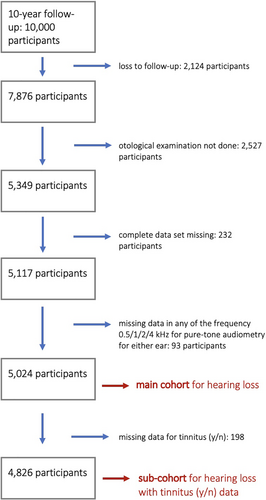
For the 10-FU, 10,000 participants were invited to visit the study site for their follow-up examination. See Figure 1 for the selection process of the study population. Complete data on pure-tone audiometry were available for 5,024 participants (main cohort). Of these, 198 participants were missing data for tinnitus (y/n) and were therefore excluded. The subcohort thus comprised 4,826 participants. See Table II for demographics.
| All (n) | Male (n) | Female (n) | P Value | |
|---|---|---|---|---|
| Main cohort | 5,024 | 2,591 | 2,433 | .026* |
| Average age (yr) | 61.2 | 61.9 | 60.4 | <.0001* |
| Age group | ||||
| 25–34 | 211 | 102 | 109 | .63 |
| 35–44 | 353 | 167 | 186 | .31 |
| 45–54 | 988 | 469 | 519 | .11 |
| 55–64 | 1,280 | 653 | 627 | .47 |
| 65–74 | 1,204 | 636 | 568 | .050 |
| 75–89 | 988 | 564 | 424 | <.0001* |
- * Values represent significance with P < .05.
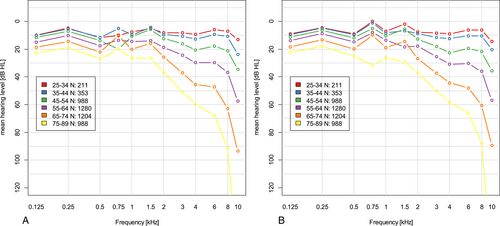
Within the GHS cohort, the overall prevalence of hearing loss across all levels of impairment was 40.9% (2,054/5,024) in the main cohort. Moderate to complete hearing loss (35 dB+) showed a prevalence of 12.7% (95% confidence interval [CI], 11.8%, 13.7%) with 15.0% in males and 10.3% in females. Hearing impairment was divided among degrees of impairment as follows: 68.9% of the cohort showed mild impairment, 24.7% moderate impairment, 5.6% moderately severe impairment, 0.6% severe impairment, 0.1% profound impairment, and 0.2% showed complete impairment. See Table III for the full results. From a frequency of 2 kHz upward, the mean hearing level decreased with age (Fig. 2).
| All (95% CI) | Male (95% CI) | Female (95% CI) | P Value | |
|---|---|---|---|---|
| n | 5,024 | 2,591 | 2,433 | .026* |
| Hearing impairment in dB (mean of 0.5/1/2/4 kHz) | ||||
| Left ear | 18.75 (18.50, 18.75) | 20.25 (20.00, 21.25) | 17.25 (16.25, 17.50) | <.0001* |
| Right ear | 18.75 (18.50, 18.75) | 20.00 (19.00, 20.25) | 17.50 (16.25, 17.50) | <.0001* |
| Minimum (of both ears) | 16.25 (16.25, 17.50) | 17.75 (17.50, 18.75) | 15.00 (15.00, 16.25) | <.0001* |
| Hearing impairment according to WHO† | ||||
| No impairment | 59.1% (57.7%, 60.5%) | 54.4% (52.5%, 56.4%) | 64.1% (62.2%, 66.0%) | <.0001 |
| Mild impairment | 28.2% (26.9%, 29.4%) | 30.6% (28.8%, 32.4%) | 25.6% (23.9%, 27.4%) | .00011 |
| Moderate impairment | 10.1% (9.27%, 11.0%) | 11.5% (10.3%, 12.8%) | 8.55% (7.47%, 9.73%) | .00052 |
| Moderately severe; impairment | 2.27% (1.88%, 2.72%) | 3.05% (2.42%, 3.79%) | 1.44% (1.00%, 2.00%) | .00019 |
| Severe impairment | 0.239% (0.123%, 0.417%) | 0.232% (0.085%, 0.503%) | 0.247% (0.091%, 0.536%) | 1.00 |
| Profound impairment | 0.020% (0.0005%, 0.111%) | 0.039% (0.001%, 0.215%) | 0% (0%, 0.152%) | 1.00 |
| Complete impairment | 0.100% (0.032%, 0.232%) | 0.154% (0.042%, 0.395%) | 0.041% (0.001%, 0.229%) | .41 |
- * values represent significance with P < .05.
- † Audiometric value (average across 0.5/1/2/4 kHz).
- CI = confidence interval; WHO = World Health Organization.
Generalizing these results weighted for the ESP of 2013 (all ages), the overall prevalence of hearing loss across all levels of impairment is assumed to be 26.9% (for males: 29.0%, for females: 24.8%). Moderate to complete hearing loss (35 dB+) has a prevalence of 7.9% (95% CI [7.2%, 8.7%]) with 9.1% for males and 6.8% for females. If only the age groups below 85 years are included, the overall prevalence of hearing loss across all levels of impairment is assumed to be 25.5% (for males: 27.5%, for females: 23.5%). Moderate to complete hearing loss (35 dB+) shows then a prevalence of 7.5% (95% CI [6.7%, 8.2%]) with 8.3% for males and 6.6% for females. See Table IV for the distribution among the different levels of hearing impairment.
| EU Standard Population 2013 (95% CI) | EU Standard Population 2013, Only <85 yr (95% CI) | |
|---|---|---|
| Mild impairment | 19.0% (17.9%, 20.1%) | 18.0% (17.0%, 19.1%) |
| Moderate impairment | 6.1% (5.5%, 6.8%) | 5.9% (5.2%, 6.6%) |
| Moderately severe impairment | 1.6% (1.3%, 2.0%) | 1.4% (1.1%, 1.8%) |
| Severe impairment | 0.1% (0.1%, 0.3%) | 0.1% (0.1%, 0.3%) |
| Profound impairment | 0.0% (0.0%, 0.1%) | 0.0% (0.0%, 0.1%) |
| Complete impairment | 0.1% (0.0%, 8.7%) | 0.1% (0.0%, 0.2%) |
- CI = confidence interval; WHO = World Health Organization.
Within the subcohort, the prevalence of hearing loss across all levels of hearing impairment was 39.9% (1,925/4,826). Overall, 25.5% (1,230/4,826) reported of having experienced a tinnitus. Of those who reported having a tinnitus, 607 (49.3%) participants also suffered from hearing loss, while 623 (50.7%) participants had no hearing loss.
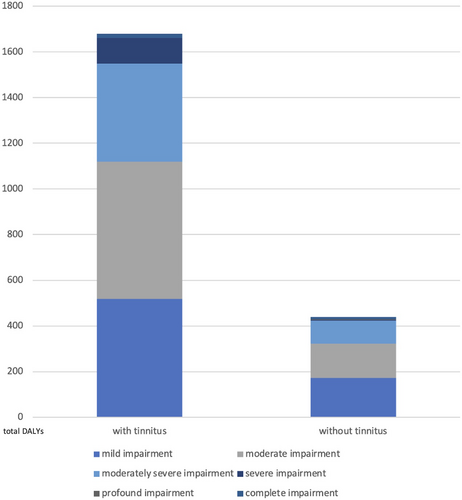
Around 53.377 DALYs were accumulated by hearing loss across all grades of impairment. Of these, 28.859 DALYs were caused by hearing loss with tinnitus and 24.518 by hearing loss without tinnitus. The majority of all DALYs was caused by mild to moderately severe hearing loss. Within this group, hearing loss with tinnitus was the major contributor. Weighted for the ESP 2013 (all ages), we can assume that hearing impairment across all levels (with and without tinnitus) causes a total of 2,118.97 DALYs per 100,000 population. Figure 3 shows the results divided by grade of hearing impairment and with or without tinnitus. Summarizing DALYs across all grades of hearing impairment for participants with and without tinnitus shows that hearing impairment with tinnitus causes 79.3% of the overall burden of hearing loss (without tinnitus: 20.7%).
DISCUSSION
The recent World Report on Hearing by the WHO placed hearing loss as a major contributor to all disabilities worldwide at the top of the agenda.10 This study fills a gap in data on hearing loss by reporting the prevalence of hearing loss in a large German cohort study including stratification by age and presence of tinnitus.
Due to the fact that hearing loss often develops slowly, especially at a mild level of impairment, patients might not be aware of their disability. Therefore, self-report of hearing impairment may not be sufficient to detect hearing loss.19 The strength of this study can hence be seen in the procedure of testing by pure-tone audiometry in a soundproof booth, as described above. Furthermore, the cohort is based on a randomly selected population-based sample representative for the subregion of Mainz-Bingen and can therefore be generalized to greater regions considering the limitations described below.
The study cohort is composed of residents of the city of Mainz and the district of Mainz-Bingen. This ensures a combination of urban and rural residents, although the city and district are geographically very close to each other. Since both are located in a highly industrialized and also densely populated region of Rhineland-Palatinate, we do not assume a difference in urban and rural participants. Due to the central location of the region, we assume that it is similar to the rest of the country and thus representative of the population of Germany. However, it should be noted that Mainz and its surrounding area are in close proximity to Frankfurt International Airport. Since environmental noise can be a cause of acquired hearing loss, this fact must be taken into account, especially when considering the relatively high prevalence of hearing impairment in our cohort (see also below).20
The main finding of this study was an overall prevalence of hearing impairment across all levels of 40.9%. Moderate to complete hearing loss (35 dB+) accounted for a prevalence of 12.7%. Löhler et al. conducted a recent review of studies reporting upon the prevalence of hearing impairment in Germany.21 Only one study (HÖRSTAT study) provided data for a randomized sample of adults based on data from pure-tone audiometry. The HÖRSTAT study included a total of 1,866 participants from two cities in Lower Saxony. They found a prevalence of hearing impairment of approximately 15.7% according to the previous WHO definition with a mean pure-tone audiometric value (0.5/1/2/4 kHz) of 25 dB or more.22 One of their limitations laid in different study settings. About 8% of participants were tested at their homes without a soundproof booth. Other European studies reported a prevalence of hearing impairment ranging from 16.1% to 18.8% in the adult population.23-26 They also defined hearing impairment with a pure-tone audiometric average (0.5/1/2/4 kHz) of 25 dB or greater. Our result of 12.7% for moderate to complete hearing loss is defined as a pure-tone audiometric average (0.5/1/2/4 kHz) of 35 dB or more. This higher threshold is probably the reason for a lower prevalence number. To compensate for the different definitions of the hearing impairment threshold, we aimed to provide our data as granularly as possible and for all levels of hearing impairment separately following the revised grading by the WHO.
When weighting the study results to the ESP of 2013, we can assume a prevalence for hearing impairment in Europe (for ages between 25 and 86 years) across all grades of 26.9%. This prevalence is higher than the recently reported GBD 2019 prevalence of 14.1% for all hearing loss in Europe.7 Although the overall distribution between the different degrees of impairment was similar, the prevalence of mild to severe hearing impairment was higher in our study cohort than in the GBD 2019 results (20.3%).
This difference can be attributed to the fact that the GBD study includes children from early neonatal age. Children have the lowest prevalence, whereas hearing loss is more common at older ages, especially 50 years and older. In contrast to this age structure, our cohort excludes children and shows an age structure with a mean of 61.2 years. Males showed a higher prevalence of hearing impairment than females. This is consistent with the results of the GBD study 2019.
The cumulative result of 2,119.0 DALYs per 100,000 population provides another form of representation to make the results more comparable across health states and environments as well. Thus, the burden of hearing loss in our cohort is comparable to the burden of blindness and vision impairment in Brazil, which ranges from 1,009.9 to 3,210.2 DALYs per 100,000 population, depending on age group.27 Further studies examining the burden of diseases for other conditions within the GHS cohort are needed to better understand how hearing loss contributes to the overall burden of disease in the Mainz-Bingen region.
This study contains a couple of limitations, which we will reflect upon in the following. First, the GHS is designed as a population-based cohort study and by its design is representative of the population of Mainz-Bingen, Germany.15 As mentioned above, Mainz and its district are located in a highly industrialized region near an international airport. Therefore, the study participants might be more exposed to environmental noise than residents of other regions in Germany. In addition, demographic change in Germany results in an aging population compared to other European countries.28 Because average hearing levels decreased with age, the age structure of our study may overestimate the prevalence of hearing impairment in countries with a younger adult population. Generalization of the results beyond Europe will be difficult because of even greater variation in living conditions and demographics. These limitations must be kept in mind when interpreting our results.
The otologic examination was included in the course of the study and conducted for the first time at the 10-FU examination. Around 21.2% of the initial baseline cohort was lost to follow-up. Even though interviews with nonresponders were included in the baseline examination, this was not performed during 10-FU. Therefore, the extent to which nonresponders and responders differed at 10-FU remains unknown. This creates a certain selection bias of unknown magnitude. Furthermore, an additional 2,527 participants were excluded due to a missing otologic examination. This was mostly due to study staff absences due to illness. We assume that the bias caused by this is random. Hence, the prevalence results from the GHS population (main cohort) should be considered the primary outcome of this study. Assumptions based on the weighting of these results to the ESP 2013 should only be interpreted under these limitations.
Higher-ranking exclusion criteria for the GHS study were physical and mental disabilities that might prevent the participant from visiting the study site. It is known that the prevalence of hearing loss is greater in people with comorbidities such as diabetes or cardiovascular disease.29 Excluding these participants from a study might lead to an underestimation of the prevalence of hearing loss.
In addition, the ESP 2013 does not subdivide into age groups of 85 years or older. With the aging of the population kept in mind, this includes a significant population over 87 years of age. In our sample, 100% of the participants were under 87 years of age. Removing this final age category of 85+ gives a more unbiased result that accounts only for those under 85 years. We report both versions in the Results section.
Furthermore, we did not consider the quality of the tinnitus (ringing, roaring, and buzzing) or time aspects (i.e., once a month) when asking about the occurrence of tinnitus. Therefore, we were not congruent with the National Health and Nutrition Examination Survey and thus the basis of tinnitus modeling in the GBD 2019 study.30
Finally, we did not survey individual causes of hearing loss (i.e., infection or surgery) and cannot attribute the hearing loss to its etiology.
Despite these limitations, the strength of this study lies in the clinical rigor of examining all participants by pure-tone audiometry in a sound-proof booth and adhering to the standards of the university's Department of Otorhinolaryngology. With this design, it provides data from the largest cohort of adults in Germany known to the authors to date.
CONCLUSION
Our study showed a prevalence of moderate to complete hearing loss (35 dB+) of 12.7%. Considering all levels of impairment, mild hearing impairment represented the majority of all participants affected. With mild hearing impairment, individuals may not yet experience functional limitations, but require close monitoring and regular re-testing.
Understanding the burden of hearing loss in the German population will provide the basis for future guidelines on how to care for these patients. To facilitate this care, future studies on care provision (i.e., hearing aids) are needed to understand the unmet need resulting from this burden of disease.